Nearly 900,000 Americans face blood clots each year. Many cases are linked to health conditions.
Different diseases and factors raise the risk of blood clots. These include heart diseases, cancer, and autoimmune disorders.
It’s important to know these risks. This helps in preventing and treating blood clots early. If not, they can be deadly.
Key Takeaways
- Certain diseases increase the risk of blood clots.
- Cardiovascular diseases are a major risk factor.
- Cancer and autoimmune disorders also play a role.
- Early intervention is key to prevent complications.
- Understanding risk factors helps in prevention.
Understanding Blood Clots: The Basics
Blood clots are a complex part of our body’s response to injury. They play a key role in preventing too much bleeding. We will look at the basics of blood clots, including how they form and the risks of clotting disorders.
What Are Blood Clots?
Blood clots are clumps of blood that form in response to injury. They are made up of blood cells, platelets, and proteins. These components work together to stop bleeding. Blood clot formation is essential for healing and recovery from injuries.
Normal Blood Clotting Process
The blood clotting process involves several steps. It starts with an injury that damages a blood vessel. This injury exposes the tissue underneath.
The body responds by activating platelets and releasing chemical signals. These signals attract more platelets and cells, forming a clot.
The clotting process has three main stages:
- Platelet activation and aggregation
- Coagulation cascade, involving various clotting factors
- Fibrin formation, which stabilizes the clot
When Clotting Becomes Dangerous
Blood clotting is vital but can be dangerous if it happens too much. Thrombosis is when blood clots form inside a blood vessel. This can block blood flow and cause serious health problems like heart attack, stroke, and deep vein thrombosis.
It’s important to understand the risks of blood clots. This helps us identify who is at risk and take steps to prevent it. We will explore the causes and risk factors of blood clotting disorders next.
What Causes Blood Clots: The Underlying Mechanisms

It’s important to know what causes blood clots to prevent and treat them. Blood clots form through a complex process involving many factors and pathways.
Virchow’s Triad: The Three Factors
Virchow’s Triad helps us understand blood clot causes. It points out three main factors: hypercoagulability, blood vessel damage, and blood stasis. These factors work together and can greatly increase clot risk.
Hypercoagulability Explained
Hypercoagulability means the blood clots more easily. It can be due to genetics, cancer, or some medicines. Even small injuries or blood flow changes can cause clots when the blood clots more easily.
Key factors contributing to hypercoagulability include:
- Genetic disorders, such as Factor V Leiden mutation
- Cancer and its treatment
- Hormonal changes, such as those occurring during pregnancy or with the use of hormonal contraceptives
Blood Vessel Damage and Clotting
Damage to blood vessel walls is key in clotting. When the lining of a blood vessel gets hurt, it starts the clotting process. This damage can come from trauma, infection, or inflammation.
The role of blood vessel damage in clotting highlights the importance of maintaining vascular health.
Blood Stasis and Flow Problems
Blood stasis, or slow blood flow, is the third part of Virchow’s Triad. It can happen from not moving enough, heart problems, or blood vessel compression. When blood flow slows, clotting factors build up, making clots more likely.
Knowing these causes is key to spotting risk and preventing clots. By understanding what leads to blood clots, we can lower the risk of these dangerous events.
Inherited Blood Clotting Disorders
Inherited blood clotting disorders are genetic conditions that affect how blood clots. They can lead to serious health issues. These disorders increase the risk of blood clots, which can be deadly if not managed well.
We will look at several key inherited conditions that lead to blood clotting disorders. Knowing about these conditions is key for early diagnosis and effective management.
Factor V Leiden Mutation
The Factor V Leiden mutation is a common inherited blood clotting disorder. It’s caused by a mutation in the factor V gene. This mutation makes it hard for protein C to inactivate factor V, raising the risk of venous thromboembolism.
Key aspects of Factor V Leiden mutation include:
- Increased risk of deep vein thrombosis (DVT)
- Higher risk of pulmonary embolism
- Often asymptomatic until a clotting event occurs
Prothrombin Gene Mutation
The prothrombin gene mutation, G20210A, causes high levels of prothrombin. This increases the risk of venous thrombosis.
