Last Updated on October 31, 2025 by
Understanding carcinoma in situ is key for patients and doctors to spot early cancer. We aim to give top care and support to patients from around the world.
Carcinoma in situ, or “in its original place,” means abnormal cells that haven’t spread. This stage 0 cancer is not invasive and is often found through screenings.
At places like Liv Hospital, we use the latest screening methods. Our focus is on caring for patients with cancer in situ effectively.
The Origin and Meaning of “In Situ” in Cancer Terminology

The Latin phrase “in situ” means “in its original place.” This idea is key to understanding early-stage cancer.
The term “in situ” comes from Latin, meaning “in its original place” or “in its place.” It’s very important in cancer talk. It shows cancers that stay in their original spot without spreading to other tissues.
The word “in situ” became a big deal in medicine. It shows how vital it is to know where cancer cells start. This term helps doctors sort cancers by how serious they are.
Using “in situ” in medical writing highlights cancers that don’t spread. It means the cancer is in its early stages and hasn’t reached deeper tissues yet.
For a long time, “in situ” was seen as stage 0 cancer. This was a big deal in how doctors classify cancer. It shows how important catching cancer early is.
| Stage | Description | Characteristics |
| Stage 0 | Carcinoma in situ | Cancer cells are confined to the epithelium |
| Stage I | Early invasive cancer | Cancer has begun to invade deeper tissues |
What Does In Situ Mean in Cancer? Understanding Stage 0

In situ cancer, or stage 0 cancer, is a key stage in cancer growth. At this point, abnormal cells are there but haven’t spread to other tissues. Knowing about in situ cancer helps patients make smart choices about their treatment.
Carcinoma in situ, or stage 0 cancer, means abnormal cells are present but haven’t moved. It’s a non-invasive condition, meaning it hasn’t reached nearby tissues or organs. The main thing about in situ cancer is that it stays in the layer where the cells first appeared.
Spotting in situ cancer early is very important. It lets doctors act fast, which can stop cancer from becoming worse. Treatment at this stage often leads to good results.
The main difference between in situ and invasive cancer is how far the cells have spread. In situ cancer stays in one place, while invasive cancer has spread to other areas. Knowing this helps doctors choose the right treatment and predict how well it will work.
In situ cancer is called stage 0, while invasive cancers are stages 1 to 4. It’s key for patients to understand this to know what treatment they need.
Finding in situ cancer early makes treatment much more effective. Regular screenings and check-ups help catch cancer early. Early detection means in situ cancer can often be treated well, stopping it from becoming invasive.
Being aware and educated about cancer screening is very important. Knowing how early detection helps can encourage people to watch their health closely and get medical help when needed.
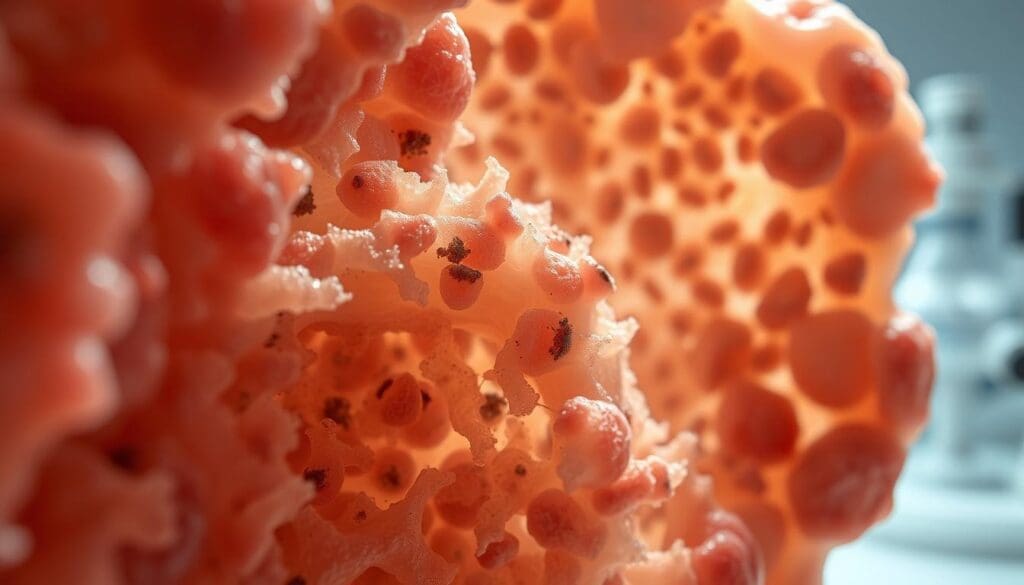
Carcinoma in situ involves complex changes in cells and molecules. These changes can lead to invasive cancer if not treated. The cells are not yet cancerous but can become so if left untreated.
