Last Updated on November 25, 2025 by Ugurkan Demir
Learn what causes plaque buildup in arteries and how to prevent arteriosclerosis naturally.
Cardiovascular diseases are a major cause of death globally. The World Health Organization says coronary artery disease is a big part of this. Arteriosclerosis, or the hardening of arteries, is a big risk for these diseases.
At Liv Hospital, we know how important it is to understand plaque buildup and prevent arteriosclerosis. By knowing the risks and taking steps to prevent them, people can lower their chance of heart disease.
We will look at the seven main reasons for plaque buildup in arteries. We will also talk about how to keep arteries healthy.
It’s important to know about arterial plaque to keep your heart healthy. If not treated, it can cause serious problems.
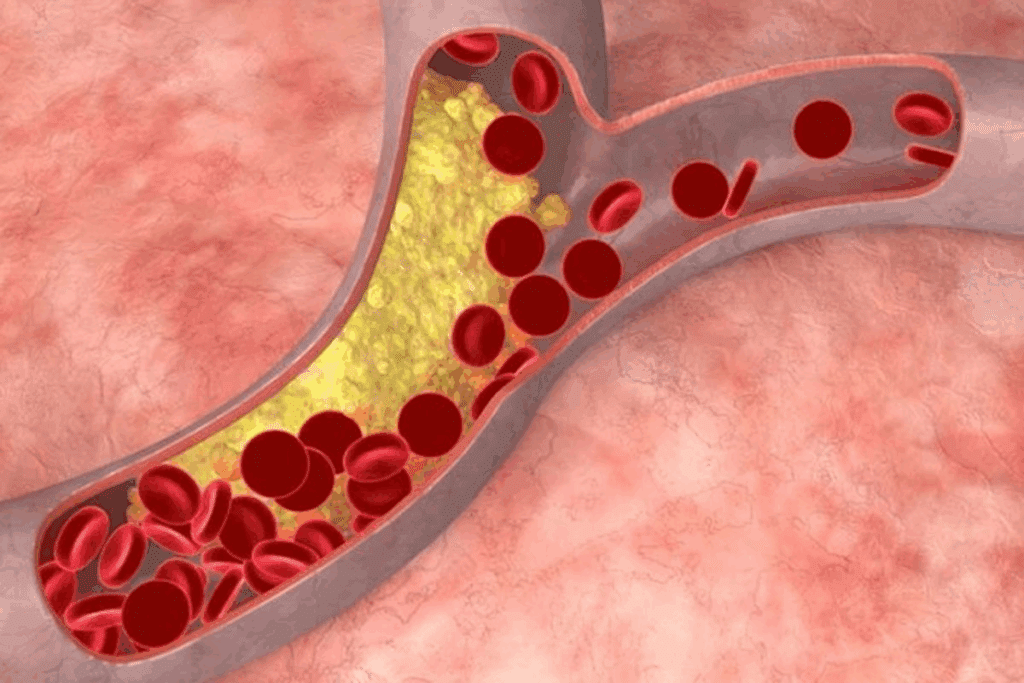
Atherosclerosis is when plaque builds up in artery walls, making them hard and narrow. This can block blood flow, leading to heart attacks and strokes.
The term atherosclerosis means fats, cholesterol, and other stuff build up in artery walls. This can block blood flow and cause serious health problems.
Plaque forms in arteries through a complex process. It starts with damage to the artery’s inner layer, often from high blood pressure or smoking. Then, plaque builds up at the injury site.
The process includes:
Though often confused, atherosclerosis and arteriosclerosis are different. Arteriosclerosis is when arteries harden, which can happen for many reasons. Atherosclerosis is a specific type of arteriosclerosis, caused by plaque buildup.
| Condition | Description |
| Atherosclerosis | Buildup of plaque in arterial walls, leading to hardening and narrowing |
| Arteriosclerosis | Hardening or stiffening of the arteries, can be due to various causes |
In summary, all atherosclerosis is arteriosclerosis, but not all arteriosclerosis is atherosclerosis. Knowing this helps with accurate diagnosis and treatment.
