Last Updated on November 25, 2025 by Ugurkan Demir
At Liv Hospital, we understand the complex nature of heart failure. Decompensated congestive heart failure (CHF) is a serious condition. It happens when the heart can’t keep up with blood circulation. Learn what is decompensated congestive heart failure and how it differs from compensated.
We know that decompensated heart failure is a critical condition that needs quick medical help. It’s important to know the difference between decompensated and compensated heart failure. Compensated heart failure means the heart can manage blood flow, even with some problems.
To understand decompensated congestive heart failure, we need to know the basics of heart failure.
The heart pumps blood all over the body. It brings oxygen and nutrients to tissues and takes away waste. Its normal function is key to our health. The heart works through electrical impulses, muscle contractions, and a system of valves and chambers.
Heart failure happens when the heart can’t pump enough blood. This can be due to electrical problems, valve issues, or muscle conditions. The heart’s efficiency drops, causing fatigue, shortness of breath, and more.
In early heart failure, the body tries to help by changing how it works. It increases heart rate, makes the heart chambers bigger, and uses certain systems. These changes can help for a while, but they can also make heart failure worse over time.
It’s important to know about decompensated congestive heart failure to manage heart failure well. This condition happens when the heart can’t pump blood right. It makes symptoms worse, causing fluid buildup and swelling.
Decompensated CHF means the heart can’t keep blood flowing well. Fluid builds up in the lungs and body. This is serious and often needs quick medical help to avoid getting worse.
This condition is very important because it can harm patients a lot. It can lead to more health problems, death, and high medical costs. Doctors need to understand this to help patients better.
Heart failure can get worse in two ways: acute decompensation and chronic decompensation. Acute means symptoms get much worse fast, needing emergency care. Chronic means it gets worse slowly over time.
Telling the difference is key for treatment. Acute needs quick action, while chronic needs long-term care and lifestyle changes.
The heart’s failure to pump blood is due to many reasons. These include too much pressure, weak heart muscle, or problems with heart valves.
Knowing why the heart fails is vital for treatment. It helps doctors find the root cause and manage symptoms better.
Heart failure can be either compensated or decompensated. Compensated heart failure means the heart works well enough. Decompensated heart failure has severe symptoms.
Heart failure has a range from stable to unstable. Compensated heart failure is when the heart adapts to its reduced function. It keeps a good cardiac output through various mechanisms.
Decompensated heart failure happens when these mechanisms fail. This leads to a big drop in heart function and severe symptoms.
Compensated heart failure shows mild symptoms like shortness of breath or fatigue. These symptoms can be managed with treatment.
Decompensated heart failure has severe and sudden symptoms. These include severe dyspnea, orthopnea, and acute pulmonary edema.
Patients with compensated heart failure can do some physical activities. But they have some limits.
Those with decompensated heart failure see a big drop in their ability to do things. This severely affects their quality of life.
The outlook for heart failure patients differs based on their state. Those in a compensated state have a better chance of recovery.
Decompensated heart failure, on the other hand, raises the risk of hospitalization, illness, and death. This highlights the need for quick and effective treatments.
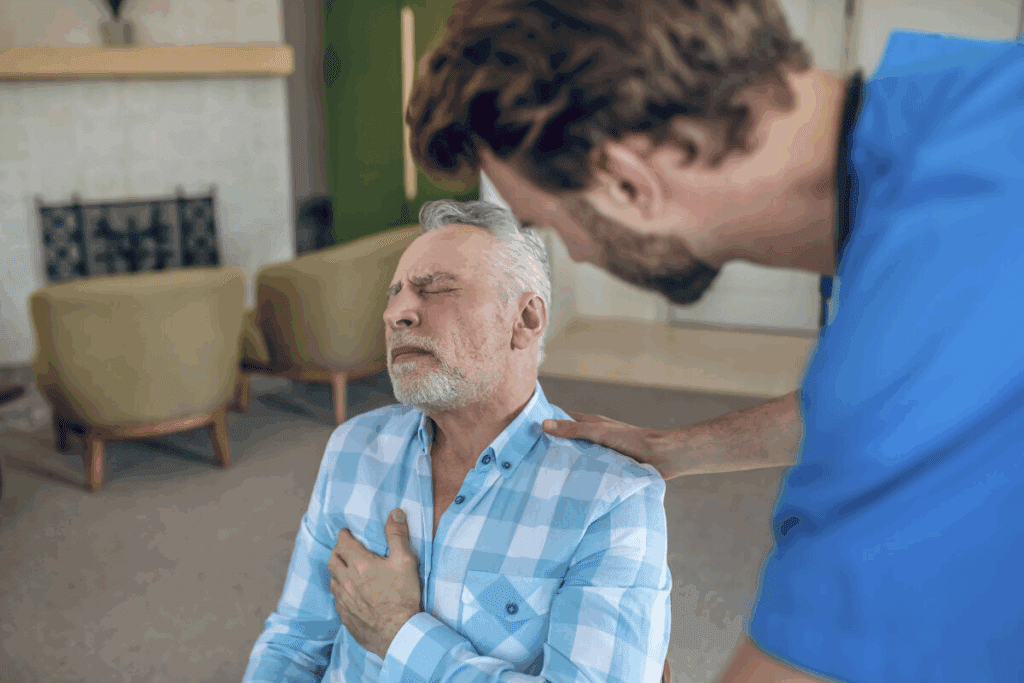
Decompensated heart failure brings severe symptoms that greatly affect a patient’s life. These signs and symptoms are alarming and need quick medical help. We will look at these symptoms, which are key for early detection and treatment.
