Last Updated on November 4, 2025 by mcelik

Osteoporosis affects over 10 million Americans, making it a big health issue. Weakened bones lead to a higher risk of fractures, affecting life quality.
It’s important to understand how bone density loss progresses. The condition goes through different stages, each with its own signs.
Knowing these stages is key for early action. This article will look at the 5 stages of osteoporosis. It will give insights into how to diagnose and manage it.
Key Takeaways
- Understanding osteoporosis stages is key for effective management.
- Osteoporosis diagnosis involves checking bone density loss.
- The condition goes through five distinct stages.
- Early detection can greatly improve treatment results.
- Knowing the stages helps in timely medical action.
Understanding What Is An Osteoporosis
Osteoporosis changes how bones work and makes them more likely to break. It’s a condition where bones get weaker, making them more prone to fractures.
Definition and Basic Concepts
Osteoporosis is a disease that makes bones lose density and structure. This leads to bones becoming thinner and more fragile, raising the chance of fractures. The name “osteoporosis” means “porous bones.”
The loss of bone density in osteoporosis happens when bone remodeling goes wrong. Normally, bones are rebuilt by cells that break down and build up bone. But in osteoporosis, this balance is off, causing bone loss.
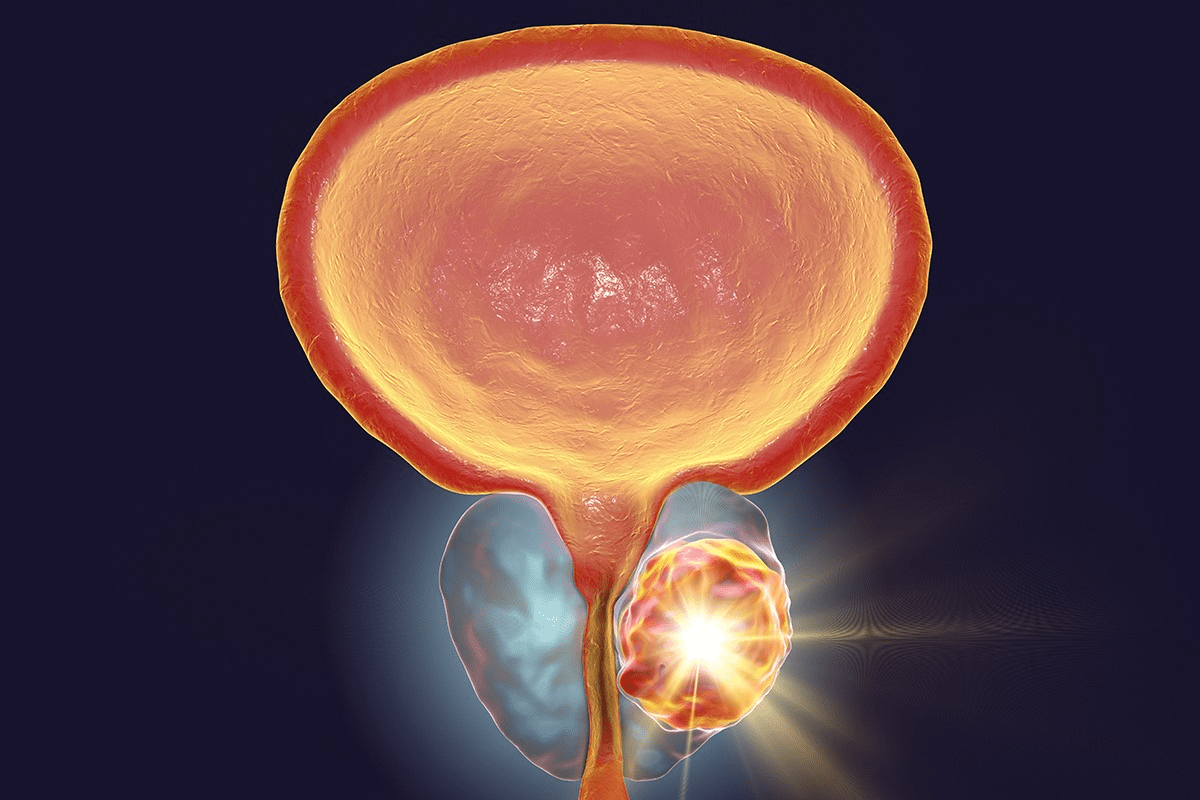
How Osteoporosis Affects Bone Structure
Osteoporosis makes bones more fragile by changing their structure. It affects both the outer dense layer (cortical bone) and the inner spongy layer (trabecular bone). As it gets worse, the trabecular bone gets less dense, and the cortical bone gets thinner.
