Last Updated on November 27, 2025 by Bilal Hasdemir
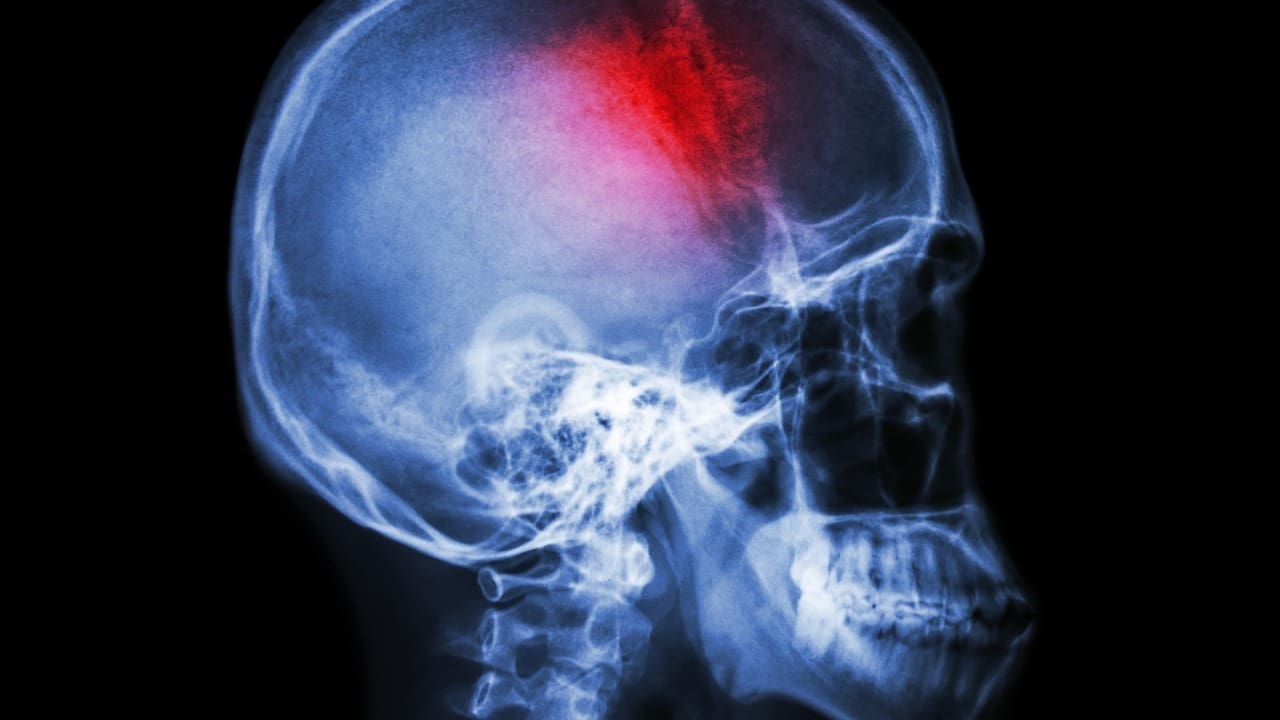
At Liv Hospital, we know how acute cerebral infarction affects people and their families. This condition, also known as an ischemic stroke, happens when blood flow to the brain stops suddenly. This leads to damage because of a lack of oxygen and nutrients.
We know how important quick medical help is. Our goal is to offer top-notch healthcare and support for patients from around the world. Learning about infarct stroke and its effects is the first step to getting better.
The term ‘acute cerebral infarction’ means sudden brain function loss due to blocked blood vessels. This leads to rapid brain cell death and neurological problems. It’s a medical emergency needing quick treatment to reduce brain damage.
Cerebral infarction, or ischemic stroke, happens when a brain blood vessel gets blocked. Knowing the medical terminology is key. The term “infarct” means tissue death from no blood supply. The National Center for Biotechnology Information says it’s a big cause of illness and death globally.