Important facts about prothrombin gene mutation:
- Associated with an increased risk of DVT and pulmonary embolism
- Can be detected through genetic testing
- Management involves anticoagulant therapy
Protein C and Protein S Deficiencies
Protein C and protein S are natural anticoagulants. They help regulate blood clotting. Deficiencies in these proteins increase the risk of thrombosis.
| Deficiency | Effect on Clotting | Management |
| Protein C Deficiency | Increased risk of venous thrombosis | Anticoagulant therapy |
| Protein S Deficiency | Increased risk of venous thrombosis | Anticoagulant therapy |
Antithrombin Deficiency
Antithrombin is a protein that stops several clotting factors. A deficiency in antithrombin greatly increases the risk of blood clots.
Key features of antithrombin deficiency:
- High risk of venous thromboembolism
- Often requires lifelong anticoagulation
- Can be managed with antithrombin concentrate in some cases
Understanding these inherited blood clotting disorders is key for identifying at-risk individuals. Early diagnosis and treatment can greatly reduce the risk of complications.
Acquired Blood Clotting Disorders
Acquired blood clotting disorders can start for many reasons. These include autoimmune responses and side effects from medicines. Knowing what causes these conditions and how they show up is key to managing the risk of blood clots.
Antiphospholipid Syndrome
Antiphospholipid syndrome (APS) is an autoimmune disease. It happens when the body makes antibodies against phospholipids. This can cause blood clots in veins or arteries.
APS can happen alone or with other autoimmune diseases like systemic lupus erythematosus.
Key Features of Antiphospholipid Syndrome:
- Presence of antiphospholipid antibodies
- History of thrombosis or pregnancy morbidity
- Variable clinical manifestations, including cardiovascular and neurological symptoms
Heparin-Induced Thrombocytopenia
Heparin-induced thrombocytopenia (HIT) is a serious side effect of heparin. It happens when the body makes antibodies against heparin-PF4 complexes. This can cause low platelet counts and increase the risk of blood clots.
| Characteristics | HIT |
| Platelet Count | Typically decreased |
| Thrombotic Risk | Increased |
| Antibody Presence | Anti-heparin-PF4 antibodies |
Disseminated Intravascular Coagulation (DIC)
Disseminated intravascular coagulation (DIC) is a complex condition. It involves widespread clotting and bleeding in the blood vessels. It often comes with severe conditions like sepsis or cancer.
Clinical Features of DIC:
- Prolonged clotting times
- Low platelet count
- Elevated D-dimer levels
- Variable clinical presentation, ranging from asymptomatic to severe bleeding or thrombosis
Thrombotic Thrombocytopenic Purpura
Thrombotic thrombocytopenic purpura (TTP) is a rare disorder. It involves blood clots in small blood vessels all over the body. It’s often linked to a lack of ADAMTS13, a metalloprotease enzyme.
Management of TTP:
- Plasma exchange therapy
- Immunosuppressive therapy in some cases
- Supportive care to manage complications
Cardiovascular Diseases and Blood Clots
It’s important to know how cardiovascular diseases and blood clots are connected. These diseases affect the heart and blood vessels. They can make it more likely for blood clots to form.
Atrial Fibrillation and Stroke Risk
Atrial fibrillation is a heart rhythm problem that raises stroke risk. It happens when the heart’s upper chambers beat irregularly. This can cause blood to pool and clot. Anticoagulant medications help lower this risk.
Heart Failure and Venous Stasis
Heart failure can cause blood to move more slowly in veins. This is called venous stasis. It increases the chance of blood clots forming, like deep vein thrombosis (DVT). Managing heart failure well is key to avoiding blood clots.
Atherosclerosis and Arterial Clots
Atherosclerosis is when plaque builds up in arteries. This can cause arterial clots. These clots can lead to heart attacks or strokes. Controlling risk factors like high blood pressure and high cholesterol is important.
Peripheral Artery Disease
Peripheral artery disease (PAD) is when arteries narrow due to plaque buildup. It raises the risk of arterial clots. PAD can cause limb ischemia and increase the risk of heart problems. Lifestyle changes and medical care are important for managing PAD and clot risk.
Cardiovascular diseases are complex and linked to blood clots. Understanding these conditions helps us prevent and treat blood clots.