Looking at normal and osteoporotic bones shows how it changes bone structure. Healthy bones have a dense, connected trabecular network. But osteoporotic bones have a sparse, disconnected network, making them weaker.
| Characteristics | Normal Bone | Osteoporotic Bone |
| Bone Density | High | Low |
| Trabecular Network | Dense and Connected | Sparse and Disconnected |
| Cortical Thickness | Thick | Thin |
Knowing how osteoporosis changes bones is key to treating it. Healthcare providers can then create better treatment plans to lower fracture risk and help patients.
The Silent Nature of Bone Loss
Osteoporosis is called the “silent disease” because it quietly weakens bones. Often, there are no signs until a bone breaks. This makes it hard to catch in its early stages.
Why Osteoporosis Is Called the Silent Disease

Osteoporosis is called the “silent disease” because it quietly weakens bones. This happens over years without clear signs. It’s a slow process that can sneak up on you.
Key factors contributing to its silent nature include:
- The gradual loss of bone density
- Lack of noticeable symptoms in the early stages
- The disease’s ability to affect different parts of the body at varying rates
Early Warning Signs Often Missed
In the early stages, osteoporosis often has no symptoms. But, there are some signs that are easy to miss. These include:
- Receding gums or changes in the fit of dentures, which can indicate bone loss in the jaw
- Weakened grip strength
- A decrease in overall physical performance or endurance
It’s important to notice these small changes. They can mean osteoporosis is starting. Catching it early is key to stopping it and avoiding breaks.
“The silent progression of osteoporosis highlights the need for early care. Knowing the risks and spotting early signs can help protect bones.”
Understanding why osteoporosis is called the “silent disease” helps. Knowing the early signs lets people take action to protect their bones.
Bone Health Fundamentals
Strong bones start with understanding bone health basics. It’s a mix of genetics, diet, and lifestyle. It includes bone remodeling, reaching peak bone mass, and how age and other factors affect bone density.
Normal Bone Remodeling Process
Bone remodeling is a constant cycle. It balances bone breakdown by osteoclasts and building by osteoblasts. This keeps bones healthy and controls calcium levels. Bone remodeling has four stages: activation, resorption, reversal, and formation.
In the activation stage, osteoclasts get ready to break down bone. Then, they do, releasing calcium into the blood. Next, the reversal phase gets the site ready for new bone. Lastly, osteoblasts make new bone matrix, which gets mineralized to form new bone.
Peak Bone Mass and Age-Related Changes
Peak bone mass is the highest bone density reached, usually in early adulthood. Genetics, diet, and lifestyle during growth and development affect it. A higher peak bone mass means a lower risk of osteoporosis later.
After reaching peak bone mass, bone density starts to decline with age. This decline can be sped up by hormonal changes, like in postmenopausal women.
Factors Affecting Bone Density
Many things can change bone density, like genetics, hormones, diet, and lifestyle. Genetics can make bones denser or less dense. Hormones like estrogen and testosterone are key in bone health.