This condition means sudden brain cell death, causing neurological issues. Symptoms include facial drooping, arm weakness, and speech problems. Knowing the cerebrovascular infarction definition helps doctors give the right care.
It’s important to know the difference between cerebral infarction and other brain injuries. Unlike hemorrhagic stroke, which is bleeding in the brain, infarction is a blockage. Doctors say knowing the difference is key for the right treatment.
Unlike traumatic brain injuries from outside forces, infarction is caused by internal blockages. Knowing these differences helps in giving the right care. The term infarct cerebral means the dead brain tissue from no blood supply.
Understanding cerebral infarcts is key to finding treatments. These strokes happen when blood flow to the brain stops. This can be due to a blockage or a blood vessel rupture, causing tissue damage.
When blood flow stops, the brain lacks oxygen and glucose. This damages brain tissue in several ways. The lack of oxygen forces the brain to switch to anaerobic metabolism, leading to lactic acid buildup and less ATP.
This energy failure causes ion pumps to fail. This leads to an influx of calcium ions into neurons, worsening cellular injury.
The blood–brain barrier (BBB) is also vital in cerebral infarcts. Damage to the BBB can cause edema. This makes it harder for oxygen and nutrients to reach the brain tissue.
“The integrity of the BBB is critical in stroke outcomes, as damage can worsen injury severity.”
The ischemic cascade is a series of events after blood flow stops. It includes energy failure, oxidative stress, excitotoxicity, and ion imbalance. These lead to cell death through necrosis and apoptosis.
| Process | Description | Effect on Brain Tissue |
|---|---|---|
| Energy Failure | Lack of ATP due to insufficient oxygen and glucose | Impaired neuronal function, ion pump failure |
| Oxidative Stress | Production of reactive oxygen species (ROS) | Damage to cellular components, including DNA and proteins |
| Excitotoxicity | Release of excitatory neurotransmitters like glutamate | Overactivation of glutamate receptors, leading to calcium influx and cell death |
The ischemic cascade is key to understanding cerebral infarcts. It shows how processes like energy failure and oxidative stress harm brain tissue. This knowledge is vital for finding effective treatments.
Brain infarcts are divided into different types, each with its own traits and treatment needs. Knowing these types helps doctors understand and treat brain infarcts better.
Territorial infarcts happen when a major artery to the brain gets blocked. This causes damage in the area that artery supplies. These infarcts are big and can lead to serious brain problems.
The symptoms of territorial infarcts vary based on the blocked artery. For example, a blockage in the middle cerebral artery can cause weakness on one side of the body and trouble speaking if the left side of the brain is affected.
Lacunar infarcts are small and happen in deep brain arteries. They are usually less than 1.5 cm in size. They are often linked to high blood pressure and small blood vessel disease.
Lacunar infarcts can show up in different ways, like weakness on one side of the body or trouble with balance. Even though they are small, they can cause a lot of disability.
Watershed infarcts happen at the edges of two major arteries’ territories. These areas are more likely to get damaged when blood flow drops. This can happen due to low blood pressure or severe narrowing of the carotid artery.
Watershed infarcts can be either in the brain’s outer layer (cortical) or deeper (subcortical). Cortical ones often cause problems with thinking and behavior. Subcortical ones might lead to more movement issues.
| Type of Infarct | Characteristics | Common Causes |
|---|---|---|
| Territorial Infarcts | Large infarcts in the territory of a major artery | Occlusion of major cerebral arteries |
| Lacunar Infarcts | Small infarcts in deep penetrating arteries | Hypertension, small vessel disease |
| Watershed Infarcts | Infarcts at border zones between major arteries | Systemic hypotension, severe carotid stenosis |
It’s important for doctors to know about the different types of brain infarcts. Each type has its own way of happening, showing symptoms, and affecting the brain. This knowledge helps doctors give the best care and treatment.
The brain needs blood to work right. Any problem with blood flow can cause acute cerebral infarction. Knowing why it happens helps us prevent and treat it.
