For those fighting blood cancers, bone marrow transplants are a ray of hope. Yet, this lifesaving step also brings the risk of a complex immune reaction called Graft Versus Host Disease (GVHD).
GVHD happens when the transplanted cells see the host’s body as foreign. They then attack it. This can cause serious problems, affecting the patient’s life quality and survival chances.
At Liv Hospital, we know how critical it is to manage GVHD well. Our care is focused on the patient, using the latest evidence. We aim to provide top-notch treatment, supporting our patients every step of the way.
Key Takeaways
- Graft Versus Host Disease is a serious complication that can occur after bone marrow or stem cell transplants.
- The condition arises when the transplanted cells recognize the recipient’s body as foreign and attack it.
- Effective management of GVHD is key to better patient outcomes and quality of life.
- Liv Hospital’s approach to GVHD care is patient-centered and based on the latest evidence.
- Comprehensive support is given to patients throughout their treatment journey.
What Is GVHD? Defining Graft Versus Host Disease
Graft Versus Host Disease, or GVHD, is a big worry for people getting bone marrow transplants. It happens when the donor’s immune cells see the recipient’s body as different and attack it. This is a big problem with bone marrow transplants where the donor and recipient are not genetically the same.
The Basic Mechanism of GVHD
The basic mechanism of GVHD is when donor T-cells see the recipient’s tissues as foreign and attack them. This can cause inflammation and damage in organs like the skin, liver, and gut.
Why GVHD Occurs After Transplantation
GVHD happens after a transplant because the donor’s immune cells see the recipient’s body as different. The genetic differences between them start an immune response, causing GVHD. Knowing how this works is key to finding ways to stop and manage GVHD.
The Science Behind Bone Marrow and Stem Cell Transplants
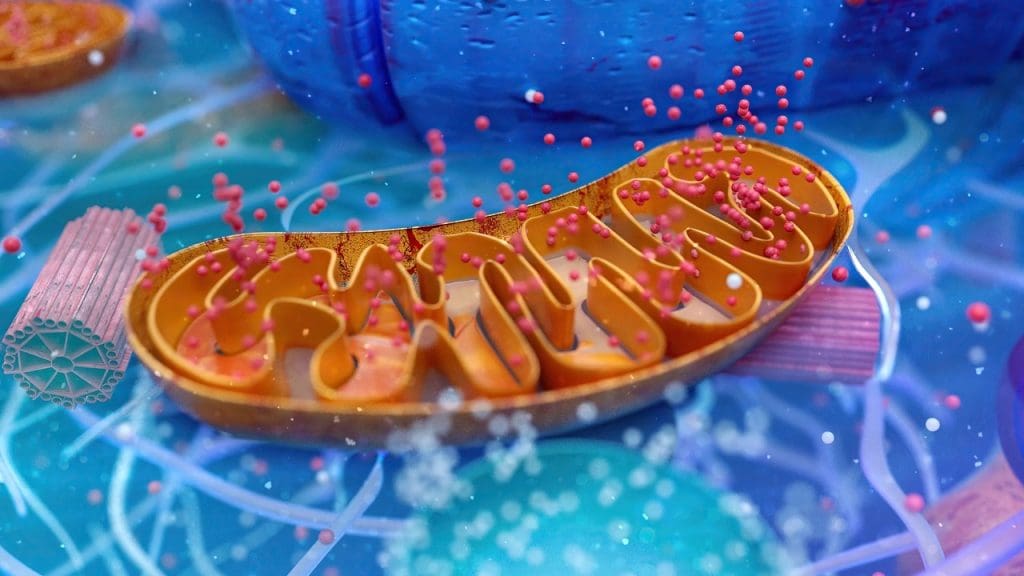
To understand GVHD, we must first grasp the basics of bone marrow and stem cell transplants. These procedures replace a patient’s sick or damaged bone marrow with healthy cells. They are used to treat many cancers and diseases.
How Transplantation Works
The transplant process starts with conditioning therapy to kill the old bone marrow. Then, healthy stem cells are given to the patient. These cells go to the bone marrow and start making new blood cells.
This whole process can take weeks to months. During this time, the patient’s immune system is very weak.
