Last Updated on November 18, 2025 by Ugurkan Demir

Orthopedic doctors, also known as orthopaedic physicians or ortho specialists, are key in treating musculoskeletal disorders. The musculoskeletal system includes bones, joints, muscles, ligaments, and tendons. It’s prone to many conditions that can really affect your life.
Musculoskeletal diseases and conditions affect nearly 128 million people in the United States. This makes orthopedic care very important. Orthopedic doctors often treat issues like arthritis, osteoporosis, fractures, dislocations, sprains, strains, tendonitis, and muscle injuries.
At Liv Hospital, we focus on innovative, patient-centered orthopedic care. We use the latest treatments to help patients move better and feel less pain. Our team is all about helping you get back to your active life.
Key Takeaways
- Orthopedic doctors diagnose and treat musculoskeletal disorders.
- Common conditions treated include arthritis, osteoporosis, and fractures.
- Musculoskeletal diseases affect nearly 128 million people in the US.
- Liv Hospital provides innovative, patient-focused orthopedic care.
- Orthopedic care is key for restoring mobility and easing pain.
Understanding Orthopedic Medicine: Scope and Specialization

Orthopedic doctors are key in healthcare. They focus on treating musculoskeletal disorders. This includes conditions affecting bones, joints, muscles, and more.
They help with many musculoskeletal problems. This ranges from simple injuries to complex surgeries. Their work includes both surgery and non-surgical treatments to fix problems and ease pain.
The Role of Orthopedic Doctors in Healthcare
Orthopedic doctors are vital in healthcare. They improve the lives of those with musculoskeletal disorders. They work with other doctors to find the best treatment for each patient.
For example, they might follow guidelines from professional associations. This ensures patients get the best care based on evidence.
Education and Training of Orthopedic Specialists
Orthopedic specialists go through a lot of education and training. After medical school, they do several years of residency. This hands-on training helps them diagnose and treat musculoskeletal issues.
Many also do fellowship training in areas like sports medicine or spine surgery. This advanced training keeps them up-to-date with the latest treatments.
| Education/Training Level | Description | Duration |
|---|---|---|
| Medical School | Foundational education in medicine | 4 years |
| Residency Training | Hands-on experience in orthopedic surgery | 5 years |
| Fellowship Training | Specialized training in a specific area of orthopedics | 1-2 years |
What Does an Orthopedic Doctor Treat? A Complete Overview

Orthopedic doctors focus on treating many conditions of the musculoskeletal system. This system includes bones, joints, muscles, ligaments, and tendons. These parts work together to support, stabilize, and move the body.
The Musculoskeletal System: Bones, Joints, Muscles, Ligaments, and Tendons
The musculoskeletal system is complex. It has different parts that can be affected by various conditions. Bones form the body’s structure, while joints allow for movement and flexibility. Muscles, ligaments, and tendons help with motion and keep joints stable.
The American Academy of Orthopaedic Surgeons says, “The musculoskeletal system is a complex system that allows for movement, maintains posture, and produces body heat.”
“Understanding the musculoskeletal system is key to diagnosing and treating orthopedic conditions effectively.”
