Last Updated on November 27, 2025 by Bilal Hasdemir

Cancer treatment has changed a lot with new technology, like external beam radiotherapy. The main tool for this is the linear accelerator (LINAC). It’s a cancer radiotherapy machine that makes high-energy beams to hit tumors.
LINAC is made to give exact and custom radiation therapy. It’s key in the battle against cancer. External beam radiotherapy treats specific parts of the body where tumors are found.
Key Takeaways
- Linear Accelerator (LINAC) is the most common device used in external beam radiotherapy.
- LINAC generates high-energy radiation beams to target and destroy tumors.
- External beam radiotherapy is a local treatment, focusing on specific areas of the body.
- This treatment is tailored to individual patient needs, ensuring precision and safety.
- LINAC plays a critical role in cancer treatment, providing a sophisticated way to deliver radiotherapy.
Understanding Radiotherapy and Its Role in Cancer Treatment

External beam radiotherapy is a common cancer treatment. It uses advanced technology to send radiation beams from outside the body. This method is precise, targeting cancer cells while protecting healthy tissue.
The Purpose of Radiotherapy in Modern Medicine
Radiotherapy’s main goal is to kill cancer cells while keeping healthy tissue safe. It treats many types of cancer and uses advanced imaging to protect healthy areas. It can be used alone or with other treatments like surgery and chemotherapy.
“Radiotherapy has changed cancer treatment by focusing on killing cancer cells,” says a leading oncologist. This shows how important radiotherapy is in cancer care today.
How Radiation Affects Cancer Cells
Radiation therapy damages cancer cells’ DNA, stopping them from growing. The goal is to give a precise dose of radiation to the tumor. This way, it harms cancer cells more while keeping healthy cells safe.
- Damages the DNA of cancer cells
- Prevents cancer cells from dividing and growing
- Maximizes damage to cancer cells while sparing healthy tissue
When Radiotherapy Is Recommended
The choice to use radiotherapy depends on the cancer type, stage, and the patient’s health. It’s often used for patients with localized tumors or those needing relief from symptoms.
| Cancer Type | Stage | Radiotherapy Role |
| Breast Cancer | Early-stage | Adjuvant treatment post-surgery |
| Lung Cancer | Locally advanced | Primary treatment with chemotherapy |
| Prostate Cancer | Localized | Curative treatment |
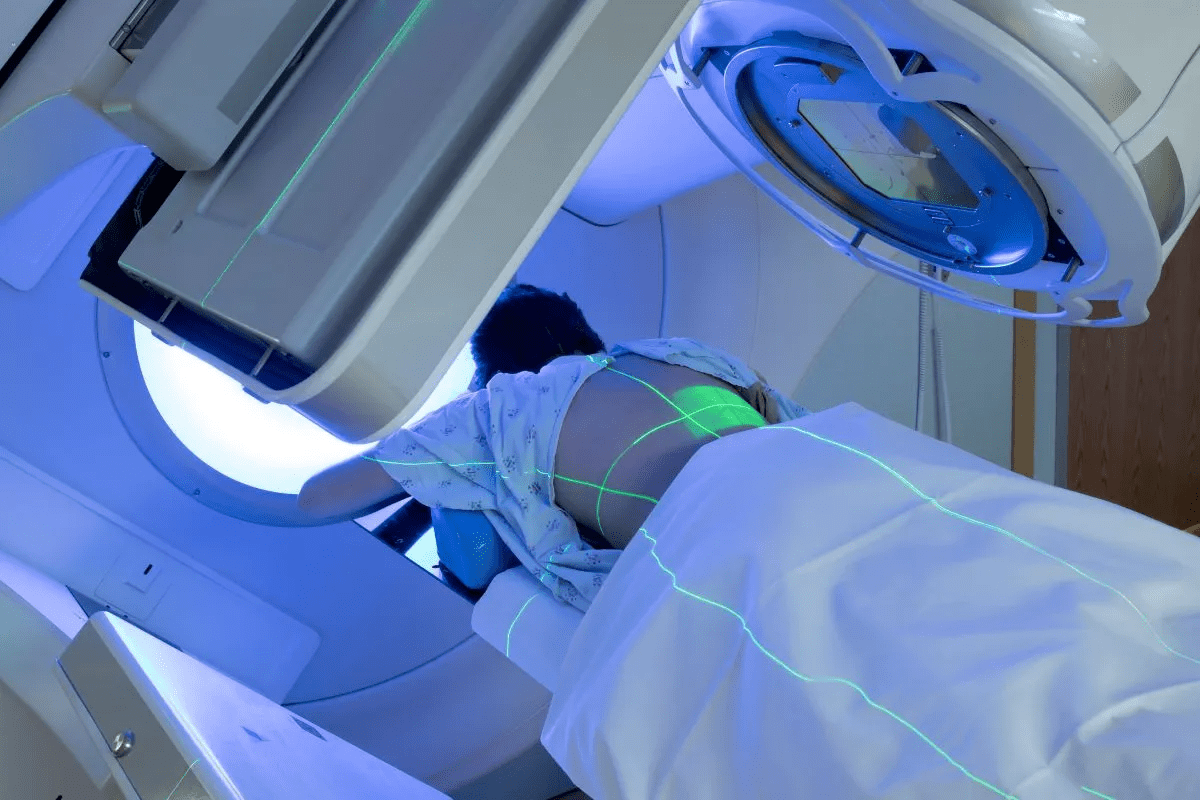
What Does a Radiotherapy Machine Look Like: An Overview

The Linear Accelerator, or LINAC, is a key tool in fighting cancer. It’s at the heart of external beam radiation therapy. This method targets tumors with precision, protecting healthy tissue.
