Last Updated on October 21, 2025 by mcelik

Each year, nearly 1.3 million people are diagnosed with blood cancers and related disorders. This shows how important hematology oncologists are in healthcare.
These medical experts help diagnose and manage many hematologic disorders. They deal with issues like anemia, bleeding disorders, leukemia, and lymphoma.
Hematology oncologists are skilled in treating complex blood diseases and blood conditions. They offer detailed care to patients all over the world.
Hematology oncology deals with many conditions, like leukemias and lymphomas. It’s a complex field that needs a deep understanding of blood disorders and cancer medicine.
Hematology oncology combines studying blood disorders and treating cancer. It focuses on cancers that affect the blood, bone marrow, and lymphatic system. Hematologic malignancies, like leukemia and lymphoma, are its main focus.
This field is not just about treating cancer. It’s also about understanding the link between blood disorders and cancer. This knowledge is key to creating effective treatment plans for each patient.
Hematology oncologists diagnose and treat many blood cancers. They handle leukemias, lymphomas, and multiple myeloma. They also manage complications like anemia and infections.
Studies in Cureus show the field is always growing. New diagnostic and treatment methods have greatly improved patient care. Hematology oncologists work with others to give complete care, using targeted therapies and immunotherapies.
Diagnosing and treating blood cancers need a team effort. Hematology oncologists are key in coordinating care. They make sure patients get the best treatment for their condition.
A hematologist is a doctor who deals with blood disorders. They help patients with problems related to blood and its parts. This is a key role in healthcare.
Hematologists diagnose and treat blood disorders. They work on conditions like anemia and bleeding issues. Their main tasks include:
According to Cureus, hematologists are key in managing complex blood disorders. They often team up with other doctors for full care.
Hematologists and hematology oncologists both deal with blood issues. But, they focus on different areas. Hematologists handle non-cancer blood problems. Hematology oncologists work on blood cancers like leukemia.
Hematologists deal with anemia and clotting issues. On the other hand, hematology oncologists manage blood cancers. They work with oncologists and other experts.
| Specialist | Primary Focus | Examples of Conditions Treated |
| Hematologist | Non-cancerous blood disorders | Anemia, bleeding disorders, clotting disorders |
| Hematology Oncologist | Blood cancers | Leukemia, lymphoma, multiple myeloma |
Hematology has many subspecialties. This lets hematologists focus on specific areas. Some include:
These subspecialties help hematologists give better care for complex conditions. This improves patient results.
Hematologists treat blood disorders like anemia, bleeding, and clotting. These issues can really affect someone’s life. So, getting the right treatment quickly is key.
Anemia means not enough red blood cells or poor quality ones. This makes it hard for tissues to get oxygen. It can happen for many reasons, like not enough iron or vitamins, or long-term diseases.
Common symptoms of anemia include:
We’ll look at different anemia types, like iron or vitamin deficiencies, and anemia from chronic diseases. We’ll also talk about how to treat them.
Bleeding disorders affect how blood clots. They can cause too much or too long bleeding. Hemophilia and von Willebrand disease are common examples.
Key characteristics of bleeding disorders:
We’ll cover how to diagnose and manage these conditions. Hematologists play a big role in caring for people with these disorders.
Clotting disorders make it easier to form blood clots. This can lead to serious problems like deep vein thrombosis (DVT) or pulmonary embolism.
Risk factors for clotting disorders include:
We’ll talk about diagnosing, treating, and preventing clotting disorders. Hematologists are vital in managing these complex conditions.
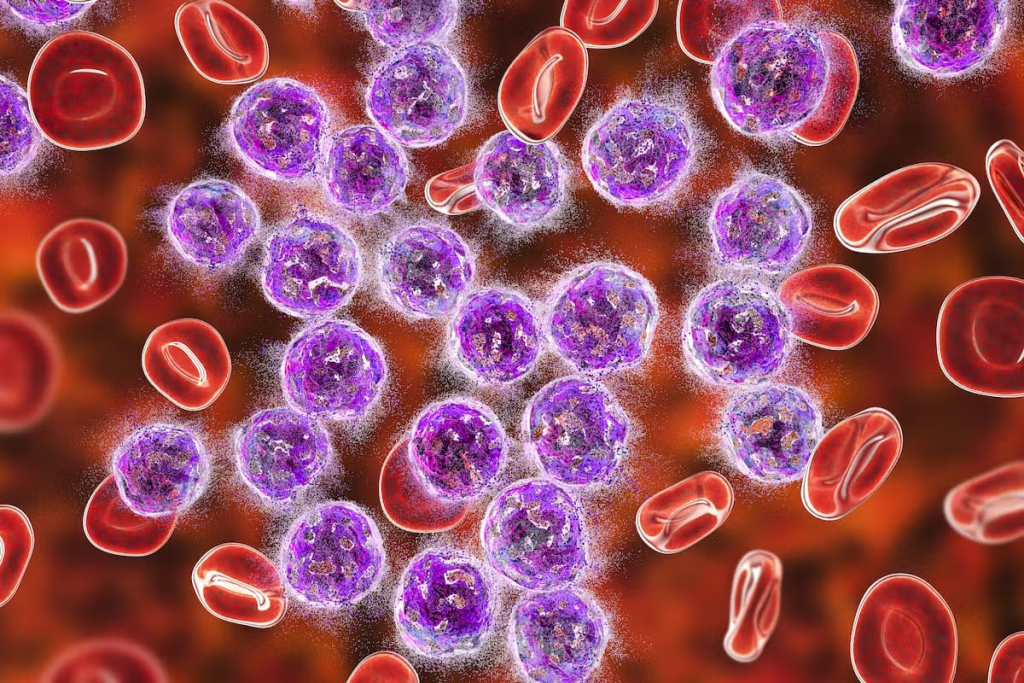
Malignant blood conditions, like leukemia, lymphoma, and multiple myeloma, are big challenges in cancer treatment today. These cancers affect the blood, bone marrow, and lymphatic system. They need detailed treatment plans.