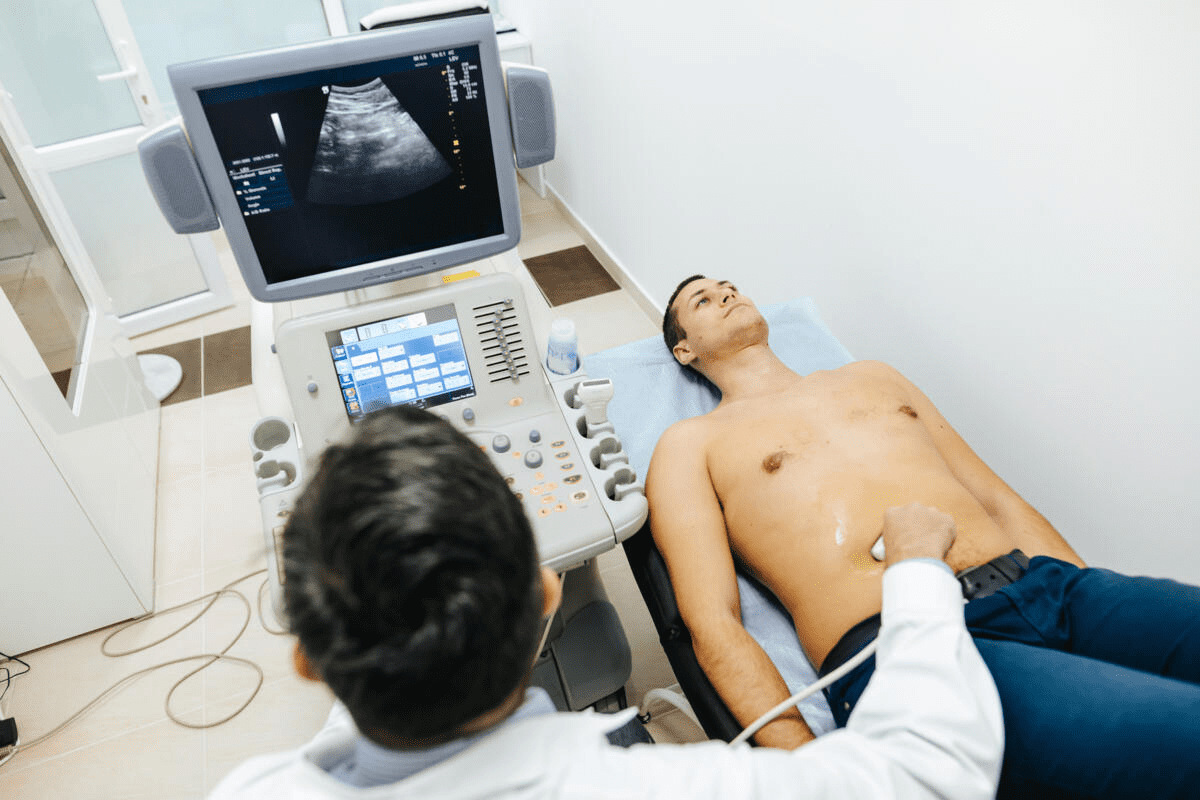
Diagnostic Methods Used by Orthopedic Specialists
Orthopedic specialists use many diagnostic methods to find and check musculoskeletal conditions. These include:
- Medical History: A detailed look at the patient’s medical history to find any past conditions or injuries.
- Physical Examination: A full physical exam to check joint mobility, muscle strength, and overall musculoskeletal function.
- Imaging Tests: X-rays, CT scans, MRI scans, and other imaging to see bones, joints, and soft tissues.
- Diagnostic Injections: Injections of anesthetics or corticosteroids into joints or soft tissues to find the pain source.
By using these methods, orthopedic specialists can accurately diagnose and create effective treatment plans for many musculoskeletal conditions.
“Accurate diagnosis is the foundation of effective treatment in orthopedic care,” highlights the need for detailed diagnostic evaluation in orthopedic medicine.
Condition #1: Arthritis and Joint Inflammation
It’s important to know about arthritis and joint inflammation to manage symptoms and improve life quality. Arthritis includes over 100 conditions that affect joints and tissues. We’ll look at osteoarthritis and rheumatoid arthritis, the most common types.
Osteoarthritis vs. Rheumatoid Arthritis: Differences and Similarities
Osteoarthritis (OA) is the most common arthritis type. It happens when cartilage in joints breaks down. This leads to pain, stiffness, and less mobility.
Rheumatoid arthritis (RA) is an autoimmune disease. It causes inflammation in joints, which can lead to serious damage if not treated.
OA is mainly caused by aging and wear and tear. RA is caused by an abnormal immune response. Both can greatly affect a person’s life quality.
