Last Updated on November 26, 2025 by Bilal Hasdemir

At Liv Hospital, we know how vital complete cancer care is. Adjuvant chemotherapy is key in this care. It targets cancer cells left after the first treatment, like surgery or radiation.
Using anti-cancer drugs after the first treatment kills any leftover cancer cells. This lowers the chance of cancer coming back. Studies have found that this method greatly boosts survival rates for cancers like breast, colon, and lung.
We add adjuvant chemotherapy to our treatment plans to help our patients get the best results. Our focus on advanced cancer treatment and care for our patients shows in our team effort. We make sure every patient gets all the support they need during their treatment.
Key Takeaways
- Adjuvant chemotherapy targets remaining cancer cells after primary treatment.
- It reduces the risk of cancer recurrence and improves survival rates.
- Recent studies show significant benefits for breast, colon, and lung cancer patients.
- Our multidisciplinary approach ensures complete care for international patients.
- Liv Hospital is dedicated to top-notch cancer treatment.
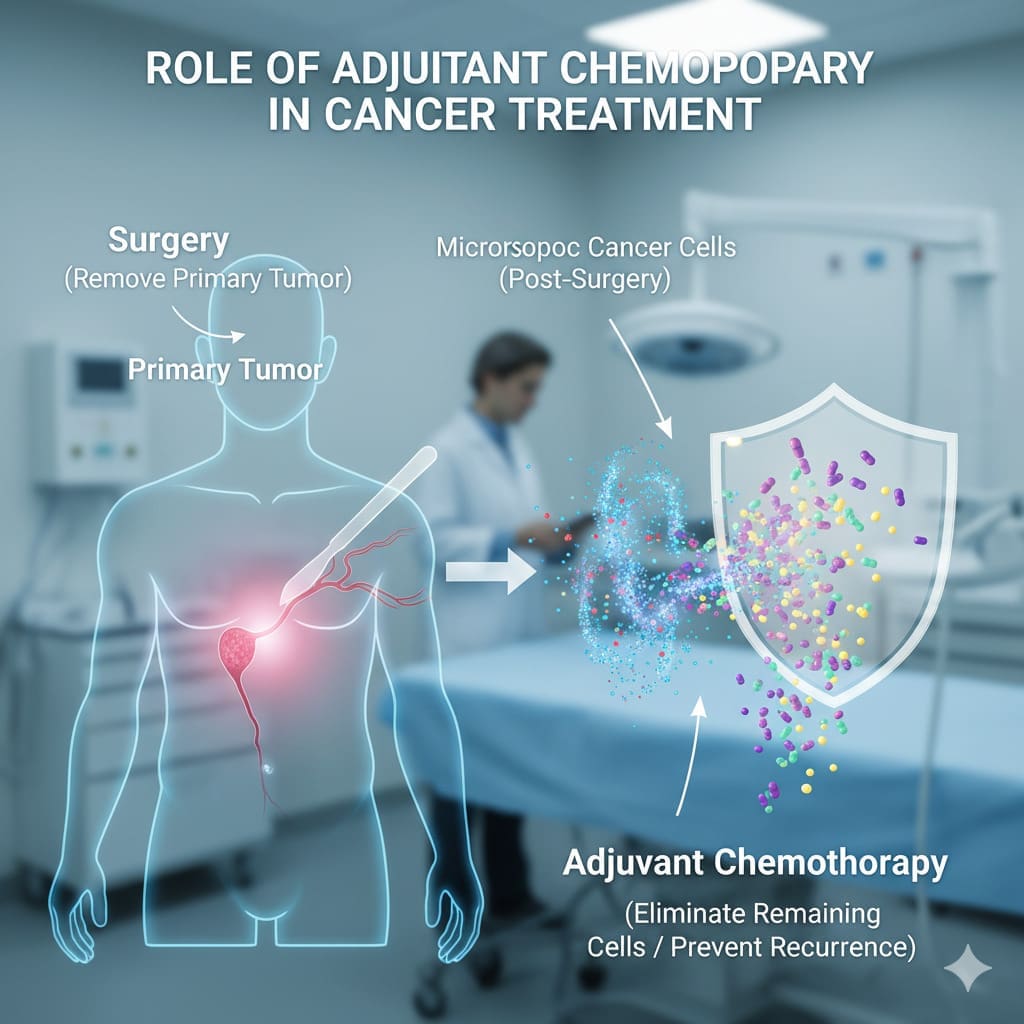
The Role of Adjuvant Chemotherapy in Cancer Treatment
Adjuvant chemotherapy is a treatment that helps primary cancer treatments work better. It kills any cancer cells left after surgery or other treatments. This lowers the chance of cancer coming back.
