Last Updated on November 17, 2025 by Ugurkan Demir
At LivHospital, we know how important it is to understand the risks of thrombi and blood clots. A thrombus is a blood clot that forms inside blood vessels or the heart. It’s made up of platelets, fibrin, red blood cells, and white blood cells. Find out what is thrombus and how blood clots, or thrombi, can obstruct vessels and cause issues.
Thrombosis is when a blood clot forms inside a blood vessel. This can block blood flow through the body. It’s a big risk for heart health, so knowing what causes it is key.
Key Takeaways
- Thrombi are blood clots that form inside blood vessels or the heart.
- The composition of a thrombus includes platelets, fibrin, and blood cells.
- Thrombosis can obstruct blood flow, posing risks to cardiovascular health.
- Understanding thrombi is important for knowing about heart risks.
- LivHospital offers patient-centered care for conditions related to thrombi and vessel obstruction.
The Definition of a Thrombus
A thrombus is a blood clot that forms inside a blood vessel. It’s made of platelets, fibrin, and blood cells, and sticks to the vessel wall. Knowing about thrombi helps doctors diagnose and treat blood clot issues.
Medical Terminology and Etymology
The word “thrombus” comes from the Greek “thrombos,” meaning “clot” or “lump.” In medicine, a thrombus is a clot in a blood vessel that sticks to the wall. This term is used when a clot might block blood flow, causing heart problems.
Thrombi Meaning in Clinical Context
In hospitals, knowing about thrombi is key for patient care. Thrombi can lead to strokes and heart attacks by blocking blood to important organs. We need to diagnose and treat thrombi right to avoid these dangers and help patients recover well.
Understanding thrombi helps us tackle blood clot risks and care for those at risk better.
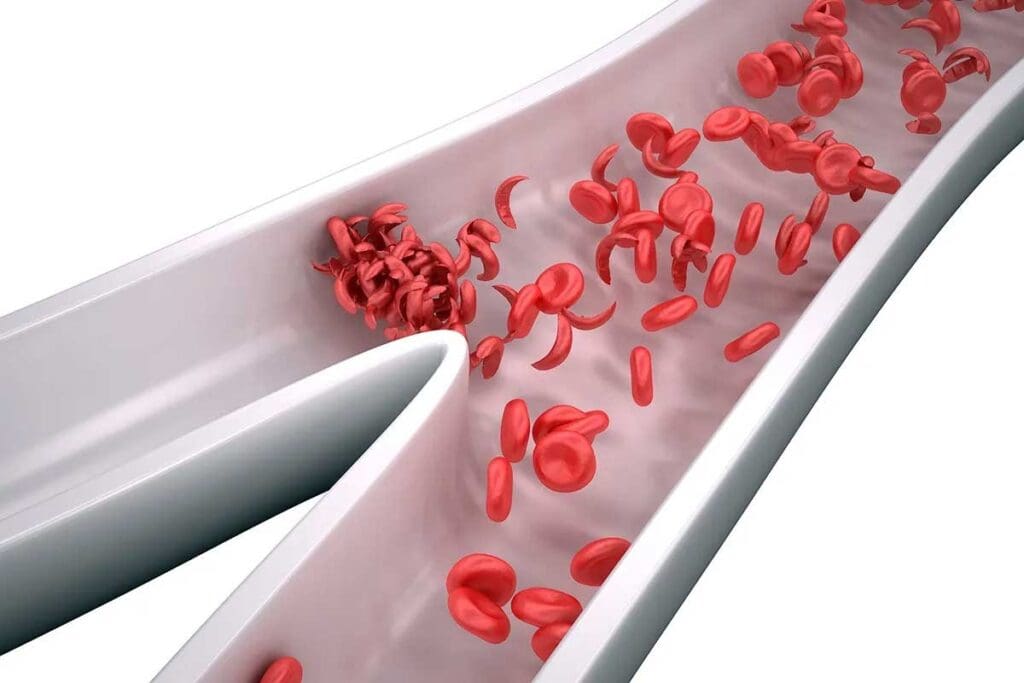
