Last Updated on October 21, 2025 by mcelik
For patients with blood cancers, finding a stem cell donor is key. At Liv Hospital, we focus on innovative, patient-focused care. We use haploidentical hematopoietic stem cell transplantation (HLA-haplo HSCT). This method uses stem cells from a donor who shares half of the recipient’s HLA markers, often a family member.
This method makes finding a donor easier, helping those without a full match. Thanks to new treatments, the risks of serious side effects have dropped. Now, haploidentical transplantation is a safe choice for many.
Key Takeaways
- Haploidentical stem cell transplant uses donors with half-matched HLA markers, typically family members.
- This approach increases donor availability for patients with blood cancers.
- Advances in medical technology have improved the safety and efficacy of haploidentical transplantation.
- Liv Hospital is committed to providing innovative, patient-centered care for international patients.
- Haploidentical transplantation is a viable option for patients without a fully matched donor.
Understanding Stem Cell Transplantation Basics
Stem cell transplantation has changed how we treat blood diseases. It gives hope to patients all over the world. We’ll look at the basics of stem cell transplantation, its role in treating blood cancers, and the different types available.
The Role of Stem Cells in Treating Blood Cancers
Stem cells are key in treating blood cancers. They replace damaged or diseased cells with healthy ones. This helps regenerate a patient’s blood cells, potentially curing leukemia and lymphoma.
Stem cell transplants are a vital treatment. They offer a chance for long-term remission or even a cure.
Types of Stem Cell Transplants
There are several types of stem cell transplants. These include autologous (using the patient’s own cells) and allogeneic (using cells from a donor). Allogeneic transplants can be further divided into haploidentical (half-matched) and fully matched transplants.
Each type has its own benefits. The choice depends on the patient’s needs and the availability of a donor.
The Importance of HLA Matching
HLA (Human Leukocyte Antigen) matching is key in stem cell transplantation. It ensures the donor and recipient are compatible. A close HLA match lowers the risk of graft-versus-host disease (GVHD).
While a fully matched donor is best, haploidentical transplants offer hope for those without a fully matched donor. This makes it possible for almost all patients to find a suitable donor.
In conclusion, knowing the basics of stem cell transplantation is important. It helps us understand the complexities and benefits of this treatment. By understanding stem cells, the different types of transplants, and the importance of HLA matching, patients can make informed decisions about their care.
Haploidentical Stem Cell Transplant: Definition and Fundamentals

Haploidentical stem cell transplant, or “half-matched” transplant, uses donors who share half of the recipient’s HLA markers. This method is key for patients needing a stem cell transplant, when a perfect match is not found.
What “Half-Matched” Really Means
“Half-matched” in haploidentical transplantation means the donor and recipient share only one set of HLA markers. HLA markers are proteins on white blood cells that help the immune system fight off foreign invaders. In a haploidentical transplant, the donor and recipient share one set of these markers, often found in families.
HLA Markers and Their Significance
HLA markers are vital in matching donors and recipients for stem cell transplants. They help prevent graft-versus-host disease (GVHD), a serious transplant complication. Knowing about HLA markers is key to finding suitable donors for haploidentical transplants.
The Growing Importance of Haplo Transplants
Haploidentical transplants are becoming more important. They help increase the donor pool, which is good for patients from diverse backgrounds. The table below shows important facts about haploidentical transplants.
| Aspect | Description |
|---|---|
| Donor Matching | Half-matched, typically family members |
| HLA Markers | Shared on one haplotype |
| Graft-versus-Host Disease Risk | Managed with post-transplant care |
| Donor Availability | Increased, specially for diverse populations |
As stem cell transplantation advances, haploidentical transplants will be more important. They will help treat blood cancers and other diseases.
Traditional Allogeneic Bone Marrow Transplantation (Allo BMT)
Allogeneic Bone Marrow Transplantation, or Allo BMT, is a complex medical procedure. It requires careful consideration of donor and recipient compatibility. “Allo BMT is a lifesaving treatment option for many patients with blood cancers or bone marrow disorders,” as emphasized by medical professionals in the field.
Definition and Process
Allo BMT involves transferring stem cells from a healthy donor to a patient. The goal is to replace the patient’s diseased or damaged bone marrow. This process starts with conditioning therapy to remove the patient’s existing bone marrow. Then, the donor’s stem cells are infused into the patient.
Full HLA Matching Requirements
A critical aspect of Allo BMT is Human Leukocyte Antigen (HLA) matching between the donor and recipient. Full HLA matching is essential to minimize the risk of graft-versus-host disease (GVHD) and ensure the success of the transplant. HLA markers are proteins on white blood cells that play a vital role in the immune system’s ability to distinguish between the body’s proteins and proteins made by foreign invaders.
Limitations in Donor Availability
The requirement for full HLA matching can significantly limit donor availability. It is challenging to find a perfectly matched donor, which is even harder for patients from diverse ethnic backgrounds. According to recent studies, “the likelihood of finding a fully HLA-matched donor varies significantly among different ethnic groups, affecting transplant accessibility.”
Understanding these challenges is key to developing strategies to improve donor availability and transplant outcomes.
Key Differences Between Haploidentical and Allo BMT
It’s important to know the differences between haploidentical stem cell transplant and allo BMT. These choices depend on several key factors. This knowledge helps both patients and healthcare providers make informed decisions.
Donor Selection Criteria
The main difference is in donor selection. For haploidentical transplants, a half-match family member can be a donor. This expands the donor pool. On the other hand, allo BMT needs a fully matched donor, like a sibling or an unrelated donor from registries. Some patients have found success with alternative donor options.
Conditioning Regimens
The conditioning regimen varies between the two transplants. Haploidentical transplants often need more intense conditioning. This is to lower the risk of graft rejection.