What we eat, like calcium and vitamin D, is vital for bones. Our lifestyle, including exercise, smoking, and drinking, also affects bone density.
| Factor | Effect on Bone Density |
| Genetics | Influences peak bone mass and bone loss rate |
| Hormonal Status | Regulates bone metabolism; changes can affect bone density |
| Nutrition (Calcium, Vitamin D) | Essential for bone health; deficiencies can lead to lower bone density |
| Physical Activity | Weight-bearing exercise can increase or maintain bone density |
| Smoking and Alcohol | Can negatively impact bone health and density |
“Adequate nutrition and a healthy lifestyle are fundamental to achieving optimal peak bone mass and reducing the risk of osteoporosis in later life.”
— National Osteoporosis Foundation
How Osteoporosis Is Diagnosed
Osteoporosis diagnosis focuses on bone mineral density tests and other evaluations. Accurate diagnosis is key to knowing the disease’s stage and treatment options.
Bone Mineral Density (BMD) Testing
BMD testing is central to diagnosing osteoporosis. It measures the minerals in your bones, like calcium. The Dual-Energy X-ray Absorptiometry (DXA) scan is the most common test.
DXA Scan: A DXA scan is a non-invasive test that uses low-level X-rays. It checks the bone density in the hip and spine, where fractures often happen.
Understanding T-scores and Z-scores
BMD test results show T-scores and Z-scores. Knowing these scores helps understand your bone health.
- T-score: It compares your bone density to a healthy young adult of the same sex. A T-score of -2.5 or lower means you have osteoporosis.
- Z-score: It compares your bone density to an average person of the same age, sex, and size. A low Z-score means you might be losing bone density faster than expected.
| Score | Interpretation |
| T-score above -1.0 | Normal bone density |
| T-score between -1.0 and -2.5 | Osteopenia (low bone mass) |
| T-score of -2.5 or lower | Osteoporosis |
Other Diagnostic Tools and Assessments
While BMD testing is key, other tools help assess bone health and fracture risk.
“Additional tests may include vertebral fracture assessment, bone turnover markers, and other imaging studies to provide a complete view of bone health.”
These tools help doctors create a treatment plan tailored to you. This plan aims to manage osteoporosis and lower fracture risk.
The T-Score Classification System
Understanding the T-score system is key to managing osteoporosis well. It measures bone mineral density (BMD) to check fracture risk.
Normal Bone Density Range
A T-score compares your BMD to a healthy young adult of the same sex. A T-score above -1.0 means your bone density is normal. The World Health Organization (WHO) says this range is healthy.
Normal Bone Density: T-score above -1.0
Interpreting Your T-Score Results
Understanding T-score results is important. The WHO has set categories to help doctors diagnose osteoporosis and osteopenia.
- T-score above -1.0: Normal bone density
- T-score between -1.0 and -2.5: Osteopenia (low bone mass)
- T-score -2.5 or lower: Osteoporosis
The WHO explains, “The T-score is the number of standard deviations below the mean BMD for young adults of the same sex.”
How Doctors Use T-Scores for Treatment Decisions
Doctors make treatment plans based on T-scores, medical history, and other factors. They use T-scores to see how severe bone loss is and suggest treatments.
For example, someone with a T-score showing osteoporosis might get medication to strengthen bones. They might also be advised to change their diet and exercise routine.
“The T-score classification system is a valuable tool in the diagnosis and management of osteoporosis, enabling healthcare providers to make informed decisions about patient care.”
Stage 1: Normal Bone Density
At Stage 1, bone health is at its best. This is when we can do the most to keep our bones strong. We can make lifestyle choices and take steps to prevent problems.
Characteristics of Healthy Bone
Healthy bones are dense and strong. Normal bone density means bones are less likely to break. This is because bones are being replaced and built up at the right rate.
The bone remodeling process is key here. It replaces old bone with new. This keeps bones healthy and strong.
Preventive Measures at This Stage
It’s important to take steps to keep bones healthy at this stage. These include:
- Eating a diet full of calcium and vitamin D
- Doing regular exercises that make bones stronger
- Not smoking or drinking too much alcohol
- Keeping a healthy weight
By following these tips, we can lower our risk of osteoporosis later.
| Preventive Measure | Benefit |
| Balanced diet | Provides essential nutrients for bone health |
| Regular exercise | Strengthens bones and improves overall health |
| Avoiding harmful habits | Reduces risk factors associated with bone loss |
Knowing what makes bones healthy and taking action can help us keep our bones strong. This way, we can avoid osteoporosis.