Composition and Structure of Blood Clots
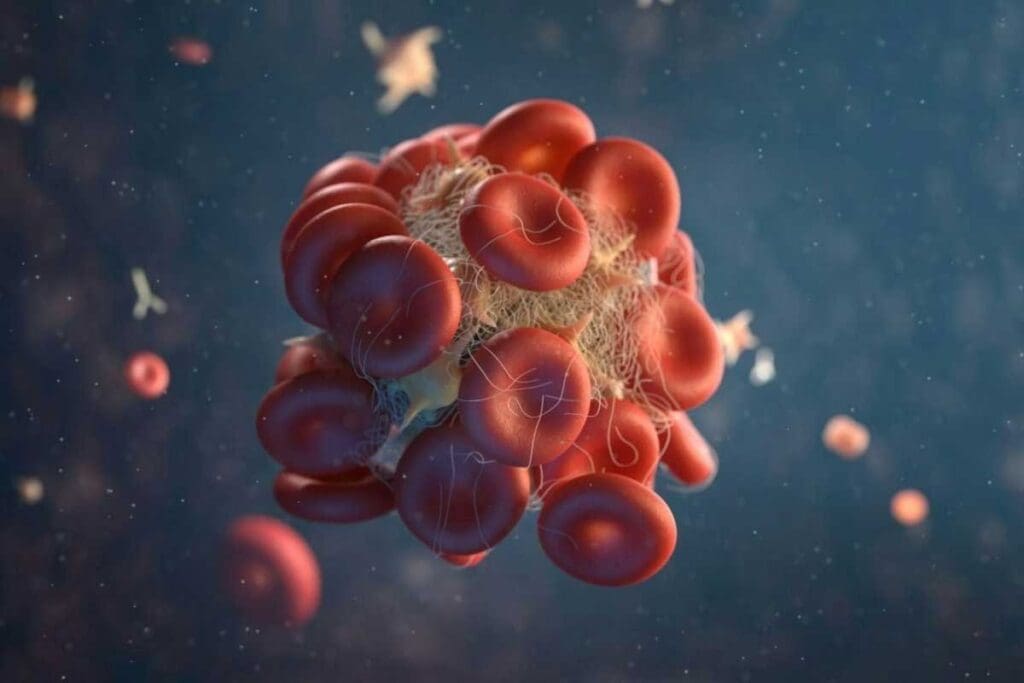
Knowing what makes up a blood clot is key to understanding its effects on heart health. A blood clot, or thrombus, is made mainly of platelets, fibrin, red blood cells, and white blood cells. The clotting process starts with platelet activation and the creation of a fibrin network. Together, they form a complex structure with big health implications.
Platelets and Their Role
Platelets are vital in forming blood clots. When a blood vessel gets hurt, platelets stick to the damage and start to clump together. This is important for stopping bleeding but can also lead to harmful clots. Platelet activation triggers a series of chemical reactions that help the clot grow.
Fibrin Network Formation
Fibrin is another key part of blood clots. It’s a protein that forms a mesh when the body is injured. This mesh traps blood cells and other debris, giving the clot strength and stability. The making of fibrin, or fibrinogenesis, happens through a series of chemical reactions in the body.
Red and White Blood Cells in Thrombi
Red and white blood cells are also part of blood clots. Red blood cells get caught in the fibrin mesh, adding to the clot’s size and stability. White blood cells, like neutrophils and monocytes, can be in clots too. They might help with inflammation and dissolving the clot. Their presence can change how the clot works and its impact on health.
. This diagram shows how platelets, fibrin, and blood cells work together in a clot.
In summary, blood clots are made up of many parts working together. Platelets, fibrin, and blood cells all play a role. Knowing how they work together helps us understand the dangers of clots and how to stop them.
Visualizing Thrombi: Blood Clot Diagrams
Visual aids like blood clot diagrams are key for doctors and patients to grasp thrombus formation. They help show the complex steps of thrombosis.