Modern Treatment Approaches for Arthritis Patients
Arthritis treatment has improved, with options for each type and severity. For OA, treatments include lifestyle changes, physical therapy, and pain meds. In severe cases, surgery like joint replacement might be needed.
For RA, treatments focus on slowing the disease and preventing damage. Disease-modifying antirheumatic drugs (DMARDs) are key. Newer biologic agents also help manage symptoms and improve outcomes.
| Condition | Primary Characteristics | Common Treatment Approaches |
|---|---|---|
| Osteoarthritis (OA) | Degenerative joint disease, cartilage breakdown | Lifestyle modifications, physical therapy, pain management, surgery |
| Rheumatoid Arthritis (RA) | Autoimmune disease, joint inflammation | DMARDs, biologic agents, lifestyle changes |
Understanding OA and RA helps doctors create specific treatment plans. Our orthopedic specialists work with patients to make personalized care plans. This ensures the best results for each patient.
Condition #2: Fractures and Traumatic Bone Injuries
Orthopedic specialists are key in diagnosing and treating fractures and traumatic bone injuries. These breaks in bones can happen from accidents, falls, or sports injuries. The severity of fractures varies based on their location, type, and how severe they are.
Types of Fractures and Their Classification
Fractures are sorted by several factors like where they are, the break’s pattern, and if the bone shows through the skin. The main fracture types include:
- Closed Fracture: The bone is broken, but the skin stays intact.
- Open Fracture: The bone breaks through the skin, raising infection risks.
- Comminuted Fracture: The bone breaks into many pieces.
- Displaced Fracture: The bone is broken, and the pieces are not in the right place.
- Stress Fracture: Small cracks in the bone, often from repetitive stress or overuse.
The Healing Process and Orthopedic Interventions
The healing of fractures goes through stages like inflammation, soft callus, hard callus, and remodeling. Orthopedic care is vital for proper healing and function. Treatment options include:
| Treatment Option | Description |
|---|---|
| Casting | Immobilizing the affected limb with a cast to allow healing. |
| Surgery | Realignment and stabilization of the bone fragments using plates, screws, or rods. |
| Physical Therapy | Rehabilitation exercises to regain strength and mobility. |
Knowing the type and severity of a fracture is key for the right treatment. Orthopedic specialists work with patients to create a treatment plan that helps in healing and recovery.
Condition #3: Spine Disorders and Back Pain
Understanding spine disorders is key to tackling back pain. Back pain is a big health issue that many people face. In the U.S., millions of adults live with chronic back or neck pain. This can really hurt their daily life and work.
Common Spinal Conditions: Herniated Discs, Stenosis, and Scoliosis
There are several spinal conditions linked to back pain. These include:
- Herniated Discs: Happens when the soft center of the disc leaks out through a tear.
- Spinal Stenosis: This is when the spinal canal gets too narrow, pressing on nerves.
- Scoliosis: A spine that curves to one side, often found in teens.
These issues can cause a lot of pain. If it’s bad, you might need to see a doctor.
Conservative and Surgical Management Options
First, doctors try non-surgical ways to help. These include:
- Physical Therapy: Helps move better and strengthen the spine’s muscles.
- Pain Management: Uses medicine and other methods to control pain.
- Lifestyle Modifications: Like staying at a healthy weight and good posture.
If these don’t work, surgery might be needed. Surgery can be simple or complex, like spinal fusion.
Choosing between non-surgical and surgical options depends on the condition, how bad it is, and your health.
Condition #4: Joint Dislocations and Instability
Understanding joint dislocations is key to effective treatment and recovery. Joint dislocations happen when bones in a joint move out of place. This can lead to instability and long-term problems if not treated right.
Shoulder, Hip, and Other Common Joint Dislocations
Joint dislocations can occur in many parts of the body. The shoulder and hip are most at risk. The shoulder, being very mobile, is also very unstable, making it prone to dislocations.