Stage 2: Osteopenia – The Precursor Stage
Understanding osteopenia is key because it’s a warning sign. It means you might be at risk for osteoporosis.Osteopenia means bones are weaker than normal but not yet osteoporotic.
Defining Osteopenia vs. Osteoporosis
Osteopenia and osteoporosis are both about bone density. Osteopenia is a step before osteoporosis. It shows your bones are denser than in osteoporosis but not as strong as they should be. Doctors use a T-score from Bone Mineral Density (BMD) tests to tell them apart.
T-Score Range for Osteopenia (-1.0 to -2.5)
The T-score is important for diagnosing osteopenia and osteoporosis. A T-score between -1.0 and -2.5 means you have osteopenia. A T-score of -1.0 or higher is normal. A score below -2.5 means you have osteoporosis.
| T-Score Range | Diagnosis |
| -1.0 and above | Normal Bone Density |
| -1.0 to -2.5 | Osteopenia |
| Below -2.5 | Osteoporosis |
Intervention Strategies for Osteopenia
Acting early is important for osteopenia. Changing your lifestyle can help a lot. Eating well, exercising, and not smoking or drinking too much alcohol are good steps. Sometimes, doctors might suggest medicine to help your bones.
It’s vital for people with osteopenia to work with their doctors. They need to create a plan that’s right for them.
Stage 3: Mild Osteoporosis
Getting a mild osteoporosis diagnosis is a big step. It shows you need to act fast to stop your bones from getting worse. At this point, your T-score is between -2.5 and -3.5, showing you’ve lost some bone mass.
Clinical Presentation and T-Score Range
Most people with mild osteoporosis don’t feel any pain. But, getting your bones checked regularly is key to catching it early. The T-score range for mild osteoporosis is -2.5 to -3.5. This means your bone density is lower than normal but not too bad.
The signs of mild osteoporosis might include:
- Slightly decreased height
- Minor back pain
- Increased risk of fractures, mainly in the spine, hip, or wrist
| T-Score Range | Clinical Presentation | Risk Level |
| -2.5 to -3.5 | Minimal symptoms; possible minor back pain or height loss | Moderate risk of fractures |
Treatment Approaches for Mild Osteoporosis
Dealing with mild osteoporosis means stopping bone loss and avoiding fractures. Here’s how:
Lifestyle Modifications: Eating right to get enough calcium and vitamin D is important. Also, doing exercises that make your bones stronger is key.
Medications: Bisphosphonates can slow bone loss and lower fracture risk.
It’s vital to keep checking your bone density. This helps see if your treatment is working and if you need to change it.
Stage 4: Moderate Osteoporosis
Moderate osteoporosis is a serious stage where bones are more likely to break. At this point, bones have lost a lot of density. This makes them very fragile and prone to fractures.
Increased Fracture Risk and Symptoms
People with moderate osteoporosis face a higher risk of breaking bones, often in the hips, spine, and wrists. Symptoms can include:
- Back pain due to vertebral fractures
- Loss of height over time
- Stooped posture or curvature of the spine
- Fractures from minor falls or stresses
Fracture risk assessment is key at this stage. Doctors use the FRAX score to predict the chance of a major osteoporotic fracture in the next 10 years.
Comprehensive Management Strategies
Managing moderate osteoporosis needs a mix of lifestyle changes, nutrition, and sometimes medicine.
Lifestyle changes are a big part and include:
- Regular exercise, such as weight-bearing and resistance training
- Stopping smoking and drinking less alcohol
- Steps to prevent falls, like making your home safer
Nutritional interventions aim to get enough calcium and vitamin D. These are vital for strong bones. If you don’t get enough from food, supplements might be suggested.
For many, medication is needed to lower the risk of fractures. Common medicines are bisphosphonates, denosumab, and teriparatide.