Thrombotic strokes happen when a blood clot blocks a brain blood vessel. Hypertension can damage blood vessel walls, making clots more likely. Atherosclerosis, or plaque buildup in arteries, also increases the risk.
“Thrombus formation is a complex mix of blood flow, vessel wall issues, and blood composition,” experts say. This shows how many factors play a role in thrombotic strokes.
Embolic strokes occur when a clot or particle from elsewhere blocks a brain blood vessel. Atrial fibrillation, an irregular heartbeat, is a big risk factor. It can cause clots in the heart.
Preventing embolic strokes means treating heart issues and managing risks like high blood pressure and diabetes.
In summary, both thrombotic and embolic strokes are major causes of acute cerebral infarction. Knowing about these causes and their risk factors is key to preventing and treating them.
Cerebral infarctions can be caused by many factors. Some can be changed, while others can’t. Knowing these factors helps in preventing and managing cerebral infarctions.
Modifiable risk factors are things we can change. By treating or changing these, we can lower our risk of cerebral infarction.
Hypertension is a big risk for cerebral infarction. It harms blood vessels, making them more likely to block. Cardiovascular disease, like atrial fibrillation, also raises the risk by causing blood clots.
Other lifestyle choices also play a part. Smoking, physical inactivity, and an unhealthy diet can all increase the risk. Smoking harms blood vessels, being inactive can lead to obesity and diabetes, and a bad diet can cause high cholesterol and hypertension.
Non-modifiable risk factors are things we can’t change. Knowing about these can help us take steps to prevent them.
Age is a big risk factor, with risk going up after 55. Genetic predisposition also matters, with a family history of stroke increasing risk.
A history of previous stroke or transient ischemic attack (TIA) raises the risk of another stroke. Knowing this can help us take steps to prevent it.
By managing both changeable and unchangeable risk factors, we can lower our risk of cerebral infarction. This improves our overall health.
It’s important for both patients and healthcare providers to know the symptoms of a cerebral infarction. This condition, also known as a stroke, happens when blood flow to the brain is cut off. This prevents brain tissue from getting the oxygen and nutrients it needs. Spotting the warning signs early is key to getting medical help fast.
The symptoms of acute cerebral infarction can differ based on the brain area affected. Common signs include sudden weakness or numbness in the face, arm, or leg, often on one side.
Motor symptoms often show up as:
Sensory symptoms may include:
Cognitive and speech issues can be very challenging, including:
The American Stroke Association says, “Act F.A.S.T.” is a simple way to remember stroke signs and the need to act fast.
The FAST method is a well-known tool for spotting stroke symptoms. It stands for:
By knowing the symptoms of acute cerebral infarction and using the FAST method, we can quickly spot when someone is having a stroke. This ensures they get the medical care they need quickly.
Diagnosing cerebrovascular infarction needs a mix of imaging and tests. These tools help us see how big and what kind of infarction it is. This info guides our treatment and helps patients get better.
Imaging is key in diagnosing cerebrovascular infarction. We use high-tech imaging to see the brain and blood vessels. This helps us find out why and how big the infarction is.
CT scans are first choice in acute strokes because they’re quick and easy to get. They help spot bleeding strokes and rule out other problems. Though MRI is better for early signs, CT scans are essential in emergencies.
MRI is better at finding early signs of stroke and showing how big the infarction is. We use special MRI scans to see how bad the stroke is and if we can save some brain tissue. These scans are key in deciding how to treat the patient.
We also use other tests to check patients with suspected cerebrovascular infarction. These tests help find the cause and risk factors. This helps us plan the best treatment.
| Diagnostic Test | Purpose |
|---|---|
| Electrocardiogram (ECG) | To identify cardiac sources of embolism, such as atrial fibrillation |
| Blood Tests | To assess for risk factors such as hyperlipidemia, diabetes, and inflammation |
| Carotid Ultrasound | To evaluate for carotid artery stenosis or occlusion |
By using imaging and other tests together, we can fully check patients with cerebrovascular infarction. This helps us make the best treatment plans.