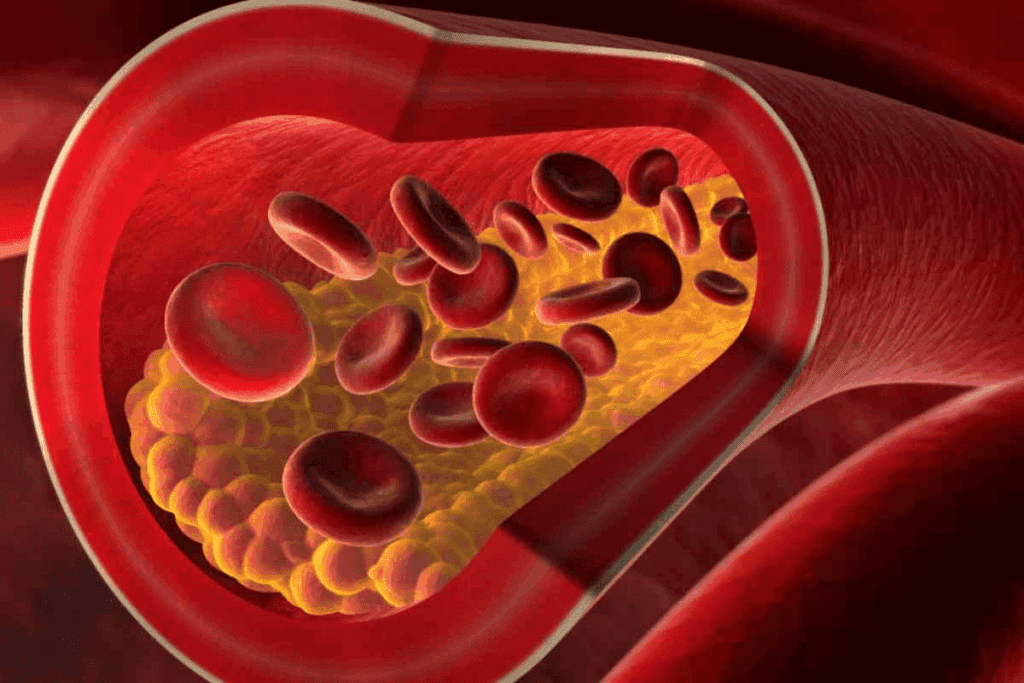
To understand the danger of artery plaque, we need to look at what it’s made of. Artery plaque is a mix of different substances that build up inside arteries.
Cholesterol, fats, and waste are key parts of artery plaque. Cholesterol, mainly low-density lipoprotein (LDL), is a big player in forming plaque. LDL cholesterol can get into the artery wall, get oxidized, and start an inflammatory response. This attracts immune cells like macrophages.
Fats, like triglycerides, also help plaque grow. Waste from dead cells and other debris adds to the plaque. This mix creates an environment where inflammation and plaque growth can happen.
Artery plaque also has calcium and fibrin. Calcium makes the plaque hard and less likely to break, but it also makes the artery walls brittle. Fibrin, a clotting protein, is in the plaque too. It helps stabilize the plaque but also makes it more dangerous by increasing the risk of blockages.
The mix of substances in artery plaque makes it dangerous because it can rupture. When it does, it releases material that can cause blood clots. These clots can block the artery, leading to heart attacks or strokes.
The instability of plaque comes from its mix of substances. Plaques with lots of lipids and thin fibrous caps are more likely to rupture. Knowing what artery plaque is made of helps us understand the risks and find ways to stop it from forming and growing.
| Component | Role in Plaque Formation | Effect on Plaque Stability |
| Cholesterol (LDL) | Penetrates arterial wall, triggers inflammation | Increases risk of rupture |
| Fats (Triglycerides) | Contributes to plaque buildup | Enhances plaque growth |
| Calcium | Makes plaque more rigid | Increases brittleness |
| Fibrin | Involved in blood clotting | Contributes to plaque stability |
| Cellular Waste | Adds to plaque composition | Increases inflammation |
It’s important to know how hardening arteries progress. This knowledge helps in early detection and prevention. The journey starts with plaque forming in the coronary arteries.
Plaque can start forming in the coronary arteries early in life. Studies show that cholesterol, fats, and waste start building up on the artery walls. This can begin as early as childhood and grow quietly over time.
Factors that contribute to early plaque buildup include:
The hardening of arteries goes through several stages:
| Stage | Description |
| 1. Initial Plaque Formation | Plaque starts to build up on the arterial walls. |
| 2. Plaque Growth | The plaque continues to grow, narrowing the arterial lumen. |
| 3. Calcification | Calcium deposits form within the plaque, making it harder. |
| 4. Advanced Hardening | The arteries become significantly hardened, reducing blood flow. |
Finding plaque buildup early is key to stopping it from getting worse. Several tests can spot plaque buildup, such as:
By understanding how arteries harden and spotting plaque early, we can prevent heart disease.