It’s important to keep an eye on things and follow up regularly. Bone density tests and doctor visits help see if the treatment is working. They also help make changes if needed.
Stage 5: Severe Osteoporosis
Severe osteoporosis is the most advanced stage of bone loss. It greatly affects a person’s quality of life. At this stage, bone density is very low, often with a history of fractures.
T-Score Below -3.5 and Existing Fractures
A T-score below -3.5 shows severe osteoporosis. This means bone density is more than 3.5 standard deviations below a healthy adult’s. People at this stage often have fractures, affecting their mobility and independence.
Impact on Quality of Life
Severe osteoporosis has a big impact on life. It can cause chronic pain, loss of height, and a stooped posture. These changes make everyday activities hard.
It also affects mental health, leading to depression and anxiety. The fear of fractures can make people less active, worsening bone loss.
Advanced Treatment Options
Despite the challenges, there are advanced treatments for severe osteoporosis. These include:
| Treatment Option | Description | Benefits |
| Medications | Drugs that help to strengthen bones or reduce bone loss. | Can reduce the risk of fractures, slow down bone loss. |
| Physical Therapy | Exercises tailored to improve mobility and strength. | Enhances mobility, reduces the risk of falls. |
| Lifestyle Changes | Dietary adjustments and lifestyle modifications. | Improves overall bone health, reduces risk factors. |
Advanced treatment plans are often a team effort. They involve healthcare providers from different fields. The goal is to improve life for those with severe osteoporosis, reducing pain and fracture risk.
Types of Osteoporosis
Osteoporosis is divided into primary and secondary types based on its causes. Knowing the difference helps us understand bone loss better. It also guides how to treat it.
Primary Osteoporosis (Type 1 and Type 2)
Primary osteoporosis is the most common type. It’s linked to aging and hormonal changes. It has two subtypes: Type 1 and Type 2.
Type 1 Primary Osteoporosis mainly affects postmenopausal women. It happens because estrogen levels drop, causing fast bone loss, mainly in trabecular bone.
Type 2 Primary Osteoporosis, or senile osteoporosis, hits both men and women over 70. It’s due to aging. It’s caused by less bone formation and more bone breakdown.
| Characteristics | Type 1 Primary Osteoporosis | Type 2 Primary Osteoporosis |
| Primary demographic | Postmenopausal women | Men and women over 70 |
| Cause | Drop in estrogen levels | Aging process |
| Main bone affected | Trabecular bone | Both cortical and trabecular bone |
Secondary Osteoporosis and Its Causes
Secondary osteoporosis comes from medical conditions or treatments that harm bones. It’s different from primary osteoporosis. It can happen at any age, not just because of aging.
Some common causes include:
- Endocrine disorders (e.g., hyperthyroidism, hyperparathyroidism)
- Gastrointestinal diseases (e.g., celiac disease, Crohn’s disease)
- Long-term use of certain medications (e.g., corticosteroids, anticonvulsants)
- Rheumatologic disorders (e.g., rheumatoid arthritis)
A medical expert says, “Finding and treating the cause of secondary osteoporosis is key. It helps prevent more bone loss.”
“The presence of an underlying condition or medication that contributes to osteoporosis requires a complete treatment plan. It must address both the osteoporosis and its cause.”
– Medical Expert
Knowing the types of osteoporosis and their causes is vital for effective treatment. Healthcare providers can create specific plans. This is based on whether a patient has primary or secondary osteoporosis.
Progression of Osteoporosis Over Time
Understanding how osteoporosis progresses is key to effective treatment. Osteoporosis is a chronic condition where bone density gradually decreases. This leads to a higher risk of fractures.
Natural History of Bone Loss
Bone loss is a natural part of aging. But in osteoporosis, it happens faster. Normally, bone is remodeled, with old bone being replaced by new. In osteoporosis, the old bone is removed faster than new bone is made, causing a net loss of bone mass over time.