Carcinoma in situ shows abnormal cell growth in the epithelial layer. This growth includes changes in cell shape, more cell division, and genetic mutations. Doctors can spot these changes through tests like histopathology.
The cells in carcinoma in situ stay in the epithelial layer. They don’t break through the basement membrane or deeper tissues. This is important because it means we can catch it early and treat it before it spreads.
Molecular markers and genetic changes are key in carcinoma in situ. These changes help doctors diagnose and track the condition. Knowing about these changes helps predict if the cancer will spread.
Some of the molecular markers associated with carcinoma in situ include:
Understanding carcinoma in situ’s biology helps us diagnose and manage it better. This can stop it from becoming invasive cancer.
In situ carcinomas come in several types, each with its own traits and treatment needs. Knowing about these types helps doctors choose the best treatment. This improves how well patients do.
Ductal carcinoma in situ (DCIS) is a common breast cancer type. It has abnormal cells in the milk ducts but doesn’t spread. It’s often found by mammograms and can be treated early.
About 56,000 people in the U.S. get DCIS each year. This shows how important it is in breast cancer.
Lobular carcinoma in situ (LCIS) affects the lobules of the breast. It’s seen as a sign of higher risk of breast cancer, not a true cancer. Women with LCIS are watched closely for any changes.
Cervical carcinoma in situ means abnormal cells on the cervix that haven’t spread. It’s found by Pap smears and treated with LEEP.
There are other in situ carcinomas like melanoma in situ and colorectal carcinoma in situ. These affect different parts of the body.
Each in situ carcinoma has its own features and treatment plans. Knowing about them is key to giving the right care and improving patient results.
It’s important to understand in situ cancers to improve screening and treatment. These cancers are abnormal cell growths that haven’t spread. They are seen as pre-cancerous or early-stage cancers.
In the United States, in situ cancers are common. Ductal carcinoma in situ (DCIS) affects about 56,000 people each year. It’s a breast cancer where cells are in the ducts but haven’t spread.
Lobular carcinoma in situ (LCIS) also increases breast cancer risk. Women with LCIS have a 25% to 30% chance of getting breast cancer in 20-25 years.
In situ cancers can happen to anyone, but some groups are at higher risk. Age, family history, genetic mutations, and radiation exposure are key risk factors.
Knowing these patterns and risks helps target screening and prevention. For example, women with a family history of breast cancer might need more frequent screening.
More in situ cancers are being diagnosed, thanks to better screening and awareness. Mammography has helped find more DCIS cases.
While more diagnoses are good, it also means more work in treating these cancers. The aim is to treat them well without overdoing it.
Progression Potencial: From In Situ to Invasive Cancer
In situ carcinomas can turn into invasive cancer, but the chance varies by cancer type. Knowing this is key for picking the right treatment and follow-up for patients.
The chance of in situ carcinomas becoming invasive cancer is not the same for all. For example, ductal carcinoma in situ (DCIS) might turn into invasive ductal carcinoma in up to 50% of cases over 10 years. On the other hand, lobular carcinoma in situ (LCIS) is seen as a risk marker, not a true precursor, and tends to grow slower.
Some in situ lesions, like certain colon polyps, will always become invasive if not treated. This shows how critical it is to get an accurate diagnosis and understand the risk level.
Several things can tell us if an in situ carcinoma will turn malignant. These include:
Knowing these predictive factors helps doctors create treatment plans tailored to each patient.
The time it takes for in situ carcinomas to become invasive cancer varies a lot. Some stay the same for years, while others change quickly. For instance, high-grade DCIS can turn into invasive cancer in just a few years. But LCIS might take decades to possibly become invasive lobular carcinoma.
It’s important to keep an eye on patients with in situ carcinomas over time. This way, treatment plans can be adjusted if needed.
Diagnosing in situ carcinomas requires several methods. These include screening protocols and molecular testing. Finding these pre-cancerous conditions early is key to treating them before they become invasive cancer.