Respiratory distress is a major symptom of decompensated heart failure. It shows as dyspnea or shortness of breath. This happens even when resting, due to fluid in the lungs.
Patients might find it hard to breathe when lying down. Or they might wake up with shortness of breath.
Fluid buildup is another symptom, causing edema or swelling in the legs, ankles, and feet. This happens because the heart can’t pump well, leading to fluid in the body. The swelling can be pitting, leaving an indentation, and often comes with weight gain.
Decompensated heart failure also shows in the heart. Symptoms include palpitations, or irregular heartbeats that feel like pounding or fluttering. It can also cause hypotension or low blood pressure, leading to dizziness or fainting.
Some patients might feel chest pain or discomfort. This could mean coronary artery disease or other heart problems.
Decompensated heart failure also has systemic symptoms. These include fatigue, weakness, and feeling unwell. Patients might also lose their appetite, feel nauseous, or have stomach discomfort.
It’s important to recognize these symptoms for timely diagnosis and treatment. Early action can greatly improve outcomes and lower the risk of complications.
Understanding decompensated heart failure is key to better public health. It’s a big cause of illness, death, and high healthcare costs worldwide.
Decompensated heart failure hits a lot of people in the U.S. Over 6 million adults have heart failure, with many experiencing decompensation.
Heart failure gets more common with age. As more people get older, the problem will grow. Older adults face a higher risk of heart failure.
Decompensated heart failure leads to a lot of hospital stays in the U.S., over 1 million a year. These stays hurt patients’ quality of life and cost a lot of money.
| Year | Hospitalizations | Average Cost per Hospitalization | Total Healthcare Cost |
| 2020 | 1,000,000 | $11,000 | $11 billion |
| 2021 | 1,050,000 | $11,500 | $12.075 billion |
| 2022 | 1,100,000 | $12,000 | $13.2 billion |
Some groups face a higher risk of decompensated heart failure. These include older adults, people with conditions like high blood pressure and diabetes, and those with heart disease history.
Socioeconomic factors also matter. People with lower income often face less access to healthcare. This makes them more likely to experience decompensation.
Heart failure can suddenly get worse due to certain triggers. Knowing these triggers is key to stopping and managing this serious condition. We will look at the main causes that lead to this critical state.
Not taking heart failure medicines as directed is a big problem. It can make heart failure worse. Forgetfulness, cost worries, or not understanding the need for medicines are common reasons. Sticking to the treatment plan is vital for heart failure patients.
Eating too much salt can cause fluid buildup and extra work for the heart. Heart failure patients are told to eat less salt to avoid this. But, sticking to a low-sodium diet is hard, and not doing so can lead to serious problems.
Conditions like high blood pressure, diabetes, and kidney problems can make heart failure worse. They add to the heart’s workload and can cause decompensation if not managed well. Controlling these conditions is critical to prevent decompensation.
Stress from infections or anemia, and from extreme weather, can also cause decompensation. These stressors increase the heart’s demand for oxygen and nutrients. Reducing these stressors can help prevent decompensation.
Understanding and tackling these common triggers and causes helps healthcare providers. They can then create better strategies to stop decompensation and help heart failure patients.
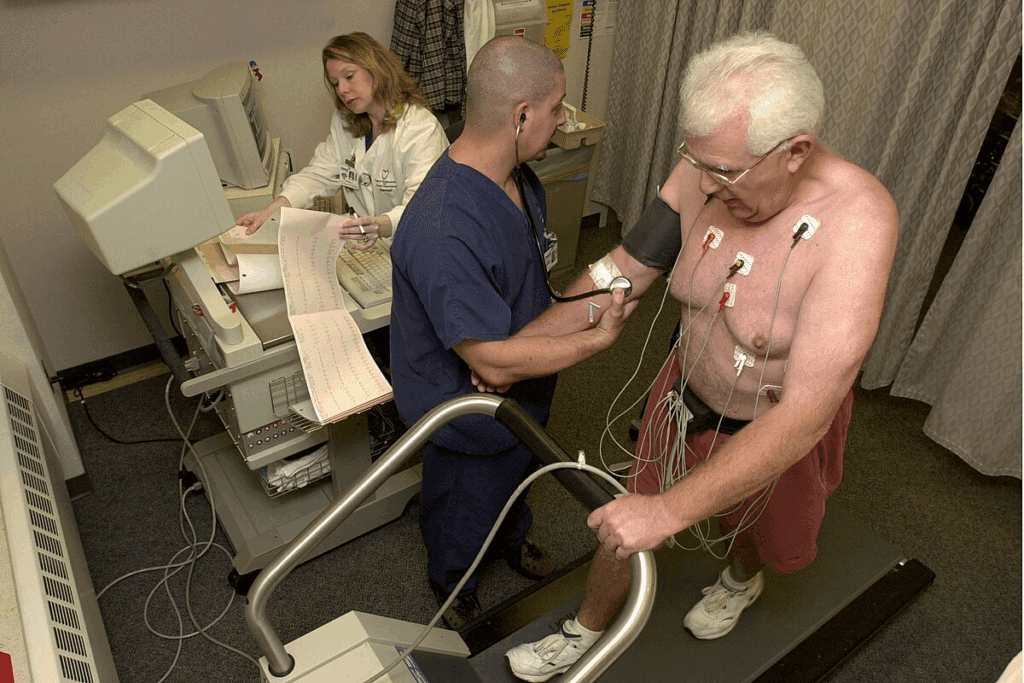
Getting a correct diagnosis for decompensated cardiac failure is key. It needs a mix of clinical checks, lab tests, and imaging studies. We’ll look at how these methods help spot and treat decompensated heart failure well.