The rate of bone loss varies among individuals. It’s influenced by genetics, hormonal changes, and lifestyle. For example, postmenopausal women lose bone density quickly due to lower estrogen levels.
Factors That Accelerate Progression
Several factors can make osteoporosis progress faster. These include:
- Lifestyle Factors: Smoking, drinking too much alcohol, and a sedentary lifestyle can all contribute to faster bone loss.
- Nutritional Deficiencies: Not getting enough calcium and vitamin D can harm bone health.
- Medical Conditions: Certain conditions, such as hyperthyroidism and rheumatoid arthritis, can increase the risk of osteoporosis.
- Medications: Long-term use of corticosteroids and certain other medications can lead to bone loss.
Knowing these factors is important for managing osteoporosis. By addressing risk factors, individuals can slow the disease’s progression and lower their fracture risk.
Visual Differences: Normal vs. Osteoporotic Bone
It’s important to know how normal and osteoporotic bones look different. Osteoporosis makes bones weaker and more likely to break. Doctors use special images to see these differences.
Microscopic Changes in Bone Architecture
Osteoporotic bones look different under a microscope. The process that makes bones strong is off balance. This leads to weaker bones.
The inside of osteoporotic bones is less dense. Normal bones have a strong network inside that helps them stay strong.
| Characteristics | Normal Bone | Osteoporotic Bone |
| Bone Density | High | Low |
| Trabecular Network | Dense | Sparse |
| Bone Porosity | Low | High |
X-ray and Imaging Appearances
X-rays show how bones look different in osteoporosis. Osteoporotic bones are less dense and look more like glass.
Dual-energy X-ray absorptiometry (DXA) is used to measure bone density. It compares your bone density to a healthy young adult’s. A lower score means you might have osteoporosis.
Other tools like computed tomography (CT) and magnetic resonance imaging (MRI) help doctors see bone health. They can spot fractures or other problems.
Treatment Approaches Across Different Stages
Managing osteoporosis well means using a mix of treatments that change as the disease gets worse. The goal is to meet the patient’s needs at each stage.
Lifestyle Modifications and Nutrition
Making lifestyle changes is key in fighting osteoporosis at every stage. Eating right is important, focusing on calcium and vitamin D for strong bones. A diet full of fruits, veggies, and whole grains is best.
Also, regular exercise, like weight-bearing and resistance workouts, keeps bones strong. This can lower the chance of breaking bones.
For some, taking supplements is needed to get enough calcium and vitamin D. It’s also wise to cut down on too much caffeine and alcohol, as they can harm bones.
Medication Options and Their Mechanisms
There are many medicines for osteoporosis, each working in its own way. Bisphosphonates help keep bones dense by stopping bone loss. Denosumab targets a protein that breaks down bones.
| Medication | Mechanism of Action | Stage of Osteoporosis |
| Bisphosphonates | Reduce bone resorption | Stage 2-5 |
| Denosumab | Inhibits bone breakdown | Stage 3-5 |
| Teriparatide | Stimulates bone formation | Stage 4-5 |
When Surgical Intervention May Be Necessary
In severe cases of osteoporosis, surgery might be needed, like for fractures. Vertebroplasty and kyphoplasty can fix broken vertebrae and ease pain.
Choosing surgery depends on the patient’s health, how bad their osteoporosis is, and any other health issues they have.
Living With Osteoporosis: Practical Considerations
Living with osteoporosis means you need to be careful and take steps to stay healthy. People with osteoporosis should use a wide range of strategies to manage their condition well.
Fall Prevention Strategies
Stopping falls is key for those with osteoporosis. Falls can cause fractures and more problems. Here are some ways to prevent falls:
- Remove tripping hazards like loose rugs and clutter
- Make sure your home is well-lit, focusing on hallways and stairs
- Put handrails in places like bathrooms and stairs
- Use non-slip mats in the shower or bathtub
Pain Management Techniques
Many people with osteoporosis deal with chronic pain. Here are some ways to manage pain:
- Medication: There are many drugs that can help with pain, from over-the-counter to prescription.