Screening is the first step in finding in situ carcinomas. For example, mammograms help spot ductal carcinoma in situ (DCIS) before symptoms show up. A study shows that screening tests, like mammograms, can find DCIS early, which is very important.
“The implementation of organized screening programs has been shown to reduce breast cancer mortality by detecting cancers at an early stage.” –
Regular screening leads to early detection of in situ carcinomas. This improves treatment results. It’s important to follow screening guidelines to catch these conditions early.
Imaging is vital in diagnosing in situ carcinomas. Mammography, ultrasound, and MRI are the main imaging tools.
Each imaging method has its own benefits. The choice depends on the cancer type and the patient’s situation. For instance, MRI is great for checking how far DCIS has spread.
Biopsy is the top method for diagnosing in situ carcinomas. It involves examining tissue samples to see if there are abnormal cells. These cells must be in the epithelial layer.
A biopsy not only confirms the diagnosis. It also tells us about the carcinoma’s grade and type. This helps doctors decide on the best treatment.
Molecular and genetic testing are becoming more common. They help figure out the risk of cancer spreading and guide treatment. These tests look for specific genetic markers in in situ carcinomas.
Knowing the genetic makeup of the carcinoma helps doctors tailor treatments. This approach can lead to better patient outcomes.
There are many ways to treat in situ cancers, from surgery to more gentle methods. The right treatment depends on the cancer type, where it is, and the patient’s health.
Surgery is a common first step for many in situ cancers. For example, melanoma in situ is often treated with wide local excision. This removes the cancer and some healthy tissue around it.
Ductal carcinoma in situ (DCIS) might get lumpectomy followed by radiation, or sometimes mastectomy.
Studies show surgery can be very effective for in situ cancers. For instance, a study on DCIS found removing the cancer with clear margins lowers recurrence risk.
| Type of In Situ Cancer | Common Surgical Treatments |
| Melanoma In Situ | Wide Local Excision |
| Ductal Carcinoma In Situ (DCIS) | Lumpectomy, Mastectomy |
| Cervical Carcinoma In Situ | LEEP (Loop Electrosurgical Excision Procedure), Conization |
Radiation therapy is used after surgery for in situ cancers. It helps kill any cancer cells left behind. For DCIS, radiation after lumpectomy cuts down the chance of cancer coming back.
“Radiation therapy after lumpectomy for DCIS significantly reduces the risk of local recurrence, providing a valuable treatment option for patients.”
For some in situ cancers, medicines or hormonal treatments are suggested. For example, tamoxifen might be given to DCIS patients to lower the risk of invasive breast cancer.
Active surveillance is sometimes recommended. It means watching the cancer closely with tests and exams. This is often for patients with low-risk cancers.
It’s important to know about the different treatments for in situ cancers. Talking to your doctor helps choose the best treatment for you.
Prognosis and Survival Rates for In Situ Carcinomas
In situ carcinomas have a good prognosis if caught early. These cancers grow in the top layer of cells and don’t spread. Early detection through screenings leads to high survival rates.
Survival rates for in situ carcinomas depend on the cancer type and location. For example, ductal carcinoma in situ (DCIS) of the breast has a high survival rate. Studies show a 98% to 99% 10-year survival rate with proper treatment.
Cervical carcinoma in situ also has a good prognosis if treated early. This reduces the risk of invasive cervical cancer. Lobular carcinoma in situ (LCIS) increases breast cancer risk, but it’s not a true cancer. It’s a marker for higher risk, and management focuses on reducing this risk.
Several factors can change the prognosis of in situ carcinomas. These include the cancer type, location, patient health, and treatment effectiveness. Molecular markers or genetic mutations can also play a role. Patient compliance with treatment and follow-up is key.
Age and health are also important. Younger patients with fewer health issues tend to have better outcomes. The psychological impact of a cancer diagnosis is also significant, affecting mental health and treatment adherence.
Long-term monitoring is vital for managing in situ carcinomas. Regular check-ups and screenings help catch any recurrence or progression early. For example, women with DCIS or LCIS need regular mammograms and breast exams.
Monitoring frequency and type depend on individual risk factors and cancer characteristics. Healthcare providers create personalized follow-up plans for each patient’s needs and risk profile.