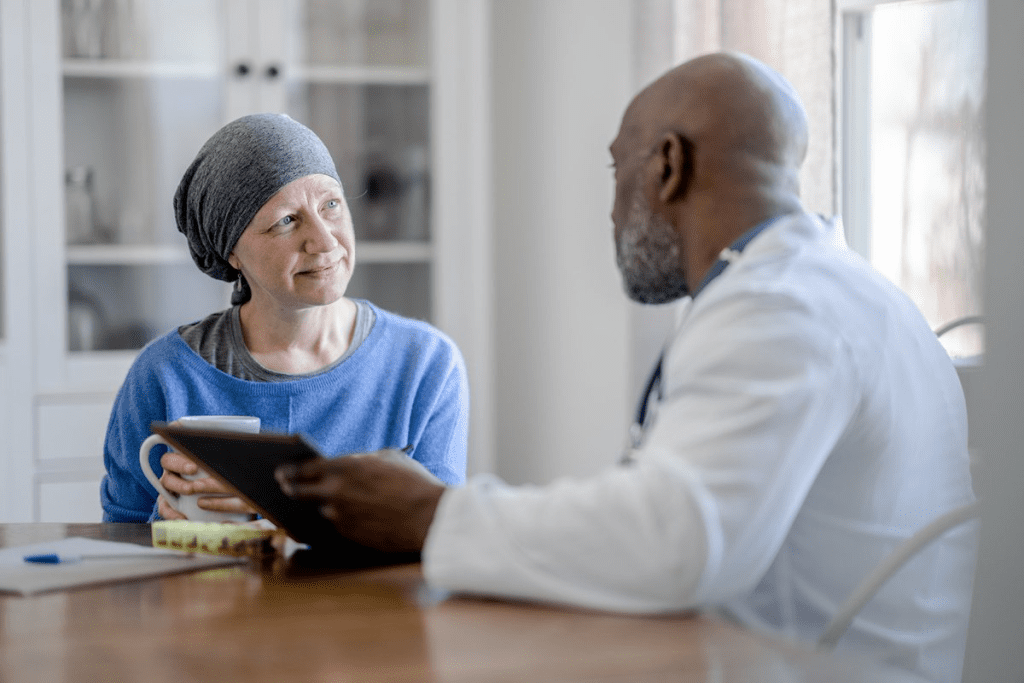
Cancer and Blood Clotting Disorders
The link between cancer and blood clotting disorders is a big worry for both patients and doctors. Cancer and its treatments can make blood clots more likely. This can lead to serious problems. It’s key to understand this to care for cancer patients fully.
How Cancer Increases Clotting Risk
Cancer can make blood clots more likely in several ways. Tumor cells can release substances that help clots form. Also, the inflammation from cancer can make the body more prone to clotting. Treatments like surgery, chemotherapy, and hormone therapy can also raise this risk.
Types of Cancer Most Associated with Clots
Some cancers are more likely to cause blood clots. These include pancreatic, brain, ovarian, and lung cancers. The risk is higher for patients with advanced or spread-out cancer.
Cancer Treatments and Blood Clots
Cancer treatments can also increase the risk of blood clots. Surgery, for example, can cause prolonged sitting, which is a clot risk factor. Chemotherapy and hormone therapy can also affect how blood clots. So, it’s important to take preventive steps.
Trousseau Syndrome
Trousseau syndrome, or malignancy-associated thrombosis, is when cancer causes recurring or moving blood clots in veins. This shows how complex the relationship between cancer and clotting disorders is. It stresses the need for careful monitoring.
Autoimmune Diseases and Blood Clots
Autoimmune diseases can raise the risk of blood clots. This is because of chronic inflammation and a messed-up immune system. These conditions make the body attack itself, changing how it clots blood.
“The presence of autoimmune diseases complicates the management of blood clots, as the underlying inflammatory process can affect the efficacy of anticoagulant therapies,” says a recent study on the topic. Recognizing the risks associated with autoimmune diseases is key to finding good treatments.
Lupus and Blood Clots
Systemic Lupus Erythematosus (SLE) is an autoimmune disease that ups the risk of blood clots. SLE patients often have antibodies that make blood clotting worse. We must take these risks into account when treating lupus patients.
Rheumatoid Arthritis
Rheumatoid Arthritis (RA) is linked to a higher risk of heart problems, including blood clots. The ongoing inflammation in RA can cause arteries to narrow, leading to clots.
Some RA treatments, like corticosteroids, can also affect clotting risks. We must weigh the good and bad of these treatments carefully.
Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD), like Crohn’s and ulcerative colitis, raises the risk of blood clots. The ongoing inflammation and possible lack of nutrients play a part in this risk.
Dealing with IBD means watching for clotting risks and taking steps to prevent them when needed.
Behçet’s Disease
Behçet’s disease is a rare autoimmune disorder that causes blood vessel inflammation. It can lead to both artery and vein clots.
Managing Behçet’s disease involves controlling inflammation and preventing blood clots. We need to customize our treatments to meet these needs.
In conclusion, autoimmune diseases make managing blood clots very challenging. By knowing the specific risks of each disease, we can create better strategies to prevent and treat blood clots.
Hormonal Influences on Blood Clotting
It’s important to know how hormones affect blood clotting. Hormonal shifts can change how blood clots, leading to health problems.
Pregnancy and Postpartum Period
Pregnancy makes blood more likely to clot. This is because of higher clotting factors and less anticoagulants. It helps prevent bleeding during birth but raises the risk of blood clots.
The risk of blood clots doesn’t go away after birth. It’s important to watch for signs and sometimes use blood thinners.
Hormonal Contraceptives and Estrogen
Hormonal birth control, with estrogen, can increase blood clot risk. Estrogen affects clotting factors, making blood more prone to clots. The risk depends on the type of birth control, with some being safer than others.
Hormone Replacement Therapy
Hormone therapy helps with menopause symptoms. But, it can raise the risk of blood clots, more so with estrogen. Oral hormone therapy is riskier than patches or gels.
Polycystic Ovary Syndrome
PCOS is linked to insulin resistance, obesity, and heart disease risk. It doesn’t directly cause blood clots. But, the hormonal and metabolic issues can make blood clotting more likely.
| Hormonal Condition | Effect on Blood Clotting | Risk Management |
| Pregnancy | Increased clotting factors | Monitoring, prophylactic anticoagulation |
| Hormonal Contraceptives | Estrogen increases clotting risk | Choose progestin-only methods if at risk |
| Hormone Replacement Therapy | Estrogen increases thrombosis risk | Consider transdermal preparations |
| Polycystic Ovary Syndrome | Metabolic disturbances increase cardiovascular risk | Manage insulin resistance, obesity |
It’s key for doctors to understand these hormonal effects. This helps manage blood clotting risks. By knowing how hormones impact blood, we can improve patient care.
Metabolic Disorders and Blood Clots
We are learning more about how metabolic disorders contribute to the risk of forming blood clots. These disorders include diabetes, obesity, metabolic syndrome, and hyperhomocysteinemia. They affect the body’s normal metabolic processes and can lead to clotting.
Diabetes and Hypercoagulability
Diabetes increases the risk of blood clots. High blood sugar levels make the blood clot more easily. This is due to inflammation and damage to blood vessel linings.
Obesity and Inflammatory Markers
Obesity is a big risk factor for blood clots. Fat tissue is not just for storing fat; it’s involved in inflammation and metabolic processes. Obesity raises levels of inflammatory markers, which help blood clot more. It also often comes with other metabolic syndrome components, raising the risk even more.
Metabolic Syndrome
Metabolic syndrome is a group of conditions that raise the risk of type 2 diabetes and heart disease. It includes high blood pressure, high blood sugar, excess belly fat, and abnormal cholesterol levels. People with metabolic syndrome are more likely to get blood clots.
Hyperhomocysteinemia
Hyperhomocysteinemia is when blood has too much homocysteine. It damages blood vessel linings and promotes clotting. Though less common, it’s a big risk for blood clots in veins and arteries.
In conclusion, metabolic disorders significantly increase the risk of blood clots. Understanding these risks is key to preventing and managing blood clots. By managing these disorders, people can lower their risk of blood clots and heart problems.
Recognizing Blood Clot Symptoms
Knowing the signs of blood clots can save lives. Blood clots can form in different parts of the body. Their symptoms vary based on where and how severe the clot is.
Deep Vein Thrombosis Symptoms
Deep Vein Thrombosis (DVT) happens when a clot forms in deep veins, usually in the legs. Signs of DVT include:
- Swelling in the affected limb
- Pain or tenderness, mainly when standing or walking
- Warmth or redness in the affected area
- A feeling of heaviness or aching in the leg
Some people with DVT may not show any symptoms. Being alert is very important, mainly for those at higher risk.