Hip dislocations, often caused by big impacts, are hard to treat because of the joint’s deep location. Other joints, like the elbow, knee, and ankle, can also get dislocated. Each has its own causes and treatment challenges.
A study in the Journal of Orthopaedic Trauma found that posterior hip dislocations have a higher risk of complications. This shows the need for quick and proper care.
Treatment Protocols and Rehabilitation Approaches
Treating joint dislocations includes immediate care to put the bones back in place and long-term rehab to make the joint stable again. First, doctors might do a closed reduction, where they move the bones back without surgery. Then, they might immobilize the joint to help it heal.
Rehab is a big part of getting better, focusing on strength, motion, and stability. Physical therapy is key, with exercises made for the specific joint and person. For example, shoulder rehab might strengthen the rotator cuff muscles, while hip rehab might focus on stabilizing the hip.
Key Components of Rehabilitation:
- Range of motion exercises to improve flexibility
- Strengthening exercises to support the joint
- Proprioceptive training to enhance joint awareness
- Functional training to return to daily activities and sports
Orthopedic specialists say, “A well-structured rehab program is essential for preventing recurrent dislocations and ensuring the long-term health of the joint.” (
Rehabilitation after joint dislocation is not just about recovering from the immediate injury but also about preventing future instability.
)
| Joint | Common Causes of Dislocation | Treatment Approaches |
|---|---|---|
| Shoulder | Falls, sports injuries | Closed reduction, physical therapy |
| Hip | High-impact trauma, accidents | Surgical reduction, rehabilitation |
| Elbow | Falls, hyperextension | Closed reduction, immobilization |
Condition #5: Sprains, Strains, and Soft Tissue Injuries
It’s important to know the difference between sprains, strains, and other soft tissue injuries. These injuries are common and can really affect someone’s life.
Differentiating Between Ligament Sprains and Muscle Strains
Ligament sprains and muscle strains are two different injuries. Ligament sprains happen when a ligament gets stretched or torn, usually near a joint. Muscle strains happen when a muscle gets stretched or torn.
The symptoms of sprains and strains can be similar. They include pain, swelling, and trouble moving. But, the pain’s location can tell you which one it is. Sprains hurt right over the joint, while strains hurt in the muscle itself.
RICE Protocol and Advanced Recovery Techniques
The RICE protocol is a common way to treat sprains and strains. RICE means Rest, Ice, Compression, and Elevation.
- Rest: Stay away from activities that make the injury worse.
- Ice: Use ice to lessen pain and swelling.
- Compression: Use a bandage or wrap to squeeze the injured area.
- Elevation: Keep the injured limb higher than your heart.
For more serious injuries, treatments like physical therapy, bracing, or surgery might be needed. The right treatment depends on how bad the injury is.
| Treatment Approach | Description | Applicability |
|---|---|---|
| RICE Protocol | Initial treatment for acute injuries | All soft tissue injuries |
| Physical Therapy | Rehabilitation and strengthening | Moderate to severe injuries |
| Bracing | Support and stability | Joint-related injuries |
| Surgical Intervention | Repair of severe tears or damage | Severe injuries or chronic conditions |
Condition #6: Tendonitis, Bursitis, and Inflammatory Conditions
Many patients face tendonitis, bursitis, and other inflammatory issues. These problems cause pain and discomfort. It’s important to know the causes, symptoms, and treatments to manage them well.
Common Sites of Inflammation
Tendonitis and bursitis can happen in different parts of the body. The elbow (tennis elbow), Achilles tendon, and shoulder (shoulder bursitis) are common areas. Each condition needs a specific treatment plan.
Tennis Elbow (Lateral Epicondylitis) causes pain on the outer elbow. It’s often due to repetitive strain. Achilles Tendonitis affects runners and athletes, causing inflammation in the Achilles tendon. Shoulder Bursitis leads to pain and less mobility in the shoulder.