The Linear Accelerator (LINAC): The Standard Radiotherapy Machine
The LINAC is the go-to radiotherapy machine today. It has parts like the treatment head and the gantry. The gantry rotates to aim at tumors from different angles. Its high-energy radiation is vital for cancer treatment.
Size and Physical Characteristics
LINAC machines are big, with the gantry being the most noticeable part. The treatment head is where the radiation beam is shaped. The machine needs a large room to operate safely.
Treatment Room Setup and Environment
The treatment room is made for LINAC and safety. It’s built with thick walls to block radiation leaks. The LINAC is set up for flexibility in targeting tumors. The treatment couch ensures patient comfort and precision.
| Component | Description | Function |
| Treatment Head | Delivers radiation beams | Generates and shapes radiation for tumor targeting |
| Gantry | Rotating arm | Allows for precise tumor targeting from multiple angles |
| Treatment Couch | Patient positioning | Ensures accurate patient placement for effective treatment |
Types of External Beam Radiotherapy Machines
There are many types of external beam radiotherapy machines used in cancer treatment. They deliver precise radiation to tumors, protecting healthy tissues nearby.
Conventional Linear Accelerators
Conventional Linear Accelerators (LINACs) are the most common machines. They make high-energy X-rays by accelerating electrons. LINACs treat a wide range of cancers, from the brain to other parts of the body.
For more details, visit the National Cancer Institute’s page on external beam radiation.
TomoTherapy Units
TomoTherapy units combine a Linear Accelerator with a CT scanner. This allows for precise radiation delivery. It’s great for treating complex tumors with less damage to nearby tissues.
Proton Therapy Systems
Proton therapy uses protons instead of X-rays. It’s very effective for tumors near important structures. This is because it delivers a high dose of radiation to the tumor while protecting the surrounding tissues.
Gamma Knife Radiosurgery Units
Gamma Knife radiosurgery uses cobalt sources for precise radiation. It’s mainly for brain tumors and abnormalities. Its precision makes it a top choice for hard-to-treat conditions.
In summary, the variety of external beam radiotherapy machines helps tailor treatments to each patient. This improves outcomes and reduces side effects.
Key Components of External Beam Radiotherapy Equipment
Understanding the parts of external beam radiotherapy equipment is key to grasping cancer treatment. These machines are complex, needing precise engineering to work well.
The Treatment Head and Gantry System
The treatment head sends the radiation beam to the tumor. It’s part of the gantry system, which targets tumors from different angles. The gantry system rotates around the patient, directing the beam at the tumor from various sides.
The treatment head and gantry system work together. They focus the radiation on the tumor, protecting healthy tissues.
The Treatment Couch and Positioning Systems
The treatment couch supports the patient during radiotherapy. It has advanced positioning systems for accurate alignment with the radiation beam. These systems include devices to keep the patient steady and in the right spot.
Getting the patient’s position right is key for effective radiotherapy. It ensures the radiation hits the tumor exactly.
Control Systems and Monitoring Equipment
Control systems run and check the radiotherapy equipment. They use software and hardware to manage radiation, monitor treatment, and keep the machine safe.
Monitoring equipment checks if the radiation is being delivered right and the patient is in the right spot. It uses cameras, sensors, and other tech for real-time feedback during treatment.
Beam-Shaping Devices and Collimators
Beam-shaping devices and collimators shape the radiation beam to fit the tumor. They reduce healthy tissue exposure by matching the beam to the tumor’s shape.
Using advanced beam-shaping devices and collimators is vital for precise radiotherapy.
The Science Behind External Beam Radiation Therapy
External beam radiation therapy uses advanced technology to fight cancer. It’s a key part of cancer treatment. It targets tumors with precision, protecting healthy tissue.