Types of Transplants
There are different types of bone marrow and stem cell transplants. Autologous transplants use the patient’s own stem cells. Allogeneic transplants use stem cells from a donor. Syngeneic transplants use stem cells from an identical twin.
Each type has its own risks and benefits. The choice depends on the patient’s condition and needs.
The Role of the Immune System in Transplantation
The immune system is key in transplantation. In allogeneic transplants, the donor’s immune cells might see the patient as foreign. This can lead to GVHD.
Understanding the immune system’s role is vital for managing GVHD and a successful transplant. As one expert says, “The immune system’s response to the transplant is a double-edged sword. It can fight cancer, but also cause GVHD.”
Acute vs. Chronic GVHD: Understanding the Differences
Knowing the difference between acute and chronic GVHD is key for treating patients after a transplant. GVHD is a complication that can happen after a bone marrow or stem cell transplant. It’s important to know which type a patient has to choose the right treatment.
Acute GVHD: Onset, Symptoms, and Progression
Acute GVHD usually starts within the first 100 days after a transplant. Its symptoms can be mild or severe. They often include a skin rash, liver problems, and stomach issues like diarrhea and pain.
The symptoms of acute GVHD can come on quickly. They can also get worse fast. So, it’s very important to diagnose and treat it quickly.
Chronic GVHD: Long-term Complications
Chronic GVHD starts after 100 days and can last for years. It can affect the skin, liver, mouth, and eyes. This can lead to problems like scarring, dryness, and vision issues.
Managing chronic GVHD is ongoing. It’s needed to improve the patient’s quality of life.
| Characteristics | Acute GVHD | Chronic GVHD |
|---|---|---|
| Onset | Within 100 days post-transplant | After 100 days post-transplant |
| Primary Symptoms | Skin rash, liver dysfunction, gastrointestinal issues | Skin, liver, mouth, and eye involvement |
| Duration | Typically short-term | Can be long-term, persisting for months or years |
A study shows that GVHD symptoms can be very different between acute and chronic forms. This means they need different treatments.
“GVHD remains a significant barrier to the success of allogeneic hematopoietic stem cell transplantation”
Understanding these differences is essential for giving the right care to patients.
Recognizing GVHD Symptoms by Affected Organ Systems
GVHD can affect many parts of the body, causing different symptoms. It’s important to know these symptoms to get the right treatment quickly.
Skin Manifestations
The skin is often hit hard by GVHD. Symptoms can be anything from mild rashes to severe blisters. Skin manifestations can be itchy or painful and may cover a lot of the body.
- Rashes or redness
- Itching or burning sensation
- Blisters or skin thickening
Gastrointestinal Symptoms
GVHD can also mess with the stomach and intestines. Symptoms include diarrhea, nausea, and abdominal pain. These can lead to dehydration and malnutrition if not managed well.
- Diarrhea or bloody stools
- Nausea or vomiting
- Abdominal cramps or pain
Liver Involvement
The liver can also be hit by GVHD, causing liver function tests to go off the rails. Symptoms include jaundice and high liver enzymes.
- Jaundice or yellowing of the skin
- Elevated liver enzymes
- Abnormal liver function tests
Ocular and Oral Complications
GVHD can also affect the eyes and mouth, causing dryness, irritation, and pain. Ocular symptoms can lead to serious issues like corneal ulcers if not treated.
- Dry eyes or ocular irritation
- Oral dryness or mucositis
- Pain or sensitivity to light
Other Organ Systems
GVHD can also hit other organs like the lungs and genital area. Symptoms vary widely depending on the organ affected.
- Respiratory issues
- Genital dryness or pain
- Other systemic symptoms
Risk Factors for Developing GVHD
It’s important to know the risk factors for GVHD after bone marrow transplant. GVHD happens when the donor’s immune cells see the recipient as foreign. They then attack the recipient’s tissues.
HLA Matching and Its Importance
The match between the donor and recipient’s HLA is key. A closer HLA match lowers GVHD risk. Doctors use HLA typing to find the best match. Siblings are more likely to match than unrelated donors.