Definition and Purpose
Adjuvant chemotherapy, or adjuvant therapy, is given along with main treatments to prevent cancer return. It aims to find and kill cancer cells in other parts of the body. This improves cancer care results.
We add adjuvant chemotherapy to main treatments like surgery. It makes these treatments more effective and cuts down recurrence risk. This is key for cancers with high recurrence risk.
Difference from Neoadjuvant and Palliative Chemotherapy
It’s important to know how adjuvant chemotherapy is different. Neoadjuvant chemotherapy is used before main treatments to shrink tumors. Adjuvant chemotherapy is given after main treatments.
Palliative chemotherapy aims to ease symptoms and improve life quality for advanced cancer patients. It’s not meant to cure the disease.
Knowing these differences helps patients understand their treatment options. Adjuvant chemotherapy’s benefits often outweigh its side effects for many patients.
How Adjuvant Chemotherapy Works to Prevent Cancer Recurrence
Adjuvant chemotherapy is key in stopping cancer from coming back. It targets cancer cells left behind after surgery. These tiny cells can’t be seen with regular tests but can cause cancer to return if not treated.
Targeting Micrometastases
Adjuvant chemotherapy aims to find and kill these tiny cancer cells. It uses drugs that travel through the body to find and destroy cancer cells in other parts. Research shows it can lower the chance of cancer coming back by getting rid of these tiny cells.
The main goal of adjuvant chemotherapy is to lower the chance of cancer coming back and help patients live longer. By targeting these tiny cancer cells, it stops cancer from spreading. This improves how well patients do.
Cellular and Molecular Mechanisms
Adjuvant chemotherapy works by messing with how cancer cells make copies of themselves. It stops cancer cells from growing and dividing. This leads to cancer cells dying, which lowers the risk of cancer coming back.
Doctors tailor adjuvant chemotherapy to each patient’s cancer and health. The choice of drugs and how long treatment lasts depends on the cancer type and the patient’s health.
Understanding how adjuvant chemotherapy works helps patients see its value in their treatment plan. It’s a vital part of cancer care. Many studies have shown it’s effective in stopping cancer from coming back.
The Evolution of Adjuvant Chemotherapy in Oncology
Adjuvant chemotherapy has become key in fighting cancer. This change came from big steps in research and history. These steps have made it a mainstay in cancer treatment.
Historical Development
The idea of adjuvant chemotherapy started in the early 1900s. But it really took off in the 1960s and 1970s. Back then, doctors were trying to find ways to kill cancer cells left after surgery.
As we learned more about cancer, so did our treatments. We started using more targeted therapies. This led to better results for many cancer patients.
“The development of adjuvant chemotherapy has been a paradigm shift in the treatment of cancer, providing a means to address microscopic disease and improve survival rates.”
Major Research Breakthroughs
Big discoveries have moved adjuvant chemotherapy forward. Finding biomarkers that show how well a patient will respond to certain drugs was a big step.
Studies have shown that adjuvant chemotherapy helps a lot. For example, it has greatly improved survival rates in breast cancer patients. It helps lower the chance of cancer coming back.
| Cancer Type | Adjuvant Chemotherapy Regimen | Survival Rate Improvement |
|---|---|---|
| Breast Cancer | Anthracycline-based | 20-30% |
| Colorectal Cancer | FOLFOX | 15-25% |
| Non-Small Cell Lung Cancer | Platinum-based | 10-20% |
Adjuvant chemotherapy will keep being a big part of cancer treatment. We’re working hard to make treatments better and safer. This will help patients even more.