Anatomical Representation of Thrombi
Diagrams of thrombi give us a close look at their structure and how they block blood vessels. They show the thrombus forming inside the vessel. This helps us see how it sticks to the vessel wall.
How Thrombi Attach to Vessel Walls
The way thrombi stick to vessel walls is complex. Platelets start the adhesion, then a fibrin network holds the clot in place. Diagrams make this process clearer.
Visual Differences Between Types of Clots
Arterial and venous clots look different, as shown in diagrams. Arterial clots are platelet-rich and tight. Venous clots are fibrin-rich and may have more red blood cells. Knowing these differences is key for correct diagnosis and treatment.
Using blood clot diagrams helps doctors and patients learn more about thrombi. These tools are essential for managing and treating blood clot disorders.
The Process of Thrombosis: How Thrombi Form
Thrombosis is when a blood clot forms inside a blood vessel, blocking blood flow. It’s a complex process that happens for good reasons, like stopping too much bleeding when a vessel is hurt. But, if it happens too much or in the wrong way, it can cause big health problems.
Initiation Phase: Endothelial Damage
The first step in thrombosis is damage to the blood vessel’s inner lining, called the endothelium. This damage can come from many things, like injuries, infections, or atherosclerosis. When the endothelium gets damaged, it shows the blood the collagen and tissue factor underneath, starting the platelet activation and adhesion.
Propagation Phase: Clot Growth
In the next phase, the activated platelets send out signals that bring more platelets and blood cells to the injury site. This creates a platelet plug, which gets stronger with a fibrin mesh. The clot grows as more platelets, red blood cells, and white blood cells join the fibrin network.
Stabilization Phase: Clot Maturation
During the final phase, the clot gets stronger and sticks better to the vessel wall. This happens through platelet contraction and fibrin cross-linking. The clot can either dissolve or stay until the body naturally breaks it down.
Knowing how thrombosis works is key to understanding its risks. Things like not moving much, having a family history, surgery, and some health conditions can increase your risk. Knowing these risks and how thrombosis happens can help prevent and manage blood clots.
| Phase | Description | Key Events |
| Initiation | Endothelial damage exposes underlying collagen and tissue factor. | Platelet activation and adhesion |
| Propagation | Activated platelets release chemical signals, attracting more platelets and blood cells. | Formation of platelet plug and fibrin mesh |
| Stabilization | Clot maturation through platelet contraction and fibrin cross-linking. | Clot stabilization and attachment to vessel wall |
Types of Thrombi Based on Location
It’s key to know the different types of thrombi and where they form. Thrombi can appear in arteries, veins, and the heart. Where a thrombus forms affects how it’s treated and its impact on health.
Arterial Thrombi
Arterial thrombi happen in arteries. These carry oxygen-rich blood from the heart to the body. They’re linked to sudden heart attacks and strokes.
These thrombi are made of platelets and fibrin. They form when the artery wall gets damaged, often because of atherosclerosis.
Venous Thrombi
Venous thrombi form in veins. These veins bring deoxygenated blood back to the heart. They’re common in the legs and can cause deep vein thrombosis (DVT).
They’re linked to being immobile, genetic factors, and some medical conditions. Knowing the risks for venous thromboembolism is vital for prevention and treatment, as the National Center for Biotechnology Information points out.
Cardiac Thrombi
Cardiac thrombi form in the heart. They’re dangerous because they can cause cardioembolic events like strokes and systemic embolism. They’re often seen in people with atrial fibrillation, heart failure, or after a heart attack.
Managing cardiac thrombi involves anticoagulation therapy and sometimes more invasive methods.
In summary, where a thrombus forms is key to understanding its impact and treatment. Knowing the differences between arterial, venous, and cardiac thrombi helps doctors tailor treatments.
What Is a Thrombus in Different Vascular Systems
Thrombi can form in various parts of the body, leading to serious health issues. The impact of a thrombus depends on where it forms in the body.