Donor-Related Factors
Donor traits can raise GVHD risk. For example, female donors, older donors, or those with pregnancy history may have more alloantibodies. This could increase GVHD risk. Using peripheral blood stem cells instead of bone marrow also affects GVHD incidence.
Recipient-Related Factors
Recipient traits also play a role. Age, health, and past infections can impact GVHD risk. Older recipients face higher risks due to weaker immune systems and other health issues.
- Poor HLA matching between donor and recipient
- Donor characteristics (e.g., female gender, older age, history of pregnancy)
- Recipient factors (e.g., older age, underlying health conditions)
Knowing these risk factors helps doctors manage and prevent GVHD in bone marrow transplant patients.
The Diagnosis Process for GVHD
Diagnosing GVHD involves several steps. We look at clinical signs and run lab tests. Accurate diagnosis is key to starting the right treatment.
Clinical Evaluation
First, we check for symptoms like skin rashes and stomach problems. We also look at liver health. A detailed medical history and physical exam help spot GVHD.
Laboratory Tests and Biomarkers
Lab tests are essential for GVHD diagnosis. We test blood for liver function and bilirubin levels. These tests show how severe GVHD is.
Biopsy and Histological Confirmation
At times, a biopsy is needed to confirm GVHD. Tissue samples are examined under a microscope. This shows signs of GVHD like tissue damage and immune cell presence.
By using clinical signs, lab tests, and biopsy results, we can accurately diagnose GVHD. Then, we can create a treatment plan.
GVHD Grading Systems and Severity Assessment
GVHD grading systems are key in figuring out how severe the disease is. This helps doctors decide on the best treatment. Knowing how bad GVHD is lets doctors make treatment plans that work.
Acute GVHD Grading
Acute GVHD grading looks at how bad symptoms are by how many organs are affected. The most common system checks the skin, liver, and stomach. Grades range from I to IV, with I being mild and IV being very severe. This helps doctors know how much help a patient needs.
Chronic GVHD Classification
Chronic GVHD is sorted by how much it affects organs and the patient’s life quality. The National Institutes of Health (NIH) criteria are used to classify it. It’s divided into mild, moderate, or severe. This system makes it easier to assess and decide on treatments.
Treatment Approaches for GVHD
Managing GVHD requires different treatments, from first steps to new options. The right treatment depends on GVHD’s severity, the patient’s health, and affected organs.
First-Line Therapies
First treatments often use corticosteroids like prednisone to calm the immune system. Corticosteroids help manage GVHD symptoms for many, but some may not get better or face side effects.
“The initial treatment approach often sets the stage for the patient’s response to subsequent therapies.”
Steroid-Refractory GVHD Management
For those not helped by corticosteroids, other treatments are tried. Immunosuppressive agents like tacrolimus or sirolimus are used to control the immune system and reduce symptoms.
Emerging Treatments and Clinical Trials
New GVHD treatments are being tested in clinical trials. These include cellular therapies like mesenchymal stem cells and new drugs targeting GVHD pathways.
Supportive Care Measures
Supportive care is key in GVHD management. It focuses on easing symptoms, preventing infections, and ensuring nutrition. Multidisciplinary care teams work together to improve GVHD patients’ lives.
GVHD Prevention Strategies
Preventing GVHD is key for successful bone marrow or stem cell transplants. We use many strategies to lower GVHD risk. This improves patient outcomes and quality of life.
Prophylactic Medications
Prophylactic medications are vital in preventing GVHD. Immunosuppressive drugs like cyclosporine and tacrolimus are used to weaken the immune system. This reduces GVHD risk. These drugs can be used alone or together for better results.
The right medication depends on the transplant type, donor-recipient match, and patient risk factors.
T-Cell Depletion and Other Preventive Approaches
T-cell depletion is another way to prevent GVHD. It reduces T-cells in the graft, lowering GVHD risk. Other methods include ATG (anti-thymocyte globulin) and post-transplant cyclophosphamide.
These methods are effective, mainly in haploidentical transplants. Tailoring these strategies to each patient helps prevent GVHD better.
The Graft-Vers The Silver Lining
GVHD is a tough condition but it also offers a chance to fight cancer. This part of GVHD is seen as a big plus in treating some cancers.