Leukemia is a blood and bone marrow cancer. It happens when white blood cells grow too much. There are different types, like ALL, AML, CLL, and CML. The treatment depends on the type and how far it has spread.
Treatment for leukemia includes chemotherapy, targeted therapy, and stem cell transplants. New treatments have made it possible for some patients to be completely cured.
Lymphoma is a cancer of the lymphatic system, which helps fight off infections. It has two main types: Hodgkin lymphoma and non-Hodgkin lymphoma (NHL). Symptoms include swollen lymph nodes, fever, and weight loss.
Diagnosing lymphoma involves tests like PET scans and biopsies. Treatment depends on the type and stage. It might include chemotherapy, radiation, and immunotherapy.
Multiple myeloma is a cancer of plasma cells in the bone marrow. It can cause bone pain, anemia, and infections. Treatment for multiple myeloma often combines therapies like targeted therapy, chemotherapy, and stem cell transplants.
New research has brought better treatments for multiple myeloma. This has improved patients’ lives and outcomes.
Benign hematological disorders are a wide range of conditions that can really affect a person’s life. They impact different parts of the blood, like red blood cells, platelets, and white blood cells. This can cause various symptoms.
Hemoglobinopathies are genetic disorders that affect hemoglobin, a key protein in red blood cells. These issues can cause anemia, pain, and other problems.
Common Types of Hemoglobinopathies:
| Hemoglobinopathy | Characteristics | Management Strategies |
| Sickle Cell Disease | Abnormal hemoglobin causing red blood cells to be misshapen | Hydration, pain management, blood transfusions |
| Thalassemia | Reduced production of hemoglobin | Blood transfusions, iron chelation therapy |
Platelet disorders involve problems with platelets, which are key for blood clotting. These issues can cause bleeding or clotting problems.
Types of Platelet Disorders:
White blood cell disorders affect the immune system, making it harder to fight off infections or causing immune problems.
Examples of White Blood Cell Disorders:
It’s important to understand these benign hematological disorders to give the right care and improve patient outcomes. We will keep exploring these conditions and how to manage them.
Understanding sickle cell disease means looking into its causes and how it affects people. It’s a genetic disorder that changes the shape of red blood cells. This happens when the cells don’t have enough oxygen.
The disease comes from a gene mutation in the HBB gene. This mutation makes sickle hemoglobin (HbS). Under low oxygen, red blood cells become stiff and sickle-shaped. This can block small blood vessels, causing pain, infections, and organ damage.
Symptoms vary but often include pain, anemia, and more infections. Some face acute chest syndrome, a serious condition.
Managing sickle cell disease includes prevention, treatments for acute issues, and long-term care. Hydroxyurea is a key drug that lowers pain crisis frequency and may reduce other risks.
Other treatments include blood transfusions to lower sickle cell risk. In some cases, hematopoietic stem cell transplantation is considered, but it’s risky.
“Early diagnosis and complete care can greatly improve life quality for those with sickle cell disease.”
Living with sickle cell disease needs a full approach. This includes medical care, lifestyle changes, and mental support. Patients should drink plenty of water, avoid extreme temperatures, and manage stress.
Family, healthcare, and support groups are key for coping. Educational programs and counseling help understand and manage the disease’s impact.
With a detailed management plan, people with sickle cell disease can live more fully. Ongoing research and new treatments are improving their lives.
Rare blood diseases are complex and pose big challenges. They need special medical care and a deep understanding. These conditions are not common but are very important to know about.
Hemophilia is a genetic disorder that makes blood hard to clot. This leads to long bleeding. There are two main types: Hemophilia A and Hemophilia B. Treatment usually involves replacing the missing clotting factor in the blood.