Anti-inflammatory Approaches and Specialized Treatments
Dealing with tendonitis, bursitis, and other inflammatory conditions needs a mix of treatments. First, rest, ice, compression, and elevation (RICE) are used. Anti-inflammatory drugs are also part of the initial treatment.
For more severe cases, corticosteroid injections, physical therapy, and sometimes surgery are considered. Physical therapy helps in getting strength and flexibility back. Corticosteroid injections help by reducing inflammation.
| Condition | Common Symptoms | Typical Treatments |
|---|---|---|
| Tennis Elbow | Pain on outer elbow, weakened grip | RICE, physical therapy, corticosteroid injections |
| Achilles Tendonitis | Pain along Achilles tendon, swelling | RICE, physical therapy, orthotics |
| Shoulder Bursitis | Shoulder pain, reduced mobility | RICE, physical therapy, corticosteroid injections |
In conclusion, treating tendonitis, bursitis, and other inflammatory conditions needs a detailed plan. Understanding the causes and symptoms helps healthcare providers manage these conditions effectively. This approach helps reduce pain and improves function.
Condition #7: Osteoporosis and Bone Density Issues
Osteoporosis and bone density problems often go unnoticed until a bone breaks. This shows why we need to be aware and take steps to prevent it. Osteoporosis makes bones weak, leading to more breaks. We’ll look at the risks, how to screen for it, and ways to keep bones healthy.
Risk Factors, Screening, and Early Detection
Knowing the risks for osteoporosis is key to acting early. These risks include age, gender, family history, and lifestyle choices like diet and exercise. A bone density test is used to screen for osteoporosis. Finding it early helps prevent breaks.
Key risk factors include:
- Age over 65
- Female gender
- Family history of osteoporosis or fractures
- Low body weight
- Lifestyle factors such as smoking and excessive alcohol consumption
Comprehensive Management of Bone Health
Improving bone health requires a mix of lifestyle changes, nutrition, and sometimes medicine. Lifestyle changes like exercise and a balanced diet are important. They help keep bones strong.
Nutritional interventions are also vital. They might include supplements if food alone isn’t enough. Medications like bisphosphonates help by making bones stronger.
Condition #8: Sports Injuries and Athletic Performance Issues
Sports injuries can stop athletes from playing, affecting their careers and health. These issues are a big worry for athletes, coaches, and doctors. Injuries can hurt athletes’ performance now and their future health and career.
Common Sports-Related Injuries: ACL Tears, Meniscus Damage, and Rotator Cuff Injuries
Sports injuries can happen anywhere in the body. ACL tears are common in sports that need quick stops and changes, like soccer and basketball. Meniscus damage often comes from twisting or direct hits. Rotator cuff injuries happen in sports that use the arms a lot, like baseball and tennis.
Knowing about these injuries helps in finding the right treatment. For example, ACL tears might need surgery and a long rehab to fix the knee. Meniscus damage might get treated with surgery or just rest, based on the injury. Rotator cuff injuries can be mild or severe, needing different treatments like physical therapy or surgery.
Return-to-Play Protocols and Performance Optimization
After an injury, athletes follow a return-to-play plan to safely get back to sports. This plan checks their strength, flexibility, and function. Return-to-play protocols help prevent more injuries and make sure athletes are ready for their sport.
Also, performance optimization is key for athletes to get back to their best. This includes personalized training programs to strengthen the injury area and improve overall fitness. By combining sports medicine with athletic training, athletes can perform well and stay injury-free.
When to See an Orthopedic Doctor: Signs and Referral Process
Orthopedic doctors are key in treating bone, joint, and muscle issues. But how do you know when to see one? It’s important to see an orthopedic specialist for effective treatment of musculoskeletal conditions.