Psychological Impact of an In Situ Cancer Diagnosis
An in situ cancer diagnosis can stir up a mix of feelings and doubts for patients. The term “in situ” means “in its original place.” It can offer relief but also cause worry, as it shows the cancer hasn’t spread but needs attention.
The term “in situ carcinoma” can affect a patient’s mind in different ways. Some doctors see it as a non-invasive cancer, while others view it as an early cancer. This can lead to confusion and worry for patients.
For example, a diagnosis of ductal carcinoma in situ (DCIS) can be seen differently by patients. Some might see it as a condition to watch, while others might think it’s an early cancer needing treatment. This difference in views can impact a patient’s mental health.
Dealing with an in situ cancer diagnosis needs a variety of strategies. Patients can find help through counseling, support groups, and educational materials. These tools help patients understand their condition, manage their anxiety, and make informed choices about treatment.
Healthcare providers are key in guiding and supporting patients. They offer clear information and emotional support, helping patients face the challenges of an in situ cancer diagnosis.
Patients with in situ carcinoma often face tough decisions about treatment. Choosing between active surveillance, surgery, or other treatments can be overwhelming, as the risks and benefits are not always clear.
| Treatment Option | Benefits | Considerations |
| Active Surveillance | Avoids immediate intervention, monitors progression | Requires regular check-ups, possible progression |
| Surgery | Removes the affected area, lowers risk of progression | Risks of surgery, possible overtreatment |
| Radiation Therapy | Reduces risk of recurrence after surgery | Side effects, impact on surrounding tissue |
Understanding the diagnosis, treatment options, and outcomes is key to making informed decisions. Patients should talk to their healthcare providers about their concerns and options. This way, they can find the best treatment for their situation.
The field of in situ cancer research has seen big steps forward. This brings new hope for patients and doctors. Research aims to better diagnose and treat in situ carcinomas. It focuses on treatments that are tailored and precise.
New studies have led to new ways to classify in situ cancers. This makes diagnosis and treatment planning more accurate. These new systems consider genetic mutations and molecular markers.
New ways to treat in situ cancers are changing how we manage them. These include:
Precision medicine is becoming more common in treating in situ cancers. It tailors treatment to each patient’s cancer. This could lead to more effective and less invasive treatments.
Research into the genetics and molecules of in situ cancers is driving precision medicine. As we learn more about these cancers, we can develop better treatments.
Conclusion: The Importance of Understanding In Situ Cancer
Knowing about in situ carcinoma is key for catching it early. This can stop it from becoming invasive cancer. By learning about its definition, traits, and treatments, people can protect their health.
Acting fast on in situ carcinoma can lead to better results. Studies prove that quick action can stop it from becoming invasive. This shows why knowing about it is so vital.
In situ cancers are different, each needing its own approach. Understanding these differences helps doctors and patients work together. This leads to the best care possible.
It’s very important to know about in situ cancer. We hope this info helps people take charge of their health. They should seek early detection and treatment when needed.
“In situ” comes from Latin and means “in its original place.” In cancer, it means abnormal cells that haven’t spread. This shows it’s a non-invasive or stage 0 cancer.
Carcinoma in situ, or stage 0 cancer, is the earliest form of cancer. It hasn’t spread to other tissues. It’s about abnormal cell growth in the epithelial layer.
Carcinoma in situ is non-invasive and stays in its original place. Invasive cancer spreads to other tissues. Knowing this difference helps choose the right treatment.
There are several types, like ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS). Cervical carcinoma in situ is another. Other types can happen in different organs.
Doctors use screening, imaging, biopsy, and lab tests to diagnose it. They might also do molecular and genetic testing. This helps decide the best treatment.
Yes, it can turn into invasive cancer. How likely it is depends on the type and other factors.
Treatment depends on the type, location, and patient’s health. Options include surgery, radiation, medication, hormonal treatments, or watching it closely.
The outlook is good, mainly if caught and treated early. Long-term checks are often needed to watch for any signs of it coming back.
Patients might feel anxious and unsure. They need support and ways to cope with the emotional impact.
New research includes better classification systems and treatments. Precision medicine is also being explored. The goal is to improve diagnosis and treatment for each patient.
Knowing about in situ cancer helps catch it early. This can stop it from becoming invasive. It helps people make informed health choices and lowers the risk of cancer getting worse.
National Center for Biotechnology Information. (2025). What Does In Situ Mean in Cancer Complete. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5161057/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!