How Radiation Beams Are Generated
A device called a linear accelerator (LINAC) makes the radiation beams. It speeds up electrons, which then hit a metal target. This creates high-energy X-rays that kill cancer cells.
Key Components of a LINAC:
- Electron gun: Produces electrons that are accelerated.
- Accelerating waveguide: Where electrons gain energy.
- Target: Converts the accelerated electrons into X-rays.
- Collimator: Shapes the X-ray beam to match the tumor’s dimensions.
Types of Radiation Used in External Beam Therapy
Mostly, photon beams are used in external beam radiation therapy. But, proton beams are used too, for tumors near important areas. Proton therapy is precise, causing less damage to healthy tissue.
| Type of Radiation | Characteristics | Clinical Use |
| Photon Beams | High-energy X-rays, widely available | Most common form of external beam radiation therapy |
| Proton Beams | Charged particles, precise energy delivery | Used for tumors near critical structures or in pediatric cases |
Beam Shaping and Targeting Technologies
Beam shaping is key to deliver radiation just to the tumor. Technologies like multi-leaf collimators (MLCs) and advanced imaging systems help. They make sure the radiation hits the right spot.
Precision and Safety Mechanisms
Advanced imaging and positioning systems ensure the radiation hits the tumor right. Safety steps include quality checks, machine calibration, and careful planning. These steps protect healthy tissue from radiation.
Safety Measures:
- Regular machine maintenance and calibration.
- Comprehensive treatment planning.
- Use of immobilization devices to ensure patient positioning.
- Image-guided radiation therapy (IGRT) for real-time monitoring.
The External Beam Radiotherapy Treatment Process
The external beam radiotherapy treatment process has several key stages. It starts with planning and ends with quality checks. This process aims to hit cancer tumors with precision, keeping healthy tissues safe.
Pre-Treatment Planning and Imaging
Planning starts with detailed imaging and simulation. CT scans, MRI, or PET scans help see the tumor and its surroundings. This info helps create a treatment plan just for the patient.
The radiation oncologist marks the target area and the tissues to avoid. The treatment planning system (TPS) then shapes the radiation beams. This ensures the tumor gets the right dose, while healthy tissues are protected.
Patient Positioning and Immobilization Techniques
Getting the patient in the right position is key. Immobilization devices like molds, casts, or masks keep the patient steady. This keeps the radiation on target.
The treatment couch has precision positioning systems for adjustments. This ensures the patient is perfectly aligned with the beams.
| Immobilization Technique | Description | Application |
| Molds | Custom-made to fit the patient’s body part | Used for tumors in the abdomen or pelvis |
| Masks | Thermoplastic masks that mold to the patient’s face or body part | Commonly used for head and neck cancers |
| Casts | Rigid or semi-rigid casts that hold the patient in position | Used for tumors in various parts of the body |
Beam Delivery and Treatment Execution
With the patient set, treatment starts. The linear accelerator sends beams from planned angles. These beams are shaped to fit the tumor, ensuring effective treatment.
The treatment is watched in real-time to stick to the plan. Image-guided radiation therapy (IGRT) checks the patient’s and target’s position before and during treatment.
Quality Assurance Procedures
Quality assurance (QA) is vital in radiotherapy. Regular checks on the equipment ensure it works right. This includes the linear accelerator and imaging systems.
Also, QA checks on each patient to make sure the treatment plan works. This involves measuring the dose to a phantom or using other methods to check accuracy.
Duration and Frequency: How Long Is a Radiotherapy Session?
Radiotherapy sessions can last from a few minutes to 30 minutes. The exact time depends on the treatment plan. Each plan is made just for the patient, taking into account their cancer and needs.
Typical Session Length and What to Expect
A typical session is short, lasting from a few minutes to 30 minutes. But the actual radiation time is just a few minutes. The rest of the time is for setting up and checking everything is right.
Patients lie on a couch during the session. They might use special devices to stay in place. The team leaves, and the radiation is given as planned. Patients might hear sounds from the machine as it moves.
Treatment Schedules and Course Duration
Treatment schedules vary a lot. For treatments aiming to cure cancer, sessions might be daily, Monday to Friday, for weeks. The number of sessions can be from 10 to 35 or more, based on the cancer type and stage.
Palliative radiotherapy, which aims to ease symptoms, might have fewer sessions. Sometimes, it’s just one or a few sessions, depending on the patient’s condition and treatment goals.
Key factors influencing treatment schedules include:
- Type and stage of cancer
- Treatment goals (curative vs. palliative)
- Patient’s overall health
- Specific radiotherapy technique being used
Factors Affecting Treatment Length
Several things can affect how long radiotherapy lasts. These include the cancer type, its location, and the treatment’s goal. For example, treatments for tumors that are sensitive to radiation might be shorter. Tumors that are harder to treat might need longer courses.