Many risk factors lead to plaque buildup in arteries. Knowing these factors is key to stopping and managing atherosclerosis. We’ll look at the main causes of plaque and how they work together.
Risk factors for plaque buildup fall into two groups: modifiable and non-modifiable. Modifiable risk factors are things we can change, like high LDL cholesterol, high blood pressure, smoking, diabetes, being overweight, and not being active enough. Non-modifiable risk factors, like our genes and family history, we can’t change.
“Knowing what we can change helps us take action,” say heart health experts. By working on these factors, we can lower our risk of atherosclerosis.
Having many risk factors at once makes atherosclerosis worse. For example, high blood pressure and high LDL cholesterol together raise the risk a lot. Smoking and diabetes also make plaque grow faster. It’s important to understand how these factors work together to fight atherosclerosis.
Managing many risk factors needs a big plan that includes changing our lifestyle and sometimes getting medical help. By tackling these factors together, we can keep our arteries healthy.
By knowing and tackling these risk factors, we can make big strides in preventing atherosclerosis and keeping our hearts healthy.
Eating foods high in saturated fats and cholesterol can raise LDL cholesterol levels. This is a major factor in atherosclerosis. Atherosclerosis happens when plaque builds up in arteries, causing them to harden and narrow.
Cholesterol is a fat found in the blood. There are two main types: LDL and HDL. LDL cholesterol is called “bad” because high levels can cause artery plaque. On the other hand, HDL cholesterol is “good” because it helps remove other cholesterol from the blood.
It’s important to keep LDL and HDL cholesterol in balance for good artery health. High LDL levels can be lowered with diet changes and, if needed, medication.
Some foods can lead to high cholesterol and plaque buildup. Foods high in saturated fats, like red meat and full-fat dairy, raise LDL cholesterol. Foods with trans fats, found in processed snacks and baked goods, also contribute to plaque.
Eating a heart-healthy diet can help manage cholesterol and prevent plaque. Diets rich in fruits, vegetables, whole grains, and lean proteins are good for arteries. The Mediterranean diet, which focuses on these foods, lowers the risk of heart disease.
Making dietary changes is a big step towards preventing artery hardening. Understanding how diet affects cholesterol and plaque can help people make better choices for their heart health.
A sedentary lifestyle is not just about gaining weight. It also harms our arteries. Not moving enough can lead to plaque buildup in arteries. This can cause arteriosclerosis. We will look at how sitting too much affects our arteries, how moving helps reduce plaque, and the right amount of exercise for heart health.
Being active is key for healthy arteries. Exercise boosts blood flow, lowers blood pressure, and controls cholesterol. Without enough activity, arteries become stiff and the inner lining of blood vessels, called the endothelium, doesn’t work right. This can cause inflammation and plaque buildup.
Physical inactivity harms the heart and increases risks of obesity, high blood pressure, and diabetes. These conditions raise the risk of atherosclerosis.
Regular exercise helps reduce plaque in several ways. It improves cholesterol levels by increasing good cholesterol and lowering bad cholesterol. Exercise also helps manage weight, blood pressure, and insulin levels. All these factors reduce plaque risk.
Research shows active people face fewer heart problems than those who don’t move much. The American Heart Association suggests 150 minutes of moderate or 75 minutes of vigorous activity weekly for heart health.
Finding the right exercise amount and intensity is important. While guidelines suggest 150 minutes of moderate or 75 minutes of vigorous activity weekly, individual needs vary. Age, health, and fitness level play a role.
Even a little bit of activity is better than none. For beginners, starting small and gradually increasing activity can help maintain heart health.
Tobacco use, like smoking, greatly increases the risk of atherosclerosis. This is a condition where plaque builds up in arteries. We will look at how smoking harms arteries, the dangers of secondhand smoke, and the risks of vaping and new tobacco products.
Smoking harms arteries in many ways. It damages the inner lining of blood vessels, making them more prone to plaque buildup. It also raises blood pressure and heart rate, stressing the heart.
Smoking leads to blood clots, which can cause heart attacks and strokes. The chemicals in tobacco smoke, like nicotine and carbon monoxide, play a big role. Nicotine increases heart rate and blood pressure. Carbon monoxide reduces blood’s oxygen-carrying ability, damaging blood vessels.