Coronary Thrombi and Heart Attacks
Coronary thrombi are blood clots in the coronary arteries. These arteries supply blood to the heart. If a coronary thrombus blocks blood flow, it can cause a heart attack.
The severity of a heart attack depends on the thrombus’s size and location.
Key factors that influence the outcome of coronary thrombi include:
- The size of the thrombus
- The location of the occlusion
- The presence of collateral circulation
Cerebral Thrombi and Strokes
Cerebral thrombi form in the brain’s blood vessels. They can cause ischemic strokes by blocking blood flow. The effects of a cerebral thrombus depend on the brain area affected.
The timely treatment of cerebral thrombi is critical to minimize brain damage.
Deep Vein Thrombi in Extremities
Deep vein thrombi (DVT) occur in the deep veins of the extremities, often in the legs. DVT can cause pain, swelling, and warmth in the affected limb. If a part of the thrombus breaks loose, it can travel to the lungs and cause a pulmonary embolism, a potentially life-threatening condition.
Pulmonary Thrombi
Pulmonary thrombi, often originating from DVT, can migrate to the pulmonary arteries, causing a pulmonary embolism. This condition can lead to sudden onset of shortness of breath, chest pain, and in severe cases, cardiovascular collapse.
Prompt diagnosis and treatment are essential to manage pulmonary thrombi effectively.
Occlusive Thrombus: When Blood Flow Is Blocked
An occlusive thrombus happens when a blood clot blocks a blood vessel. This can lead to serious health problems. We’ll look at the differences between complete and partial blockages, the immediate effects of blockage, and the damage to tissues.
Complete vs. Partial Occlusion
An occlusive thrombus can block a blood vessel completely or partially. Complete blockage means no blood flow, while partial blockage lets some blood through.
Complete occlusion is more dangerous because it stops all blood flow. This can cause severe tissue damage. Partial occlusion may reduce blood flow, leading to tissue dysfunction.
Acute Effects of Vessel Obstruction
The immediate effects of a blocked vessel can be severe. When a major vessel is blocked, the tissue it supplies can become ischemic. This can damage or kill cells.
For example, a blocked coronary artery can cause a heart attack. A blocked cerebral vessel can lead to a stroke.
Tissue Ischemia and Necrosis
Tissue ischemia happens when blood flow is reduced or stopped. This leads to a lack of oxygen and nutrients. Prolonged ischemia can cause tissue necrosis, or premature cell death.
The effects of tissue necrosis can be severe. For instance, heart tissue necrosis from a heart attack can lead to long-term heart failure.
| Occlusion Type | Blood Flow | Tissue Effect | Clinical Outcome |
| Complete Occlusion | No blood flow | Severe ischemia, necrosis | High risk of organ damage |
| Partial Occlusion | Reduced blood flow | Ischemia, possible dysfunction | Variable clinical outcomes |
To sum up, an occlusive thrombus can cause serious health problems by blocking blood vessels. It’s important to understand the differences between complete and partial blockages. This knowledge helps in diagnosing and treating related conditions.
Complications of Thrombi
Thrombi can cause serious health problems in different parts of the body. They can lead to mild or severe conditions, even life-threatening ones.
Embolization: When Thrombi Break Free
Embolization is a major issue with thrombi. It happens when a piece of the thrombus breaks off and travels in the blood. This can block a vital blood vessel.
Depending on where it goes, embolization can be very serious. For example, if it reaches the lungs, it can cause a pulmonary embolism. This is a very dangerous condition.
It’s very important to treat thrombi quickly and effectively. If not, the risk of embolization goes up. This could lead to very bad outcomes.
Organ Damage from Prolonged Obstruction
When a thrombus blocks a blood vessel for a long time, it can harm the tissues it supplies. Tissues need oxygen and nutrients, which come through the blood. Without these, tissues can suffer from reduced blood flow and even die.
For instance, a coronary thrombus can block a heart artery, causing a heart attack. This damages the heart muscle. A cerebral thrombus can block a brain artery, leading to a stroke and brain damage.
