Last Updated on November 27, 2025 by Bilal Hasdemir
When your doctor says you have a mildly calcified aortic valve, it might seem like a small issue. But, it can quietly affect your heart health over time.
At Liv Hospital, we offer clear and caring care. We know a calcified heart valve is a serious issue that impacts the
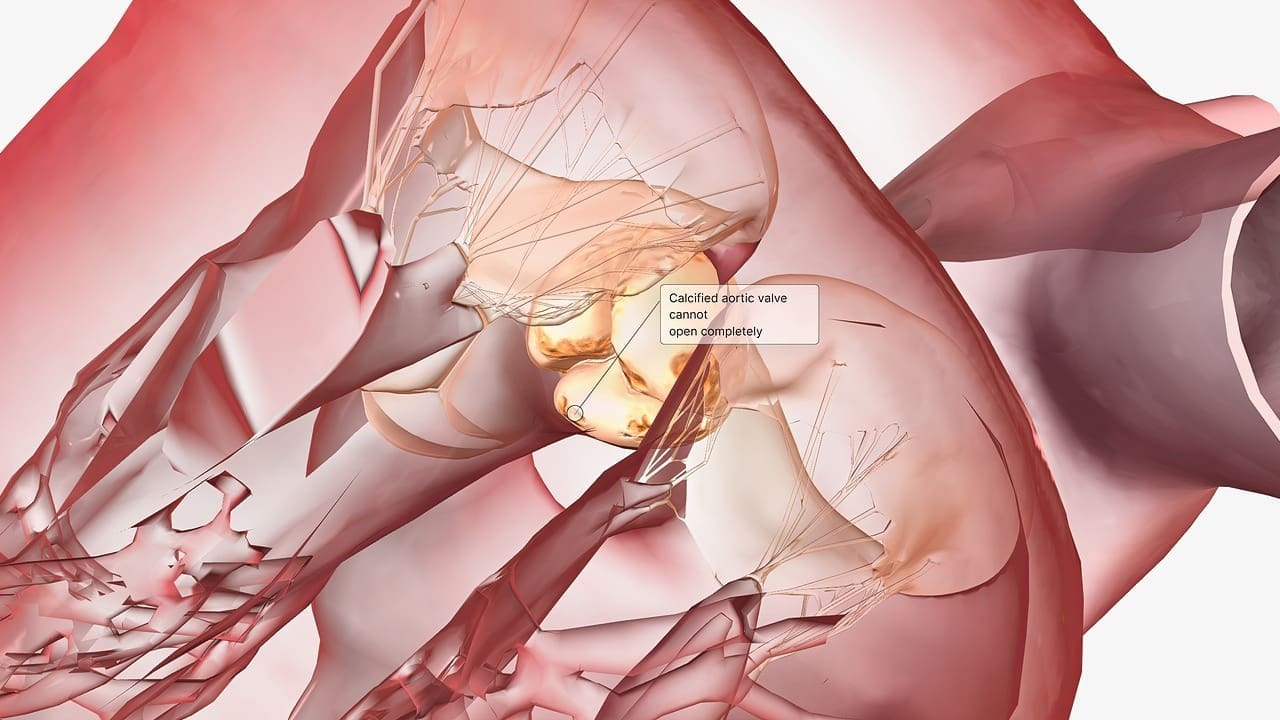
Aortic valve calcification happens when calcium builds up on the valve, making it hard. This can block blood flow and cause serious problems if not treated.
Understanding heart valve function is key to knowing how valve calcification affects heart health. The heart has four valves. These valves work together to ensure blood flows well throughout the body.
The heart’s four valves are the mitral, tricuspid, pulmonary, and aortic valves. The mitral and tricuspid valves manage blood flow between the heart’s chambers. The pulmonary and aortic valves control blood flow to the lungs and the rest of the body, respectively.
| Valve Name | Location | Function |
|---|---|---|
| Mitral Valve | Between left atrium and ventricle | Controls blood flow between left chambers |
| Tricuspid Valve | Between right atrium and ventricle | Controls blood flow between right chambers |
| Pulmonary Valve | Between right ventricle and pulmonary artery | Regulates blood flow to lungs |
| Aortic Valve | Between left ventricle and aorta | Regulates blood flow to the body |
For blood to circulate efficiently, valves must function correctly. When a valve calcifies, it can’t open and close right. This can cause serious health problems.
Calcification of the heart valve happens when calcium builds up on the valve, making it hard. This can affect how well the valve works. It might even cause problems like valve stenosis.
A calcified heart valve means calcium has built up on the valve, making it stiff. This can mess up how the valve opens and closes. It’s like when you try to open a door that’s stuck.
Many things can cause calcium to build up on the valve. These include getting older, your genes, and some health issues. As more calcium forms, the valve gets stiffer. This makes it harder for the heart to pump blood well.