Managing brain infarction requires a detailed plan. It aims to restore blood flow, manage symptoms, and prevent more damage. We’ll look at emergency treatments, medicines, and surgery.
Quick action is key in treating acute cerebral infarction. The goal is to get blood flowing back to the brain fast to lessen damage.
Thrombolytic therapy uses drugs to break up blood clots. Alteplase (tPA) is a common drug that can help if used quickly after symptoms start.
Mechanical thrombectomy removes the clot from the blood vessel. It’s very effective for big clots and can greatly improve outcomes if done quickly.
Both thrombolytic therapy and mechanical thrombectomy are urgent. The choice depends on how long ago the stroke happened, the clot’s size and location, and the patient’s health.
Medicines are vital in treating cerebral infarction. They include drugs to prevent clots, control blood pressure, and manage diabetes and high cholesterol.
| Medication Type | Examples | Purpose |
|---|---|---|
| Antiplatelet Agents | Aspirin, Clopidogrel | Prevent platelet aggregation and clot formation |
| Anticoagulants | Warfarin, Novel Oral Anticoagulants (NOACs) | Prevent new clot formation and reduce risk of further strokes |
| Blood Pressure Management | ACE inhibitors, Beta-blockers | Control hypertension to reduce stroke risk |
Surgery may be needed for complications or to fix underlying issues. This includes surgery to relieve swelling or to clean out carotid arteries.
Handling brain infarction needs a detailed plan for each patient. Knowing the treatment options helps doctors give the best care for those with cerebral infarction.
Understanding cerebral infarction is key to preventing and managing it. We’ve looked at its definition, how it works, and how to diagnose and treat it.
Managing cerebral infarction means controlling risk factors and living a healthy lifestyle. It also means getting medical help fast when symptoms show up. This way, people can lower their stroke risk.
It’s vital to get medical help quickly and make lifestyle changes to prevent cerebral infarction. Working with doctors, people can create a plan to lower their risk factors. This improves their health overall.
By using these strategies, people can handle their condition better. They can also lower the chance of future strokes. This makes life better for those living with cerebral infarction.
Acute cerebral infarction, also known as ischemic stroke, happens when blood flow to the brain stops or slows down. This prevents brain tissue from getting oxygen and nutrients. It can cause tissue damage and loss of brain function.
Cerebral infarction is a brain injury caused by a lack of blood flow. Other brain injuries can come from trauma, infection, or other causes. Cerebral infarction is when brain tissue dies because of a lack of blood flow.
Symptoms include sudden weakness or numbness in the face, arm, or leg. You might also have trouble speaking or understanding speech. Other signs are sudden vision changes, dizziness, or loss of balance. The FAST method helps spot these symptoms: Face drooping, Arm weakness, Speech difficulty, and Time to call for emergency services.
Risk factors you can change include high blood pressure, diabetes, high cholesterol, smoking, and obesity. Risk factors you can’t change include age, family history, and genetics. Changing the things you can control can lower your risk of cerebral infarction.
Doctors use imaging like CT or MRI scans to see the brain and find damage. They might also do blood tests, electrocardiograms, and carotid ultrasound.
Emergency treatments might include dissolving clots with thrombolytic therapy or removing the clot with mechanical thrombectomy. Other treatments include medicines to manage symptoms, prevent more strokes, and help recovery.
While some risks can’t be changed, managing modifiable risks can help prevent cerebral infarction. This includes keeping blood pressure healthy, managing diabetes, and not smoking.
Cerebral infarction can cause significant disability. It affects cognitive, motor, and sensory functions. The impact depends on the location and severity of the infarct, and the effectiveness of treatment and rehabilitation.
A lacunar infarct is a type of cerebral infarction in the deep brain arteries. It causes small, cavity-like lesions. Lacunar infarcts are often linked to high blood pressure and can lead to significant cognitive and motor impairments.
The ischemic cascade is a series of events after blood flow stops in the brain. It leads to tissue damage and cell death. Understanding this cascade is key to finding effective treatments for cerebral infarction.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!