- Physical therapy: Gentle exercises and therapy can help move better and feel less pain.
- Alternative therapies: Things like acupuncture, massage, and relaxation exercises can also help.
It’s important to work with a doctor to create a pain management plan that’s right for you.
Adaptive Equipment and Home Modifications
Changing your living space can make it safer and more comfortable for those with osteoporosis. This includes:
- Using tools like reachers and grabbers to avoid straining
- Modifying your home with walk-in showers, raised toilet seats, and more
- Arranging furniture to make paths clear and avoid tripping
These changes can help you stay independent and avoid injuries.
Conclusion
Understanding and managing osteoporosis needs a full approach. It covers all stages of the condition. Each stage has its own challenges and chances for help.
Knowing the stages of osteoporosis is key to managing it well. It helps people take steps to keep their bones strong and avoid fractures.
Managing osteoporosis means making lifestyle changes, eating right, and sometimes taking medicine. By being proactive, people can lower the risks of osteoporosis and live well.
In short, an osteoporosis summary shows how early detection and treatment are vital. Understanding the condition helps people make smart choices about their health. This leads to better health outcomes.
Effective managing osteoporosis needs teamwork between healthcare providers and patients. This ensures treatment plans fit each person’s needs.
FAQ
References
What is osteoporosis?
Osteoporosis is a condition where bones lose density and strength. This makes bones fragile and increases the risk of fractures.
What are the stages of osteoporosis?
Osteoporosis has stages from normal bone density to severe. Osteopenia is a stage before osteoporosis. Stages are measured by T-scores, comparing bone density to a healthy young adult.
What is a normal bone density score?
A normal bone density score is a T-score of -1.0 or above.
What is osteopenia?
Osteopenia means bone density is lower than normal but not low enough for osteoporosis. It has a T-score between -1.0 and -2.5.
How is osteoporosis diagnosed?
Doctors use Bone Mineral Density (BMD) testing to diagnose osteoporosis. This test measures bone density and compares it to a healthy young adult. The results are given as a T-score.
What is a T-score?
A T-score compares bone density to a healthy young adult. It helps diagnose osteoporosis and osteopenia.
What is severe osteoporosis?
Severe osteoporosis has a T-score below -3.5 and often includes existing fractures. It greatly increases the risk of more fractures and can affect quality of life.
How does osteoporosis progress over time?
Osteoporosis can get worse over time due to age, hormonal changes, and lifestyle. The rate of worsening varies by individual.
What are the treatment options for osteoporosis?
Treatments for osteoporosis include lifestyle changes, nutrition advice, medication, and sometimes surgery. The right treatment depends on the osteoporosis stage and individual risk factors.
How can osteoporosis be prevented?
Preventing osteoporosis means living a healthy lifestyle. This includes eating well, exercising regularly, and avoiding smoking and too much alcohol.
What is the difference between Type 1 and Type 2 osteoporosis?
Type 1 osteoporosis happens in postmenopausal women and causes fast bone loss. Type 2 osteoporosis is age-related and affects both men and women, leading to slow bone density decline.
Can osteoporosis be treated?
Yes, osteoporosis can be treated. There are medications that help improve bone density, reduce fracture risk, and manage symptoms.
What are the symptoms of osteoporosis?
Osteoporosis often has no symptoms until a fracture happens. Some people might feel back pain, lose height, or notice posture changes due to vertebral fractures.
How can I manage osteoporosis?
Managing osteoporosis involves lifestyle changes and medical treatment. Changes include preventing falls, managing pain, and using adaptive equipment. Medical treatment aims to improve bone density and lower fracture risk.
- Petersen, S. G., & Waehrens, E. E. (2020). Osteoarthritis, mobility-related comorbidities and mortality: An overview of meta-analyses. Journal of Clinical Rheumatology, 27(7), 269–275. https://www.researchgate.net/publication/347972649_Osteoarthritis_mobility-related_comorbidities_and_mortality_an_overview_of_meta-analyses