Knowing how adjuvant chemotherapy has evolved helps us see its importance today. It also shows us where it can go in the future.
When Doctors Recommend Adjuvant Chemotherapy
Doctors decide on adjuvant chemotherapy based on a detailed look at the patient’s health and cancer type. They check if the cancer might come back and if more treatment could help.
Risk Assessment Factors
Several important factors guide the decision for adjuvant chemotherapy. These include:
- The type and stage of cancer
- The presence of cancer cells in lymph nodes or other areas
- The grade of the tumor
- The patient’s overall health and medical history
- Genetic markers or other biomarkers associated with the cancer
Doctors use these factors to guess the chance of cancer coming back. They then decide if adjuvant chemotherapy is a good choice.
| Risk Factor | Description | Impact on Treatment Decision |
|---|---|---|
| Cancer Type | The specific type of cancer, such as breast, colon, or lung cancer | Influences the choice of chemotherapy drugs and regimen |
| Cancer Stage | The extent of cancer spread, including tumor size and lymph node involvement | Affects the likelihood of recurrence and the need for adjuvant treatment |
| Tumor Grade | A measure of how much the tumor cells resemble normal cells | Higher-grade tumors may require more aggressive treatment |
Cancer Types and Stages Most Responsive to Adjuvant Treatment
Some cancers and stages do better with adjuvant chemotherapy. For example:
- Early-stage breast cancer with high-risk features
- Stage III colon cancer
- Non-small cell lung cancer with lymph node involvement
Studies show that adjuvant chemotherapy can greatly improve outcomes for these patients. It helps lower the chance of cancer coming back.
Shared Decision-Making Process
The choice to have adjuvant chemotherapy is a team effort. It involves:
- Discussing the benefits and risks of treatment
- Considering the patient’s preferences and values
- Reviewing the latest research and treatment guidelines
- Creating a treatment plan that fits the patient
By working together, patients and doctors can make a choice that weighs the benefits against the risks and side effects.
Adjuvant Chemotherapy for Breast Cancer: Protocols and Outcomes
Adjuvant chemotherapy is key in treating breast cancer. It kills any cancer cells left after the first treatment. This lowers the chance of cancer coming back, helping patients live longer.
Common Drug Regimens
Many drug combinations are used in adjuvant chemotherapy. For example, a mix of cyclophosphamide and doxorubicin, then paclitaxel or docetaxel. The right mix depends on the patient’s health, cancer stage, and tumor type.
New treatments like Verzenio (abemaciclib) are showing great promise. They help certain patients even more.
Statistical Improvements in Survival Rates
Research shows adjuvant chemotherapy greatly boosts survival chances for breast cancer patients. Adding taxanes to anthracyclines can cut recurrence risk by up to 30%. Targeted therapies also improve results, helping more patients survive.
Thanks to adjuvant chemotherapy, breast cancer deaths have dropped. As research grows, we’ll see even better treatments and care for patients.
Colorectal Cancer and Adjuvant Chemotherapy Success Rates
Adjuvant chemotherapy is key in fighting colorectal cancer. It helps lower the chance of cancer coming back and boosts survival rates. We’ll look at how it’s used in treating colorectal cancer, focusing on different stages and the evidence backing its use.
Stage-Specific Treatment Approaches
Adjuvant chemotherapy’s use changes with the cancer’s stage. For stage III colon cancer, it’s a common treatment. It often includes drugs like FOLFOX or CAPOX, which have proven to help patients live longer and stay cancer-free.
In stage II colon cancer, the choice to use adjuvant chemotherapy is more complex. It depends on factors like tumor size, lymph node count, and cell type. For rectal cancer, chemotherapy is sometimes paired with radiation to control the cancer and lower recurrence risk.