Pulmonary Embolism Warning Signs
A pulmonary embolism (PE) happens when a clot breaks loose and goes to the lungs. It can block blood flow. Symptoms of PE are sudden and severe, such as:
- Shortness of breath or trouble breathing
- Chest pain that gets worse with deep breathing or coughing
- Coughing up blood
- Rapid heart rate or palpitations
Seek immediate medical help if you have these symptoms.
| Symptom | DVT | PE |
| Swelling | Common | Rare |
| Chest Pain | Rare | Common |
| Shortness of Breath | Rare | Common |
Arterial Clot Symptoms
Arterial clots form in arteries and can lead to heart attack or stroke. Symptoms include:
- Sudden numbness or weakness in the face, arm, or leg
- Confusion or trouble speaking
- Trouble seeing in one or both eyes
- Dizziness or loss of balance
As a medical expert says, “Recognizing stroke symptoms quickly is key for effective treatment and less damage.”
“Time is brain” is a mantra for stroke care, stressing the need for quick medical help.
When to Seek Emergency Care
If you or someone else has blood clot symptoms, get emergency care right away. Don’t wait; quick medical help can prevent serious problems or death.
Knowing the FAST acronym helps spot stroke symptoms: Face drooping, Arm weakness, Speech difficulty, Time to call for emergency services.
Diagnosing Blood Clotting Disorders
Diagnosing blood clotting disorders requires a detailed approach. We use clinical evaluation, lab tests, and imaging studies. This combination helps us find the cause and plan treatment.
Blood Tests for Clotting Disorders
Blood tests are key in diagnosing clotting disorders. They check the levels of clotting factors and biomarkers. For example, complete blood count (CBC) and coagulation panels help us see if the blood clots properly.
Some important blood tests include:
- Prothrombin Time (PT) and International Normalized Ratio (INR) for the extrinsic pathway.
- Activated Partial Thromboplastin Time (aPTT) for the intrinsic pathway.
- Fibrinogen level to check for bleeding or clotting risks.
Imaging Studies: Ultrasound, CT, and MRI
Imaging studies help us see blood clots and understand disorders. We use ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) for different body parts.
Ultrasound is often used for DVT, while CT scans help find pulmonary embolism.
Genetic Testing for Inherited Disorders
Genetic testing is critical for inherited clotting disorders. It looks for mutations in clotting factor genes, like Factor V Leiden and prothrombin gene mutation. This helps us diagnose and treat conditions like thrombophilia.
D-dimer and Other Biomarkers
D-dimer is a biomarker for blood clots. We use it to diagnose and monitor clotting disorders, like DVT or pulmonary embolism. Other biomarkers, like troponin and brain natriuretic peptide (BNP), help check for heart damage.
By using these methods together, we can accurately diagnose and treat blood clotting disorders.
Treatment Options for Blood Clotting Disorders
Managing blood clotting disorders needs a mix of treatments. Each one is chosen based on the person’s specific needs. We’ll look at the different ways to handle these conditions well.
Anticoagulant Medications
Anticoagulant drugs are key in treating blood clotting disorders. They stop new clots from forming and prevent existing ones from growing. Common ones include warfarin, apixaban, rivaroxaban, and dabigatran. Monitoring is critical to avoid problems.
The right drug depends on the patient’s health, other medicines, and lifestyle. For example, warfarin needs blood tests to check its effect. But newer drugs like apixaban and rivaroxaban don’t need as much monitoring.
Thrombolytic Therapy
Thrombolytic therapy is for emergencies. It dissolves clots that cause serious issues, like strokes or severe lung blockages. Time is key here, as starting treatment quickly improves results.
Surgical Interventions and Filters
Surgery might be needed for some blood clotting disorders. This could be removing the clot or using filters in the IVC to catch clots. These filters are for those who can’t take anticoagulants.
| Treatment Option | Description | Indications |
| Anticoagulant Medications | Prevent new clot formation and growth of existing clots | Long-term management of blood clotting disorders |
| Thrombolytic Therapy | Dissolve clots causing acute serious conditions | Acute ischemic stroke, severe pulmonary embolism |
| Surgical Interventions | Remove clots or place filters to prevent clot migration | Clots not responding to medical therapy, contraindications to anticoagulation |
Managing Underlying Conditions
It’s important to manage conditions like high blood pressure, diabetes, and high cholesterol. These can lead to clots. Changing your diet, exercising, and quitting smoking are also key.