Calcification and stenosis are not the same, even though they’re related. Calcification is when calcium builds up on the valve. Stenosis is when the valve opening gets too narrow. Not all calcification leads to stenosis, though.
| Condition | Description | Impact on Valve |
|---|---|---|
| Calcification | Accumulation of calcium deposits | Hardening of the valve |
| Stenosis | Narrowing of the valve opening | Impaired blood flow |
The aortic valve is key to heart health. It lets blood flow from the heart to the aorta. This ensures oxygen-rich blood reaches the body’s parts well.
The aortic valve has three cusps that open and close. This structure is vital for normal valve work. Proper valve function stops backflow and lets blood flow one way, from heart to aorta.
The aortic valve is vital for cardiovascular health. It keeps blood flowing well. But, calcification can harm this, causing mild aortic valve sclerosis and severe problems.
Knowing the aortic valve’s role in heart health is important. It shows why keeping it working right is key. And why fixing valve calcification issues is urgent.
The aortic valve calcification is caused by age, genetics, and medical conditions. As we get older, the risk of this condition grows.
Age is a big risk factor for aortic valve calcification. Older adults are more likely to have it because of valve wear. Studies show that more elderly people are affected by this condition.
Genetics also play a part in aortic valve calcification. People with a family history of heart diseases are at higher risk. Some genetic conditions can make the valve more prone to calcification.
Medical conditions like hypertension and kidney disease can lead to aortic valve calcification. Knowing these causes helps in preventing and managing the condition.
| Cause | Description | Impact |
|---|---|---|
| Age-Related Wear | Wear and tear on the aortic valve over time | Increased risk with age |
| Genetic Predisposition | Family history and genetic conditions | Higher likelihood of calcification |
| Hypertension | High blood pressure | Increased risk of calcification |
Aortic valve calcification is caused by different risk factors. These can be changed or are fixed. Knowing these factors helps in catching and treating the condition early.
Modifiable risk factors are things we can change. They include lifestyle choices and some health conditions.
Non-modifiable risk factors are things we can’t change. They include age and genetics.
| Risk Factor Category | Specific Risk Factors |
|---|---|
| Modifiable | Smoking, High Blood Pressure, High Cholesterol |
| Non-Modifiable | Age, Genetic Predisposition |
By understanding and tackling these risk factors, we can manage aortic valve calcification better.
Aortic valve calcification gets worse over time, moving through different stages. Each stage has its own signs and affects health differently. Knowing these stages helps doctors choose the right treatment.
At first, small calcium spots start on the valve. The valve works okay, and people might not feel sick. But, it’s important to watch it closely to see how it changes.
When it gets worse, more calcium builds up, making the valve stiff. This can make it harder for the valve to open, causing symptoms like breathing trouble or feeling tired. Regular doctor visits are key to keeping track and adjusting treatment.
At the worst stage, the valve is very stiff and narrow. This blocks blood flow, causing serious symptoms like chest pain, feeling dizzy, and heart failure. Often, surgery is needed to fix the valve at this point.
It’s vital to catch and watch aortic valve calcification early. Knowing the stages helps doctors make better plans to help patients.
It’s important for patients to know the signs of aortic valve calcification. This knowledge helps them get medical help early. We will look at the symptoms from the start to the later stages.
In the early stages, you might not feel any symptoms. But some people might notice small changes. It’s key to watch for any health changes early on.
When the calcification gets worse, symptoms get more obvious. You might feel chest pain, have trouble breathing, or get very tired. These happen because the valve blocks blood flow.
| Symptom | Description |
|---|---|
| Chest Pain (Angina) | Discomfort or pain in the chest due to reduced blood flow to the heart muscle. |
| Shortness of Breath (Dyspnea) | Difficulty breathing or feeling winded even when sitting or doing light activities. |
| Fatigue | Feeling very tired or weak, which means the heart is working harder. |
If you have symptoms like chest pain, trouble breathing, or fatigue, see a doctor right away. It’s important to talk to your doctor if you notice any unusual signs.
Knowing the symptoms of a calcified aortic valve helps patients take care of their health. By recognizing these signs and getting medical help quickly, people can live better lives.
A calcified aortic valve is found through a mix of clinical checks and advanced imaging. We use many methods to see how much of the valve is affected.
The first step is a detailed physical check. We listen for heart sounds and check the heart’s health. This helps decide what tests to do next.
Imaging tests are key in spotting aortic valve calcification. They give clear pictures of the heart and its valves.
An echocardiogram is a main test for the aortic valve. It checks how well the valve works and if there’s calcification.
A CT scan gives more details on calcification and valve narrowing. It helps plan treatment.
Other tests, like cardiac catheterization, help check the heart’s condition. They help find the best treatment.
By using these methods together, we can accurately find and treat calcified aortic valve problems.