Evidence-Based Outcome Data
Many studies have shown adjuvant chemotherapy’s success in treating colorectal cancer. A big study found that it greatly lowers the chance of cancer coming back and improves survival in stage III colon cancer patients.
| Cancer Stage | Treatment Approach | Outcome |
|---|---|---|
| Stage III Colon Cancer | FOLFOX or CAPOX | Improved DFS and OS |
| Stage II Colon Cancer with High-Risk Features | Fluoropyrimidine-based chemotherapy | Potential improvement in DFS |
| Rectal Cancer | Adjuvant chemotherapy with radiation therapy | Improved local control and reduced recurrence |
Risk Reduction Statistics
Adjuvant chemotherapy significantly cuts down recurrence and death rates in colorectal cancer. For stage III colon cancer, it can reduce recurrence risk by up to 30% and boost survival by 20-30%.
These numbers show how vital adjuvant chemotherapy is in managing colorectal cancer. It plays a big part in bettering patient outcomes and survival rates.
Lung Cancer and Other Malignancies: The Impact of Adjuvant Treatment
Adjuvant chemotherapy in oncology has shown great promise. It’s changing how we treat different cancers. Adjuvant chemotherapy is key in this shift.
Non-Small Cell Lung Cancer Protocols
For non-small cell lung cancer (NSCLC), adjuvant chemotherapy is now standard. It’s used for stage II and III patients. Clinical trials show it can greatly improve survival rates.
The treatment plan is based on the patient’s tumor and health. Research is ongoing to find better treatments.
Applications in Melanoma, Ovarian, and Other Cancers
Adjuvant chemotherapy is also used for other cancers. In melanoma, it includes interferon and ipilimumab. For ovarian cancer, it’s a key part of treatment after surgery. It helps improve survival rates.
Other cancers like breast and colorectal also benefit. Adjuvant chemotherapy is vital in modern oncology.
Comparative Effectiveness Across Cancer Types
The benefits of adjuvant chemotherapy vary by cancer type. For example, NSCLC sees smaller benefits compared to breast or ovarian cancers. But, even small gains can make a big difference for many patients.
Our knowledge of adjuvant chemotherapy’s effectiveness is growing. As we learn more, combining it with other treatments could lead to better results for many cancers.
The Patient Experience During Adjuvant Chemotherapy
Adjuvant chemotherapy is a complex journey. It involves many aspects of care and support. Understanding the treatment timeline, how it’s given, and how it’s monitored is key for both patients and healthcare providers.
Treatment Timeline and Scheduling
Adjuvant chemotherapy lasts several months. The exact time depends on the cancer type, stage, and treatment plan. We work with patients to create a plan that works with their life.
For example, breast cancer treatment might include four to six cycles of chemotherapy. Each cycle is three weeks long. Patients get chemotherapy on the first day and then rest. Knowing this helps them prepare for treatment.
Administration Methods and Settings
Chemotherapy can be given in clinics, hospitals, or at home. We use central venous catheters or peripheral IV lines for drug delivery. We choose the best method for each patient.
In some cases, patients take oral chemotherapy at home. But, they need to know how to take it and watch for side effects. Our team supports patients every step of the way.
Monitoring During Treatment
We watch patients closely during chemotherapy. We check for treatment response and side effects. Regular blood tests, imaging, and clinical checks help us adjust the treatment as needed.
| Monitoring Aspect | Frequency | Purpose |
|---|---|---|
| Blood Tests | Weekly or Biweekly | To assess blood cell counts and liver function |
| Imaging Studies | Every 3-6 months | To evaluate treatment response and detect any recurrence |
| Clinical Assessments | At each chemotherapy session | To monitor side effects and overall health |
By staying proactive in monitoring, we can quickly address any problems. This ensures the best experience for patients during adjuvant chemotherapy.
Managing and Minimizing Side Effects of Adjuvant Chemotherapy
Managing side effects of adjuvant chemotherapy is key to keeping patients well. As we deal with cancer treatment, we must tackle the challenges of adjuvant chemotherapy.