Other conditions like Von Willebrand Disease and rare factor deficiencies also affect blood clotting.
Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. This can cause bone marrow failure. The risk of getting MDS goes up with age. It’s also more common after being exposed to certain chemicals or radiation.
Key things about MDS include:
Aplastic anemia is a rare condition where the bone marrow doesn’t make blood cells. It can be caused by toxins, certain medicines, or viruses. Treatment aims to fix the cause and may include immunosuppressive therapy or bone marrow transplantation.
Managing aplastic anemia involves:
In summary, rare blood diseases like hemophilia, myelodysplastic syndromes, and aplastic anemia are tough to diagnose and treat. Knowing about these conditions is key to giving good care and helping patients get better.
Autoimmune blood disorders are complex conditions where the immune system attacks the body’s own blood cells. These disorders can cause mild to severe health issues. They affect different blood components, like red blood cells, platelets, and white blood cells.
It’s important to understand these conditions for proper diagnosis and treatment. We’ll look at key autoimmune blood disorders, such as immune thrombocytopenia and autoimmune hemolytic anemia.
Immune thrombocytopenia (ITP) is an autoimmune condition with low platelet count. The immune system makes antibodies against platelets, marking them for destruction. This can cause bruising, bleeding, and a higher risk of hemorrhage.
Autoimmune hemolytic anemia (AIHA) happens when the immune system attacks red blood cells. This leads to their early destruction. It can cause anemia, jaundice, and fatigue.
The diagnosis involves a direct Coombs test, which finds antibodies or complement proteins on red blood cells. Treatment includes corticosteroids, immunosuppressive drugs, and sometimes blood transfusions.
There are other autoimmune hematologic conditions, like autoimmune neutropenia. This condition targets neutrophils, a type of white blood cell. These conditions show how autoimmune disorders can affect the blood in different ways.
We understand the complexity of autoimmune blood disorders and the need for thorough care. By knowing these conditions, we can improve diagnosis and treatment. This helps improve the lives of those affected.
Getting a correct diagnosis is key to treating blood disorders. Hematologists use many tests to find and treat different blood issues. These include anemia, bleeding problems, and blood cancers.
Blood tests are a main tool in diagnosing blood disorders. They check the levels and types of blood cells. Tests like the Complete Blood Count (CBC) and Blood Smear are common.
These tests help spot issues like anemia, infections, and leukemia. More detailed tests, like flow cytometry, can also help diagnose complex cases.
Bone marrow biopsies and aspirations are key for diagnosing blood diseases. They take samples of bone marrow for study. These tests help find:
The results from these tests are essential for figuring out blood disorders and planning treatment.
Modern hematology uses advanced tests to diagnose blood disorders. Some of these include:
| Technique | Description | Application |
| Flow Cytometry | Analyzes the characteristics of cells in a fluid | Diagnosing leukemia and lymphoma |
| Genetic Testing | Examines genetic mutations or abnormalities | Identifying genetic causes of blood disorders |
| Cytogenetic Analysis | Studies chromosomal abnormalities | Diagnosing and monitoring hematological malignancies |
These advanced tests give detailed info on blood disorders. They help doctors make accurate diagnoses and choose the right treatments.
Understanding and treating hematological conditions requires a deep dive into their causes. These disorders, from anemia to leukemia, need specific treatments. The goal is to manage symptoms and improve patient health.
Medications are key in treating hematological conditions. They include:
These drugs often work together with other treatments for the best results.
Blood transfusions are vital for many conditions. They provide:
Stem cell transplantation can cure some blood cancers. It involves:
This treatment offers hope for a cure in some cases.
New treatments like targeted and immunotherapies are changing the game. They are less toxic than traditional chemotherapy. Examples include:
These treatments are constantly improving, giving patients new hope.
It’s important to know the signs of blood disorders early. Some conditions can really affect your life. Getting diagnosed early can help manage them better.
Blood disorders show up in different ways. Some common signs are:
If you keep getting these symptoms, see your doctor. They might send you to a hematologist.
Seeing a hematologist starts with your primary care doctor. They check your symptoms and do tests. If you need a specialist, they’ll send you to one. The referral process includes:
Your primary care doctor is key in spotting blood disorders. They help you know what to do next.
Getting ready for your hematologist visit is smart. Here’s how:
Being ready can make your visit more useful. You’ll understand your condition and treatment better.
Knowing when to see a hematologist is important. Spotting signs early and following the right steps can help. This way, you get the care you need for blood disorders.
Pediatric hematology deals with many blood disorders in kids. These range from mild to serious. Kids with these issues need special care that fits their age and growth.
Children face different blood disorders, like anemia and bleeding issues. They can also get leukemia and other blood cancers. Knowing about these is key to helping them.