Differences Between Curative and Palliative Schedules
Curative and palliative radiotherapy have different schedules. Curative treatments aim to cure the cancer and are given in higher doses over a longer time. This helps minimize side effects.
Palliative treatments focus on symptom relief. They often involve shorter courses with higher doses per session. The goal is to improve the patient’s quality of life with advanced cancer.
| Treatment Aspect | Curative Radiotherapy | Palliative Radiotherapy |
| Treatment Duration | Several weeks | One or a few sessions |
| Dose per Session | Lower dose | Higher dose |
| Frequency | Daily, Monday to Friday | Variable, often less frequent |
Advanced Radiotherapy Technologies and Techniques
Advanced radiotherapy technologies have changed cancer treatment. They offer better results and fewer side effects.
Image-Guided Radiation Therapy (IGRT)
Image-Guided Radiation Therapy (IGRT) uses imaging in treatment. It helps target tumors accurately, even when they move or are close to important areas.
IGRT Benefits: It’s more precise, safer for healthy tissues, and improves treatment success.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) uses beams of different intensities from many angles. It shapes the radiation dose closely, protecting healthy areas.
IMRT Advantages: It’s precise, reduces harm to healthy tissues, and controls tumors better.
Stereotactic Body Radiation Therapy (SBRT)
Stereotactic Body Radiation Therapy (SBRT) gives high doses of radiation in a few sessions. It’s great for small, well-defined tumors.
SBRT Characteristics: It uses high doses, targets precisely, and needs only a few sessions.
Adaptive Radiation Therapy
Adaptive Radiation Therapy changes the treatment plan as needed. It adapts to changes in the tumor, keeping treatment safe and effective.
| Therapy Type | Description | Key Benefits |
| IGRT | Integrates imaging into radiotherapy | Enhanced precision, reduced risk |
| IMRT | Delivers radiation beams of varying intensities | Highly conformal dose, reduced toxicity |
| SBRT | Delivers high doses in few fractions | Effective for small tumors, high dose per fraction |
| Adaptive RT | Modifies treatment plan during therapy | Ensures treatment remains effective and safe |
Conclusion: The Evolution and Future of Radiotherapy Technology
Radiotherapy has seen big changes, changing how we fight cancer. New tech makes treatments more precise and better. This means patients get better results.
New tech in radiotherapy is on the horizon. We’ll see treatments that are safer and work better. Research and new tools like AI will keep improving care.
As radiotherapy tech gets better, treatments will target cancer more accurately. The future looks bright with more innovation. Cancer patients will get care that’s more effective and tailored to them.
FAQ
What does a radiotherapy machine look like?
A radiotherapy machine, like a Linear Accelerator (LINAC), is big. It has a treatment head that shoots out radiation beams. The gantry rotates to aim at tumors precisely.
What is external beam radiotherapy?
External beam radiotherapy is a way to treat cancer. It uses high-energy beams to target tumors. This damages the DNA of cancer cells, stopping them from growing.
How long is a session of radiotherapy?
Radiotherapy sessions can last from 10 to 30 minutes. This depends on the treatment’s complexity and the machine used.
What are the different types of external beam radiotherapy machines?
There are many types, like conventional LINACs and TomoTherapy Units. There are also Proton Therapy Systems and Gamma Knife Radiosurgery Units. Each has its own features and uses.
How does external beam radiation therapy work?
It generates high-energy beams that target tumors. LINACs are used to damage cancer cells’ DNA.
What is the role of the gantry system in radiotherapy?
The gantry system is a rotating arm. It lets the treatment head move around the patient. This allows for precise targeting of tumors from different angles.
What is the purpose of beam-shaping devices in radiotherapy?
Beam-shaping devices shape the radiation beam to match the tumor’s shape. This helps protect healthy tissues nearby.
How often are radiotherapy sessions scheduled?
Sessions can be daily for weeks or less often. It depends on the treatment plan.
What is the difference between curative and palliative radiotherapy schedules?
Curative radiotherapy aims to cure cancer. It needs a more intense schedule. Palliative radiotherapy focuses on symptom relief and has a less intense schedule.
What are some advanced radiotherapy technologies?
Advanced technologies include IGRT, IMRT, SBRT, and Adaptive Radiation Therapy. They improve precision and effectiveness.
References
- RadiologyInfo.org. (2025). LINAC (Linear Accelerator).
https://www.radiologyinfo.org/en/info/linac
- Cancer Research UK. (2024). What is external radiotherapy?
https://www.cancerresearchuk.org/about-cancer/treatment/radiotherapy/external/what