Common Acute Side Effects
Adjuvant chemotherapy can cause fatigue, nausea, and hair loss. These symptoms can really affect a patient’s life. Fatigue is not just feeling tired but also includes mental and emotional exhaustion.
To help, doctors often suggest medication and lifestyle changes. For example, anti-nausea meds can help with nausea from chemotherapy.
Long-Term Side Effect Considerations
Long-term side effects can also happen, sometimes years after treatment. These might include cognitive changes, heart problems, or secondary cancers. It’s important to know about these possible long-term effects.
Regular follow-up care is key to managing these effects. This includes check-ups and screenings to catch any issues early.
Supportive Care Strategies
Supportive care is vital in managing chemotherapy side effects. It includes nutritional counseling, psychological support, and physical therapy. This approach helps improve patients’ overall quality of life.
Also, new supportive care methods are being developed. For example, scalp cooling can help prevent hair loss from chemotherapy.
By adding these supportive care strategies to treatment plans, doctors can provide better care. This addresses the many challenges patients face during adjuvant chemotherapy.
Conclusion: Balancing Benefits and Risks in Adjuvant Cancer Care
Adjuvant chemotherapy is key in cancer treatment. It helps lower the chance of cancer coming back. Knowing the good and bad sides helps patients and doctors make better choices.
The aim is to find the right balance in treatment. Every patient is different, so treatments must fit their needs. Good care means looking at each person’s cancer and health carefully.
By focusing on the patient, we can make treatments work better and cause less harm. Keeping up with new ways in cancer care is important. This helps us give the best treatment possible.
FAQ
What is adjuvant chemotherapy, and how does it differ from other types of chemotherapy?
Adjuvant chemotherapy is a treatment given after primary therapy, like surgery or radiation. It aims to reduce cancer recurrence by killing any remaining cancer cells. It’s different from neoadjuvant chemotherapy, which is given before primary treatment. Palliative chemotherapy is used to manage symptoms and slow disease progression in advanced cancer.
How does adjuvant chemotherapy work to prevent cancer recurrence?
Adjuvant chemotherapy targets small clusters of cancer cells that have spread from the primary tumor. By killing these cells, it reduces the risk of cancer coming back and improves patient outcomes.
What factors influence doctors’ decisions to recommend adjuvant chemotherapy?
Doctors consider several factors when recommending adjuvant chemotherapy. These include the type and stage of cancer, risk assessment, and the patient’s overall health. The decision-making process between healthcare providers and patients is also important.
What are the common drug regimens used in adjuvant chemotherapy for breast cancer?
Common drug regimens for breast cancer include anthracycline-based and taxane-based regimens. The specific regimen depends on the patient’s cancer characteristics, overall health, and other factors.
How effective is adjuvant chemotherapy in improving outcomes for colorectal cancer patients?
Adjuvant chemotherapy significantly improves outcomes for colorectal cancer patients, mainly those with stage III disease. Studies show it reduces recurrence risk and improves survival rates.
What are the common side effects of adjuvant chemotherapy, and how can they be managed?
Common side effects include fatigue, nausea, hair loss, and increased infection risk. Supportive care strategies like anti-nausea medications, nutritional counseling, and emotional support can help manage these effects and improve quality of life.
How is adjuvant chemotherapy administered, and what is the typical treatment timeline?
Adjuvant chemotherapy is usually given intravenously, but some regimens are oral. The treatment timeline varies based on the regimen and patient response. Most regimens last several months.
Can adjuvant chemotherapy be used to treat other types of cancer beyond breast and colorectal cancer?
Yes, adjuvant chemotherapy is used for various cancers, including lung cancer, melanoma, and ovarian cancer. Treatment protocols and regimens vary based on cancer type and stage.
How does adjuvant chemotherapy impact patient survivorship and quality of life?
Adjuvant chemotherapy can greatly improve survivorship and quality of life by reducing recurrence risk and improving outcomes. It can also have long-term side effects. Patients should discuss their individual risks and benefits with their healthcare provider.