Some common blood disorders in kids are:
Finding out what’s wrong with a child’s blood can be hard. This is because kids are always changing and symptoms can be small. Doctors use special tests to figure out what’s going on.
| Diagnostic Tool | Description | Application in Pediatric Hematology |
| Blood Tests | Analysis of blood components to identify abnormalities. | Used to diagnose anemia, infection, and blood cancers. |
| Bone Marrow Biopsy | Examination of bone marrow to assess its function and detect malignancies. | Critical for diagnosing leukemia and other marrow disorders. |
Children with ongoing blood disorders need ongoing care. This care changes as they grow. When they get older, they need to switch to adult care to keep getting the right treatment.
Key considerations for long-term management include:
Understanding pediatric hematology helps us give kids the care they need. This improves their life and health outcomes.
Becoming a hematologist takes a lot of hard work and dedication. They are doctors who focus on blood disorders and cancers. Their education and training help them give top-notch care to patients with these conditions.
To start, one needs a bachelor’s degree in a science field. Then, four years of medical school to get an M.D. or D.O. degree. This education covers both classroom learning and clinical practice.
After medical school, they do a three-year residency in internal medicine. This hands-on experience helps them manage adult diseases, including blood-related ones.
Next, they enter a two to three year fellowship in hematology. This training focuses on blood disorders like leukemia and lymphoma.
This fellowship includes both clinical and research parts. It helps them learn new diagnostic and treatment methods. It also lets them do research and contribute to the field.
After fellowship, they can get board certified by the ABIM. This shows they are experts in their field and care deeply about their patients.
To keep their certification, they must keep learning. They stay updated with new discoveries in hematology. This ensures they can give the best care to their patients.
Key aspects of a hematologist’s education and training include:
Living with chronic blood disorders is more than just treatment. It’s about a whole care plan. These conditions, like anemia and bleeding disorders, really affect a person’s life. It’s not just about the treatment; it’s about the person’s overall health.
Managing chronic blood disorders for a long time needs a big plan. This includes checking the condition often, taking medicine as told, and making lifestyle changes. These changes help lessen symptoms and avoid problems.
Managing medicines is key to long-term care. Patients must work with their doctors to understand and follow their medicine plans.
Chronic blood disorders can really affect a person’s life. Issues like chronic pain, tiredness, and the mental stress of dealing with a long-term condition can change daily life. These problems can affect how well a person feels every day.
Support from family, friends, and groups is very important. It helps patients deal with these challenges. Doctors can also help by teaching ways to manage symptoms and improve life quality.
| Aspect of Life | Impact of Chronic Blood Disorders | Support Strategies |
| Physical Health | Chronic pain, fatigue | Pain management, energy conservation techniques |
| Emotional Well-being | Anxiety, depression | Counseling, support groups |
| Social Life | Social isolation | Support from family and friends, joining support groups |
Patients with chronic blood disorders have many support options. These include groups, online forums, and educational materials.
Groups like the Aplastic Anemia & MDS International Foundation and the National Hemophilia Foundation offer a lot. They have educational stuff, support groups, and help with advocacy.
By using these resources and a complete care plan, patients can live better with chronic blood disorders. They can manage their conditions more effectively.
Hematology oncologists are key in finding and treating blood cancers and disorders. They give full care to those with blood cancers and other blood issues.
These experts handle tough cases, like leukemia and lymphoma, and other blood problems. They use the latest tests and treatments, like medicines and stem cell transplants.
Knowing how important hematology oncologists are helps patients make better choices. It lets them find the right treatment. We see how vital these doctors are in giving top-notch care and support.
A hematologist is a doctor who focuses on blood disorders and diseases. They diagnose, treat, and manage these conditions.
Hematology oncologists deal with blood cancers and disorders. This includes leukemias, lymphomas, and multiple myeloma.
Hematologists and hematology oncologists both work with blood disorders. But, oncologists focus more on blood cancers like leukemia and lymphoma.
Hematologists treat many blood disorders. These include anemia, bleeding disorders like hemophilia, and sickle cell disease.
Tests diagnose blood disorders. These include blood tests, bone marrow biopsies, and advanced tests like flow cytometry.
Treatments vary by condition. They include medications, blood transfusions, and stem cell transplants. The choice depends on the condition and its severity.
See a hematologist if you have symptoms like fatigue, frequent infections, or easy bruising. Also, if you have a family history of blood disorders.
Prepare by gathering your medical history and symptoms. Be ready to discuss your history and any questions you have.
Hematologists manage chronic blood disorders. They provide ongoing care, monitor disease, and adjust treatments to improve quality of life.
Hematologists get a lot of education and training. This includes medical school, residency, and fellowship programs. They also get board certification.
Yes, there are many support resources. These include patient organizations, counseling services, and online resources. They help manage the condition and improve quality of life.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!