How GVHD Can Help Fight Cancer
The graft-versus-tumor effect is when donor immune cells attack the recipient’s cancer cells. This is very important for people getting bone marrow transplants for blood cancers. Research shows that those with GVHD have a lower chance of cancer coming back.
A study on leukemia patients who got stem cell transplants found a big drop in relapse rates for those with GVHD. You can learn more about this on Vaia’s Immunobiology resources.
Balancing GVHD and Anti-Cancer Benefits
It’s important to balance the good of GVHD with its risks. Managing GVHD well is key to getting its cancer-fighting benefits without too many side effects. Scientists are working hard to find ways to make GVHD’s benefits stronger while making it less severe.
Living with GVHD: Patient Perspectives and Quality of Life
Living with Graft-Versus-Host Disease (GVHD) can be tough. But, knowing about it and how to manage it can really help. GVHD happens after a bone marrow transplant. It’s when the donated immune cells attack the body of the person who got the transplant.
Coping Strategies for Patients
Patients with GVHD can find ways to cope well. Following treatment plans and talking openly with doctors are key. Also, making your home safe can help avoid problems.
Support Resources and Patient Communities
Support groups and communities are very important for those with GVHD. Support groups let patients share and get emotional support. Getting accurate info and education programs helps patients manage their GVHD better.
Conclusion: The Future of GVHD Management and Research
As we learn more about Graft Versus Host Disease (GVHD), it’s clear we need more research. Good GVHD management means using the latest research and treatments. We’re working on new ways to treat GVHD and prevent it.
New discoveries in immunotherapy and allogeneic stem cell transplantation are helping. These advances could make GVHD less common and less severe. More research will help us understand how GVHD works, improving care for patients.
We must keep studying GVHD and working together. This includes researchers, doctors, and patients. Together, we can find better ways to manage GVHD. This will make life better for those dealing with this condition.
What is GVHD, and how does it occur after a bone marrow or stem cell transplant?
GVHD, or Graft Versus Host Disease, is a complication after a bone marrow or stem cell transplant. It happens when the donor’s immune cells react against the recipient’s body.
What is the difference between acute and chronic GVHD?
Acute GVHD occurs within the first few months after a transplant. Symptoms include skin rash, diarrhea, and liver issues. Chronic GVHD can happen months or years later, affecting more organs.
What are the symptoms of GVHD, and how do they manifest in different organ systems?
GVHD symptoms vary by organ. Common signs include skin rash, diarrhea, liver problems, and eye or mouth issues.
What are the risk factors for developing GVHD, and how can they be managed?
Risk factors for GVHD include HLA mismatching and donor and recipient factors. Managing these risks helps prevent GVHD through medications and T-cell depletion.
How is GVHD diagnosed, and what is the role of biopsy in confirming the diagnosis?
GVHD diagnosis involves clinical evaluation, lab tests, and biomarkers. Biopsy confirms the diagnosis and assesses GVHD severity.
What are the treatment approaches for GVHD, and how are they determined?
GVHD treatment includes first-line therapies and steroid-refractory management. Treatment choice depends on GVHD severity, as graded by acute and chronic GVHD systems.
Can GVHD be prevented, and what strategies are used to prevent it?
Yes, GVHD prevention is possible through prophylactic medications, T-cell depletion, and HLA matching.
Is there a beneficial aspect to GVHD, and how can it be balanced with the risks?
GVHD can fight cancer, known as the graft-versus-tumor effect. Balancing this benefit with GVHD risks is key for better patient outcomes.
How can patients cope with GVHD, and what support resources are available?
Patients with GVHD can use coping strategies and support resources. These help improve quality of life and offer emotional support.
What is the future of GVHD management and research?
Ongoing research and advancements are vital for better GVHD management. New treatments and clinical trials promise to enhance patient care and quality of life.
References
- National Center for Biotechnology Information (NCBI) / Books: https://www.ncbi.nlm.nih.gov/books/NBK538235/
- Blood Cancer United: https://bloodcancerunited.org/treatment/types-treatment/stem-cell-transplantation/graft-versus-host-disease



