Knowing the different treatments helps doctors create plans for each patient. This approach reduces risks and improves health outcomes.
Preventing Blood Clots
Preventing blood clots is key for those at risk. It requires lifestyle changes, medicines, and using compression devices. These steps help lower the chance of blood clots and their problems.
Lifestyle Modifications
Healthy choices are vital for preventing blood clots. Keeping a healthy weight, drinking plenty of water, and not sitting too long are important. Regular exercise boosts blood flow and lowers clot risk.
Those at high risk or with clot history should avoid smoking and drink less alcohol. Eating lots of fruits, veggies, and whole grains also helps your blood vessels.
Prophylactic Medications
Medicines can help prevent blood clots for those at high risk. Anticoagulants are often used. It’s important to take your medicine as directed and see your doctor regularly.
Compression Stockings and Devices
Compression stockings help prevent blood clots, mainly for those who can’t move much. They apply pressure to the legs to help blood flow back to the heart.
| Device Type | Usage | Benefits |
| Compression Stockings | Daily wear, specially during long trips or when sitting a lot | Improves blood flow, reduces swelling |
| Intermittent Pneumatic Compression Devices | Used during surgery or for patients at high risk of DVT | Enhances circulation, prevents clot formation |
Regular Movement and Exercise Strategies
Moving regularly is key to preventing blood clots. Simple actions like ankle rotations, toe wiggles, and walking help circulation. For those who can’t move much, physical therapy can help create a safe exercise plan.
By adding these strategies to your daily routine, you can lower your risk of blood clots and stay healthier.
Conclusion
We’ve looked into blood clots, their causes, risks, and related disorders. Knowing about blood clots is key to preventing and treating them. By understanding the risks, people can lower their chance of getting blood clots and their complications.
There are ways to prevent and treat blood clotting disorders. Changing your lifestyle, taking certain medicines, and wearing compression stockings can help. It’s vital to spot blood clots early and manage them well to improve outcomes.
By taking preventive steps and learning about blood clotting disorders, we can lower blood clot cases. Our aim is to offer full support and advice to those at risk. We want to make sure they get the care they need.
FAQ
What are the main causes of blood clots?
Blood clots are mainly caused by Virchow’s Triad. This includes hypercoagulability, blood vessel damage, and problems with blood flow or stasis.
What diseases increase the risk of blood clots?
Diseases like atrial fibrillation and heart failure raise the risk. Cancer, autoimmune diseases, and metabolic disorders like diabetes and obesity also increase the risk.
How do inherited conditions affect blood clotting?
Inherited conditions like Factor V Leiden mutation and prothrombin gene mutation can increase clotting risk. Deficiencies in proteins C and S, and antithrombin deficiency also play a role.
Can hormonal changes influence blood clotting?
Yes, hormonal changes can affect blood clotting. This includes changes during pregnancy, with hormonal contraceptives, or hormone replacement therapy.
What are the symptoms of a blood clot?
Symptoms vary by clot location. Deep vein thrombosis causes swelling, pain, and redness. Pulmonary embolism symptoms include sudden shortness of breath, chest pain, and coughing up blood.
How are blood clotting disorders diagnosed?
Diagnosis involves blood tests and imaging studies. Tests like ultrasound, CT, and MRI help visualize clots. Genetic testing is used for inherited conditions.
What are the treatment options for blood clotting disorders?
Treatment includes anticoagulant medications and thrombolytic therapy. Surgical interventions and managing underlying conditions are also used.
How can blood clots be prevented?
Prevention includes lifestyle changes and prophylactic medications. Using compression stockings and encouraging exercise are also important.
Are there any specific risk factors that increase the likelihood of developing blood clots?
Yes, risk factors include a history of blood clots and family history. Recent surgery, prolonged immobilization, and certain medical conditions also increase risk.
Can lifestyle changes reduce the risk of blood clots?
Yes, lifestyle changes like maintaining a healthy weight and staying hydrated can help. Avoiding immobility and exercising regularly also reduce risk.
References
NHS – Deep Vein Thrombosis (DVT)




