Treatment for aortic valve calcification varies based on the individual. Options include medical management, surgery, and lifestyle changes. It’s important to understand these choices to make informed decisions about care.
For those with mild aortic valve calcification, medical management is often the first step. This approach involves monitoring the condition and managing symptoms with medication and lifestyle adjustments. Regular check-ups and following prescribed treatments are key to slowing the disease’s progression.
In severe cases, surgery may be needed. Surgical options include:
Valve replacement surgery is a traditional and effective method for treating severe aortic valve calcification. We consider this option for patients with significant symptoms or those at risk of complications.
TAVR is a less invasive alternative to open-heart surgery, suitable for patients who are at high risk for surgical complications. This procedure has shown promising results in improving outcomes for eligible patients.
Lifestyle changes are also important in managing aortic valve calcification. Recommendations include:
| Lifestyle Change | Benefit |
|---|---|
| Dietary adjustments | Reduces risk factors associated with cardiovascular disease |
| Regular exercise | Improves overall cardiovascular health |
| Smoking cessation | Significantly reduces cardiovascular risk |
Making these lifestyle changes can help manage the condition and improve overall health outcomes.
Not treating valve calcification can have serious effects on heart health. It can cause severe problems that make the heart work less efficiently.
Heart failure is a major risk. As calcification worsens, the heart must work harder. This can lead to fatigue and lower efficiency. Eventually, it might not be able to meet the body’s needs.
Arrhythmias, or irregular heartbeats, are another issue. The heart’s strain from calcification can disrupt its rhythm. This can cause symptoms like palpitations, shortness of breath, and dizziness.
Untreated calcification can also cause other heart problems. These include a higher risk of endocarditis, an infection of the heart valves. The heart’s strain can also reduce its output, making things worse.
It’s vital to treat valve calcification quickly to avoid these problems. Early treatment can reduce risks and improve outcomes for patients.
Managing aortic valve calcification is key to keeping your heart healthy. It needs a full treatment plan and lifestyle changes.
The future outlook for those with aortic valve calcification depends on how severe it is and the treatment. The stage of calcification, symptoms, and overall health matter a lot.
People with mild aortic valve sclerosis usually do better than those with more severe cases. Regular check-ups and care are important to keep treatment on track.
Seeing your doctor regularly is critical for managing aortic valve calcification. These visits include tests like echocardiograms to check how the condition is progressing.
| Monitoring Aspect | Description | Frequency |
|---|---|---|
| Echocardiogram | Assesses valve function and calcification | Annually or as recommended |
| Physical Examination | Evaluates overall heart health and symptoms | Every 6-12 months |
| Lifestyle Assessment | Reviews diet, exercise, and other lifestyle factors | At each follow-up visit |
Living with aortic valve calcification means finding a balance between your health and daily life. Eating well, staying active, and not smoking are important.
Key Lifestyle Adjustments:
By making these lifestyle changes and sticking to your treatment, you can greatly improve your life quality.
A calcified heart valve, like the aortic valve, is a serious issue that needs quick medical help. It’s important to know the causes, symptoms, how it’s diagnosed, and treatment options. This knowledge helps manage the condition well.
We talked about how aortic valve calcification gets worse and why finding it early is key. Knowing the risk factors and symptoms helps patients get medical help early.
At our place, we’re all about giving top-notch care and support to those with calcified heart valves. Our team works with patients to create treatment plans that fit them best. This way, we aim for the best results.
Handling aortic valve calcification right means using medicine, making lifestyle changes, and sometimes surgery. Together, we can make life better for those dealing with this condition.
A calcified heart valve happens when calcium builds up on the valve. This makes the valve hard. It can stop the heart from working right, leading to serious problems if not treated.
Aortic valve calcification is when the aortic valve gets hard due to calcium. This valve is key for blood flow in the heart. It’s caused by age, genetics, and health conditions.
At first, you might not feel anything. But as it gets worse, you might feel chest pain, have trouble breathing, or get tired easily.
Doctors use many tests to find out if you have a calcified aortic valve. They do physical checks, use echocardiography and CT scans, and check how well your heart is working.
Doctors choose the best treatment for you. It might be medicine to help with symptoms, surgery like valve replacement, or TAVR, or changes in your lifestyle to lower risks.
If you don’t get treatment, valve calcification can cause serious problems. These include heart failure, irregular heartbeats, and other heart issues.
Managing aortic valve calcification means regular check-ups and care. It’s important to keep an eye on your treatment and think about how it affects your life.
Things you can change, like smoking and high blood pressure, can help. But things you can’t change, like age and family history, also play a part.
While some things can’t be changed, knowing the causes and managing what you can helps. This can prevent and manage aortic valve calcification.
How well you do long-term depends on how bad the calcification is and your overall health. Regular check-ups are key to keeping your treatment on track
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!