Secondhand smoke is also harmful to heart health. People not smoking but exposed to secondhand smoke face higher risks of heart disease and stroke. Secondhand smoke affects arteries in similar ways to smoking, including damaging the inner lining and increasing inflammation.
A study found that even brief exposure to secondhand smoke can harm blood vessels. This shows why smoke-free policies are important for public health.
| Health Impact | Active Smoking | Secondhand Smoke Exposure |
| Endothelial Dysfunction | Significant damage | Moderate damage |
| Increased Blood Pressure | Marked increase | Moderate increase |
| Cardiovascular Risk | High risk | Moderate to high risk |
Vaping and newer tobacco products bring new risks to heart health. At first, they seemed safer, but research shows they can harm arteries and increase atherosclerosis risk.
The long-term effects of vaping and new tobacco products on heart health are not clear. But, the data suggest they are not safe and may lead to heart disease.
Hypertension is key in damaging arterial walls, leading to plaque buildup. High blood pressure is a big risk for heart diseases. It affects blood vessels in many ways.
High blood pressure puts extra force on arterial walls. This can cause micro-tears in the blood vessel’s inner layer. The body tries to fix these tears, leading to plaque buildup over time.
“Hypertension is a major risk factor for heart disease,” says recent guidelines. Controlling it is key to stopping atherosclerosis.
Hypertension and atherosclerosis create a vicious cycle. High blood pressure damages walls and speeds up atherosclerosis. As atherosclerosis grows, it makes blood pressure worse by stiffening arteries.
This creates a positive feedback loop. Each condition makes the other worse.
Managing blood pressure is vital to prevent artery hardening. The American Heart Association suggests a target of less than 130/80 mmHg for most adults. Staying within this range can lower the risk of atherosclerosis and its complications.
Understanding hypertension’s effect on blood vessels is key. Taking steps to manage blood pressure can greatly reduce the risk of arteriosclerosis and heart disease.
Diabetes and atherosclerosis are linked in a complex way. High blood sugar in diabetes can harm blood vessel linings. This makes them more likely to get clogged with plaque.
Diabetes speeds up atherosclerosis in several ways. Insulin resistance, which often leads to type 2 diabetes, causes bad cholesterol levels. High blood sugar also causes inflammation and damage to blood vessels.
Important metabolic pathways include:
Keeping blood sugar levels in check is key for diabetic patients. Research shows that controlling blood sugar can lower heart disease risk. Blood sugar swings also increase heart disease risk.
Managing diabetes well involves many steps. This includes making lifestyle changes and using medicines. Lifestyle changes include:
Medicines like metformin and GLP-1 receptor agonists can help. It’s also important to watch blood pressure and cholesterol levels closely.
Obesity, often linked with metabolic syndrome, raises the risk of heart disease. We’ll look into how fat placement, inflammation, and managing weight are key in this area.
The way fat is spread in the body affects heart health. Central or visceral obesity is very risky. It’s linked to higher chances of metabolic syndrome, type 2 diabetes, and heart disease. Visceral fat also releases substances that can cause insulin resistance and worsen heart risk.
Obesity leads to ongoing inflammation, which helps atherosclerosis grow. Fat tissue isn’t just for storing fat; it’s active and releases inflammatory cytokines. These can harm the blood vessel lining, help plaque form, and up heart disease risk.
Managing weight well is key to lowering heart disease risk from obesity. Lifestyle changes, like better eating and more exercise, are essential. Eating more fruits, veggies, whole grains, and lean proteins helps with weight loss. Exercise not only helps with weight but also improves heart health by bettering lipid levels and blood pressure.
Family history and genetics play a big role in plaque buildup in arteries. Studies show that people with a family history of heart disease are more at risk. This suggests a strong genetic link.
The genetics of atherosclerosis are complex. Many genes can affect heart health. Research has found genes linked to heart disease and other conditions.
Genetics can impact the heart in several ways. For example, some genes can raise LDL cholesterol levels. This is a risk factor for plaque buildup.
Some genetic conditions speed up atherosclerosis. Familial Hypercholesterolemia (FH) is one. It causes very high LDL cholesterol, leading to early heart disease. Other conditions, like familial combined hyperlipidemia, also raise the risk.
| Genetic Condition | Effect on Atherosclerosis | Risk Level |
| Familial Hypercholesterolemia | Very high LDL cholesterol | High |
| Familial Combined Hyperlipidemia | Elevated levels of LDL and triglycerides | High |
| Genetic variants affecting lipid metabolism | Increased risk of plaque buildup | Moderate to High |
Genetic testing can reveal a person’s risk for atherosclerosis. It’s useful for those with a family history of heart disease. Tests can spot genetic risks, helping with early prevention.