Post-Thrombotic Syndrome
Post-thrombotic syndrome (PTS) is a problem that can happen after a deep vein thrombosis (DVT). It causes chronic pain, swelling, and skin changes in the affected limb. The severity of PTS can vary, but it can really affect a person’s life.
PTS is influenced by how big the initial DVT was and how well it was treated. To prevent PTS, DVT must be treated quickly and effectively. Also, steps should be taken to lower the chance of it happening again.
Life-Threatening Complications
Thrombi can lead to serious complications like pulmonary embolism, stroke, and myocardial infarction. These need immediate medical help to avoid fatal results.
In summary, thrombi can cause many serious problems. It’s important to understand these complications to manage and treat thrombi well. This can greatly improve patient outcomes.
Risk Factors for Thrombus Formation
Many things can lead to the formation of thrombi. This includes genetic factors and certain medical conditions. Knowing these risk factors is key to preventing and managing thrombotic events.
Genetic Predispositions
Genetics play a big role in the risk of getting thrombi. Some genetic conditions can mess with blood clotting. For example, the Factor V Leiden mutation and low levels of proteins C and S raise the risk of blood clots in veins.
Lifestyle Factors: Immobility and Habits
Lifestyle choices can also increase the risk of thrombi. Being immobile for a long time, like on a long flight or in bed, can cause blood to pool. This can lead to clotting. Smoking and being overweight are also bad for your blood clotting risk.
Medical Conditions That Increase Risk
Some medical conditions can also raise the risk of thrombi. These include cancer, heart disease, and blood clotting disorders. People with these conditions need careful management to lower their risk of blood clots.
Surgical and Trauma-Related Risks
Surgery and trauma are big risks for thrombi. Major surgeries and severe injuries can harm blood vessels and start the clotting process. It’s important to know these risks to take the right steps to prevent them.
To show the risks and their effects, here’s a table:
| Risk Factor | Description | Implications |
| Genetic Predispositions | Conditions like Factor V Leiden mutation | Increased risk of venous thromboembolism |
| Immobility | Prolonged bed rest or long flights | Blood stasis leading to clot formation |
| Medical Conditions | Cancer, heart disease | Increased risk of thrombosis |
| Surgery and Trauma | Major surgeries, severe injuries | Damage to blood vessels, triggering clotting |
Diagnostic Approaches for Thrombi
Diagnosing thrombi uses many methods, like imaging and lab tests. It’s key to get it right for good treatment and results.
Imaging Techniques
Imaging is a big help in finding thrombi. The right tool depends on where and what kind of clot it is.
- Ultrasound: It’s often used for DVT, being non-invasive and showing images in real-time.
- Computed Tomography (CT) Scan: CT scans spot thrombi in big vessels and organs, like in the lungs.
- Magnetic Resonance Imaging (MRI): MRI is great for seeing clots in small vessels, like in the brain.
Laboratory Tests and Biomarkers
Labs are key when imaging doesn’t show enough. They help confirm a clot when other tests fail.
| Test | Purpose |
| D-dimer | Shows fibrin breakdown, helping rule out DVT and lung clots |
| Complete Blood Count (CBC) | Finds issues that might lead to clotting |
| Coagulation Studies | Checks how blood clots, helps with blood thinners |
“The use of D-dimer testing has revolutionized the diagnosis of venous thromboembolism, allowing for safe exclusion of the condition in patients with low pre-test probability.”
Wells PS, et al. (2003)
Clinical Assessment Methods
Checking a patient is key in finding thrombi. It helps pick the right tests to use.
A good medical history and physical check can hint at a clot. Signs like swollen limbs, pain, or trouble breathing might mean a clot.
By mixing clinical checks with imaging and lab tests, doctors can spot and treat clots well.
Treatment Strategies for Thrombi
There are many ways to treat thrombi, from medicines to surgery. It’s important to manage thrombi well to avoid serious problems like embolisms and organ damage. We’ll look at the different treatments, their benefits, and risks.