Recognizing Symptoms That Require Specialist Care
Certain symptoms mean you need to see an orthopedic specialist. These include:
- Persistent pain or stiffness in bones or joints
- Limited mobility or difficulty performing daily activities
- Recent injuries or trauma to the musculoskeletal system
- Deformity or abnormal shape of a limb or joint
- Chronic conditions like arthritis or osteoporosis
If you’re experiencing these symptoms, seeing an orthopedic doctor is a good idea. Primary care providers often refer you to specialists if needed.
| Symptom | Possible Condition | Specialist Care |
|---|---|---|
| Persistent joint pain | Osteoarthritis, Rheumatoid Arthritis | Orthopedic consultation for diagnosis and treatment |
| Recent bone injury | Fracture, Dislocation | Immediate orthopedic care for assessment and intervention |
| Chronic back pain | Herniated disc, Spinal stenosis | Orthopedic or spinal specialist consultation |
What to Expect During Your First Orthopedic Consultation
At your first visit, the doctor will do a detailed check-up. This includes:
- Medical history review
- Physical examination
- Imaging tests (X-rays, MRI, CT scans) if necessary
The doctor will then talk about your diagnosis, treatment options, and lifestyle changes. Treatment might include physical therapy, surgery, or other options based on your condition.
Preparing for Your Visit
To get the most from your visit, consider the following:
- Bring any relevant medical records or test results
- List your symptoms and when they occur
- Note any medications or supplements you’re taking
Knowing when to seek orthopedic care and what to expect can help you manage your musculoskeletal health. If you’re unsure about your symptoms or need help with the referral process, talk to a healthcare professional.
Conclusion: The Evolving Field of Orthopedic Medicine
The field of orthopedic medicine is changing fast. New technology and treatments are leading the way. We’re seeing big steps forward in orthopedic care, like new surgery methods and custom rehab plans.
Orthopedic care is getting better thanks to new tools and techniques. Doctors can now diagnose and treat musculoskeletal problems more accurately. This means patients get help sooner and more effectively.
Orthopedic medicine is getting even better, with new ways to treat arthritis, fractures, and spine issues. Orthopedic experts are always learning and using the latest methods. This helps patients get the best care and live better lives.
If you have a sports injury or a degenerative condition, seeing an orthopedic specialist is key. They offer targeted and effective treatments. We urge you to take care of your musculoskeletal health and check out the newest treatments.
FAQ
What does an orthopedic doctor do?
Orthopedic doctors diagnose and treat bone, joint, and muscle problems. They help with issues like fractures and arthritis.
What is the role of orthopedic doctors in healthcare?
We help patients move better and feel less pain. Our goal is to improve their quality of life.
What kind of conditions do orthopedic doctors treat?
We treat many conditions. This includes arthritis, fractures, and sports injuries. We also help with joint problems and muscle strains.
What is orthopedic medicine, and what does it entail?
Orthopedic medicine deals with musculoskeletal disorders. It uses surgery and non-surgical treatments to help patients.
When should I see an orthopedic doctor?
See us if you have ongoing pain or limited movement. Also, if you’ve had a sports injury or trauma.
What can I expect during my first orthopedic consultation?
At your first visit, we’ll examine you and review your medical history. We might also do tests to find out what’s wrong and create a treatment plan.
What are some common diagnostic methods used by orthopedic specialists?
We use X-rays, MRI, CT scans, and physical exams. These help us find the cause of your symptoms and plan your treatment.
Can orthopedic doctors help with sports-related injuries?
Yes, we specialize in treating sports injuries. We help athletes recover and get back to their sport safely.
What are some modern treatment approaches for arthritis patients?
We offer many treatments for arthritis. This includes medication, physical therapy, injections, and surgery. Our goal is to reduce pain and improve joint function.
How can I promote bone health and prevent osteoporosis?
Eat well, exercise regularly, and prevent falls. We also recommend screenings and early detection to keep your bones healthy.
References
- MedlinePlus. (2024, June 17). Orthopedic services. Retrieved October 17, 2025, from https://medlineplus.gov/ency/article/007455.htm