But, it’s important to see genetic testing as part of a bigger picture. We suggest talking to a doctor about it. They can help understand its role in your health plan.
To prevent arteriosclerosis, a mix of lifestyle changes and medical steps is key. We’ll look at diet, exercise, medications, and procedures to fight this condition.
Eating right is vital to stop arteriosclerosis. Eat more fruits, veggies, and whole grains to cut down on plaque. Avoid saturated fats, trans fats, and high cholesterol.
Here are some diet tips:
| Dietary Component | Recommended Foods | Benefits |
| Fruits and Vegetables | Apples, berries, spinach, broccoli | Rich in antioxidants, fiber, and vitamins |
| Whole Grains | Oats, quinoa, brown rice | High in fiber, vitamins, and minerals |
| Lean Proteins | Chicken, fish, legumes | Low in saturated fats, high in protein |
Exercise is key for artery health. Aim for 150 minutes of moderate exercise, or 75 minutes of vigorous exercise, or a mix, weekly.
Here are some exercise tips:
Medicines can help stop plaque buildup. Statins lower LDL cholesterol. Antiplatelet drugs prevent blood clots.
Other medicines include:
For severe arteriosclerosis, medical procedures might be needed. Angioplasty and stenting open narrowed arteries. CABG bypasses blocked arteries.
Choosing a procedure depends on the condition’s severity and your health. Always talk to a doctor to find the best treatment.
Knowing why plaque builds up in arteries is key to keeping your arteries healthy. It helps prevent heart disease. By understanding the risks, we can start to lower them.
To manage your artery health, you need to make lifestyle changes and sometimes see a doctor. Eating right, staying active, managing stress, and taking medicine are important steps.
Keeping your arteries healthy is a long-term effort. Making smart choices about your lifestyle and health can greatly lower your risk of heart disease. This keeps your arteries in top shape.
We urge you to start making healthier choices for your heart today. By following the tips in this article, you’ll be on the path to better artery health. This leads to a healthier life ahead.
The hardening of the arteries, also known as arteriosclerosis, is when arteries get narrow and stiff. This happens because of plaque buildup. It makes it harder for blood to flow.
Atherosclerosis is a type of arteriosclerosis. It’s when plaque builds up in the arteries. This plaque is made of cholesterol, fats, cellular waste, calcium, and fibrin.
Plaque builds up in the arteries when cholesterol, fats, and cellular waste stick to the inner walls. This causes inflammation and damage.
Artery plaque is made of cholesterol, fats, cellular waste, calcium, and fibrin. These components make the plaque unstable. They can cause cardiovascular events.
Risk factors for atherosclerosis include a poor diet and high cholesterol. A sedentary lifestyle, smoking, and hypertension are also risks. Diabetes, obesity, and genetics play a role too.
Plaque buildup in the coronary arteries can start early, often in the teenage years or early twenties. It can progress over time if not treated.
Atherosclerosis is a specific type of arteriosclerosis. It’s when plaque builds up. Arteriosclerosis is a broader term. It includes various conditions that harden the arteries.
To prevent plaque buildup, adopt a healthy lifestyle. Eat a balanced diet, exercise regularly, don’t smoke, manage stress, and control conditions like hypertension and diabetes.
To prevent atherosclerosis, eat a diet rich in fruits, vegetables, whole grains, and lean proteins. Limit saturated fats, cholesterol, and sodium.
Yes, genetic factors can significantly increase the risk of atherosclerosis. This is true if there’s a family history of the condition.
Exercise helps prevent plaque buildup. It improves arterial function, reduces inflammation, and promotes cardiovascular health.
Hypertension damages arterial walls by causing inflammation, scarring, and narrowing. This makes arteries more susceptible to plaque buildup.
Diabetes increases the risk of atherosclerosis. It damages the inner lining of blood vessels. This makes them more prone to plaque buildup and cardiovascular events.
Yes, obesity can contribute to atherosclerosis. It promotes inflammation, insulin resistance, and other metabolic changes. These increase cardiovascular risk.
Pathophysiology of Atherosclerosis – PMC.” (2023). PLoS One review. PubMed Central
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!