Anticoagulant Therapies
Anticoagulant medicines are key in treating thrombi. They stop new clots from forming and growing. Heparin, warfarin, and NOACs like rivaroxaban and apixaban are common ones. It’s important to watch these medicines closely to avoid bleeding.
“Anticoagulants can prevent clots but also raise the risk of bleeding,” says a leading hematology expert. So, the right medicine and how long to use it depends on the patient’s risk.
Thrombolytic Treatments
Thrombolytic drugs dissolve clots. They’re used quickly in emergencies like heart attacks or strokes. Alteplase is a well-known drug for this. Quick action is key for these treatments to work.
- Indicated for acute ischemic stroke
- Used in the management of pulmonary embolism
- Can be lifesaving in cases of massive myocardial infarction
Surgical Interventions
Surgery might be needed to remove a clot or improve blood flow. Surgical thrombectomy removes the clot mechanically. It’s used when medicines or other treatments don’t work.
| Surgical Procedure | Indications | Benefits |
| Surgical Thrombectomy | Large clots, failed medical therapy | Immediate clot removal |
| Angioplasty and Stenting | Arterial thrombosis | Restores blood flow, prevents re-occlusion |
Emerging Treatment Approaches
New treatments for thrombi are being researched. This includes safer anticoagulants and targeted therapies. The future of treating thrombi is in personalized medicine, tailored to each person’s needs.
As we learn more about thrombosis, we’ll see better and safer treatments. This will help patients avoid serious complications from thrombi.
Conclusion: Understanding the Importance of Thrombus Awareness
It’s key to know about thrombi to stop and handle problems they cause. Knowing about thrombi helps keep our hearts healthy. Thrombi can form anywhere in the body, leading to serious issues if not treated fast.
Being aware of thrombi is critical for catching and treating them early. By knowing the risks and signs of thrombi, people can act early to lower their risk. We stress the need to understand thrombi to improve health.
Living a healthy life, knowing your family health history, and managing health issues are important steps. We urge people to talk to doctors to learn about their risks. This way, they can make a plan to prevent thrombi.
FAQ
What is a thrombus?
A thrombus is a blood clot that forms inside a blood vessel. It blocks the blood flow. It’s made of platelets, fibrin, and other blood cells.
What is the difference between a thrombus and an embolus?
A thrombus forms inside a blood vessel. An embolus is a clot that breaks loose and travels through the blood. It can block blood flow elsewhere.
What are the risks associated with thrombi formation?
Thrombi can cause serious health problems. These include heart attacks, strokes, and deep vein thrombosis. The risks depend on where the clot is and if it blocks blood flow.
How do thrombi form?
Thrombi form through thrombosis. This involves platelet activation, a fibrin network, and blood cell accumulation.
What are the different types of thrombi based on their location?
Thrombi are classified by location. They can be arterial, venous, or cardiac, depending on where they form in the vascular system.
What is an occlusive thrombus?
An occlusive thrombus blocks blood flow through a vessel. It can lead to tissue ischemia and necrosis.
How are thrombi diagnosed?
Imaging techniques like ultrasound, CT scans, and MRI diagnose thrombi. Laboratory tests and clinical assessments also help.
What are the treatment options for thrombi?
Treatment for thrombi includes anticoagulant therapies and thrombolytic treatments. Surgery and new treatments are also options, based on the clot’s location and severity.
What are the risk factors for thrombus formation?
Risk factors include genetic predispositions and lifestyle factors like immobility. Medical conditions and surgical or trauma-related risks also play a part.
Can thrombi be prevented?
While some risks can’t be avoided, prevention is possible. A healthy lifestyle, managing medical conditions, and following post-surgical guidelines can help.
What are the complications of thrombi?
Complications include embolization and organ damage. Post-thrombotic syndrome and life-threatening conditions can also occur, depending on the clot’s location and severity.
References
- National Heart, Lung, and Blood Institute. (2022). Thrombosis. U.S. Department of Health and Human Services.https://www.nhlbi.nih.gov/health/thrombosis