First, a detailed clinical check and physical exam are done. This step looks at the patient’s health history, symptoms, and physical signs. We check for jugular venous distension and peripheral edema. We also watch for respiratory distress signs like fast breathing and trouble breathing when lying down.
Labs are vital in diagnosing decompensated cardiac failure. Tests like natriuretic peptides (BNP or NT-proBNP) are key. They show heart failure when levels are high. Other tests, like complete blood count (CBC), electrolyte levels, and renal function tests, help find causes and complications.
Imaging studies are key for checking the heart’s structure and function. Echocardiography is a main tool for looking at the left ventricle, valves, and pericardium. Chest X-ray shows signs of lung congestion. Cardiac MRI gives detailed heart images and function checks.
In serious cases, hemodynamic monitoring is needed. It tracks heart and blood vessel pressures, often with a Swan-Ganz catheter. This monitoring helps see how bad the heart failure is and if treatments are working.
Managing decompensated heart failure needs quick and effective treatment. This condition makes the heart unable to pump enough blood. It’s a serious issue that can be life-threatening if not treated right away.
The first step in treating decompensated heart failure is to stabilize the patient. This often means being in the hospital for close monitoring. Emergency steps include:
These actions help stabilize the patient’s condition and improve symptoms.
Medicines are key in managing decompensated heart failure. They help reduce symptoms, improve life quality, and slow disease growth. Common medicines include:
| Medication Class | Examples | Purpose |
| ACE Inhibitors | Lisinopril, Enalapril | Lower blood pressure and reduce heart workload |
| Beta-Blockers | Metoprolol, Carvedilol | Slow heart rate and lower blood pressure |
| Diuretics | Furosemide, Spironolactone | Reduce fluid and ease symptoms |
These medicines are often used together for better results.
Device-based therapies are also used for decompensated heart failure. They include:
These devices can greatly improve survival and quality of life for some patients.
Specialized centers like Liv Hospital offer advanced treatments for severe heart failure. These may include:
These treatments are for patients with severe, hard-to-treat heart failure. They are provided by a team of heart failure specialists.
Decompensated congestive heart failure is a serious condition that can be life-threatening. We’ve looked at the differences between compensated and decompensated heart failure. We’ve also discussed the signs and symptoms of decompensation and the treatment options.
It’s important for both healthcare providers and patients to understand decompensated congestive heart failure. Knowing what triggers decompensation helps prevent it. Healthcare providers can then create effective treatment plans.
In summary, decompensated congestive heart failure is a critical condition that needs immediate medical care. We hope this article helps everyone understand this complex condition better. This understanding can lead to better outcomes for those affected.
Decompensated congestive heart failure is a serious condition. The heart can’t pump enough blood. This leads to symptoms like shortness of breath, fatigue, and fluid buildup.
Compensated heart failure means the heart has adjusted to its reduced function. It keeps blood flow somewhat normal. Decompensated heart failure, on the other hand, means the heart’s adjustments fail. This leads to poor blood flow and severe symptoms.
Signs and symptoms include respiratory distress and fluid retention. Other symptoms are cardiovascular manifestations and systemic symptoms like fatigue, weakness, and confusion.
Common triggers and causes include not taking medication as directed and dietary indiscretions. Other causes are comorbid conditions and stressors from the environment and body.
It’s diagnosed through clinical evaluation, lab tests, imaging studies, and hemodynamic monitoring.
Treatment includes emergency management and pharmacological interventions. It also includes device-based therapies and advanced treatments at specialized centers.
Decompensated heart failure is a big health issue in the United States. It leads to high hospitalization rates and healthcare costs, mainly affecting vulnerable populations.
Cardiac decompensation is when the heart’s compensatory mechanisms fail. This results in inadequate blood flow and severe symptoms.
Uncompensated heart failure is another name for decompensated heart failure. It’s when the heart’s compensatory mechanisms fail, causing inadequate blood flow and severe symptoms.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!