Graft-versus-Host Disease Management
Graft-versus-host disease (GVHD) is a big risk for both transplant types. But, GVHD management strategies differ. Haploidentical transplants might use post-transplant cyclophosphamide to reduce this risk.
Recovery Timeline Comparisons
Recovery times also differ. Both types need careful post-transplant care. But, haploidentical transplants might have a longer recovery. This is because of the higher risk of complications.
| Characteristics | Haploidentical Transplant | Allo BMT |
|---|---|---|
| Donor Matching | Half-match family member | Full match sibling or unrelated donor |
| Conditioning Regimen | Often more intense | Varies based on donor match |
| GVHD Risk | Higher risk, managed with post-transplant cyclophosphamide | Lower risk with full match donors |
| Recovery Timeline | Slightly longer | Varies based on donor match and patient health |
Patient Eligibility and Donor Selection for Haploidentical Transplants
Choosing the right donor is key in haploidentical transplant. We check each patient’s health to see if they’re a good fit for this treatment.
Ideal Candidates for Haplo Transplants
Those without a perfect match or who’ve had a transplant before might benefit from haploidentical transplants. Our team looks at each patient’s past health and current condition to decide.
Family Member Donor Assessment
Family members like parents, siblings, and kids are often donors. We check their HLA markers and health to see if they can safely give stem cells.
Advantages of Parent, Sibling, or Child Donors
Using family members has big benefits, like quick availability and lower GVHD risk. Our studies show they can match the success of unrelated donors.
| Donor Type | Advantages | Considerations |
|---|---|---|
| Parent | Quick availability, better HLA matching | Age-related health issues |
| Sibling | Higher matching chance, younger | Genetic similarities |
| Child | Motivated donor, better HLA matching | Age and health |
Special Considerations for Diverse Populations
Finding donors is tough for those from diverse backgrounds. Haploidentical transplants are a good option, as family members can often donate.
“Haploidentical transplants have changed stem cell transplantation, giving hope to those with few options.”
By carefully picking donors, we can improve haploidentical transplant results. This gives new hope to those with blood cancers.
The Haploidentical Transplant Procedure
The haploidentical transplant procedure is a detailed process. It starts with a thorough check-up and preparation. This first step is key to see if the patient is ready for the transplant.
Pre-Transplant Evaluation and Preparation
Before the transplant, patients go through a detailed check-up. This includes looking at their heart, lungs, and liver. It helps find any risks and makes sure they’re ready.
The treatment also starts early. It includes medicines to weaken the immune system. This helps prevent the body from rejecting the transplant.
Stem Cell Collection Methods
There are two main ways to get stem cells for a haploidentical transplant. These are Bone Marrow Harvest and Peripheral Blood Stem Cell Collection (PBSCT).
Bone Marrow Harvest
Bone marrow harvest takes stem cells directly from the donor’s bones. This is usually from the pelvic area. The donor is given anesthesia to make the process painless.
Peripheral Blood Stem Cell Collection (PBSCT)
PBSCT uses growth factors to move stem cells into the bloodstream. Then, a process called apheresis collects these stem cells from the blood.
The Transplantation Process
After collecting the stem cells, they are given to the patient through a vein. The stem cells then go to the bone marrow. There, they start making new blood cells.
Post-Transplant Care Protocol
After the transplant, patients need to be watched closely. They might face problems like graft-versus-host disease (GVHD) and infections. To prevent GVHD, they take medicines like cyclosporine and mycophenolate mofetil.
They also get support care. This includes blood transfusions and medicines to fight infections. It helps manage any side effects.
Knowing about the haploidentical transplant process helps patients and their families. It makes them understand this life-saving treatment better.
Benefits of Haploidentical Stem Cell Transplant
Haploidentical stem cell transplant is changing the game in stem cell therapy. It makes it easier for more patients to find a donor. This is a big win for those in need of a transplant.
Expanded Donor Availability
This method uses half-matched donors. This means more people can be donors. It’s a big help for those from different ethnic backgrounds who often can’t find a full match.
Reduced Time to Transplant
With more donors, patients can get transplanted faster. This is a big plus for those with serious or advanced diseases. Time is of the essence for them.
Benefits for Diverse Ethnic Populations
Patients from diverse backgrounds often have trouble finding a full match. Haploidentical transplantation offers a ray of hope to these patients.
Comparable Survival Outcomes to Fully Matched Transplants
Studies show haploidentical transplants work just as well as full matches. They have about 79% survival rates at one year. This makes haploidentical transplant a strong treatment choice.
Potential Complications and Management Strategies
Haploidentical donors in stem cell transplants come with risks. This method offers hope but also has complications to consider.
Unique Challenges in Haploidentical Transplants
Haploidentical transplants face challenges due to partial HLA matching. This can increase the risk of certain complications.
Graft Rejection
Graft rejection is a big risk, where the body rejects the stem cells. We use immunosuppressive therapy to help the body accept the transplant.
Graft-versus-Host Disease
Graft-versus-Host Disease (GVHD) is another risk. Here, the donor’s immune cells attack the recipient’s body. We manage GVHD with drugs and close monitoring.
Infection Risks and Prevention
Patients face infection risks due to weak immune systems. We prevent infections with antibiotics and watchful monitoring.
| Complication | Management Strategy |
|---|---|
| Graft Rejection | Immunosuppressive Therapy |
| Graft-versus-Host Disease | Immunosuppressive Drugs and Monitoring |
| Infection Risks | Antimicrobial Prophylaxis and Monitoring |
Understanding these complications and using effective strategies can improve outcomes. This is for patients getting haploidentical stem cell transplants.
Advanced Care Centers and Protocols
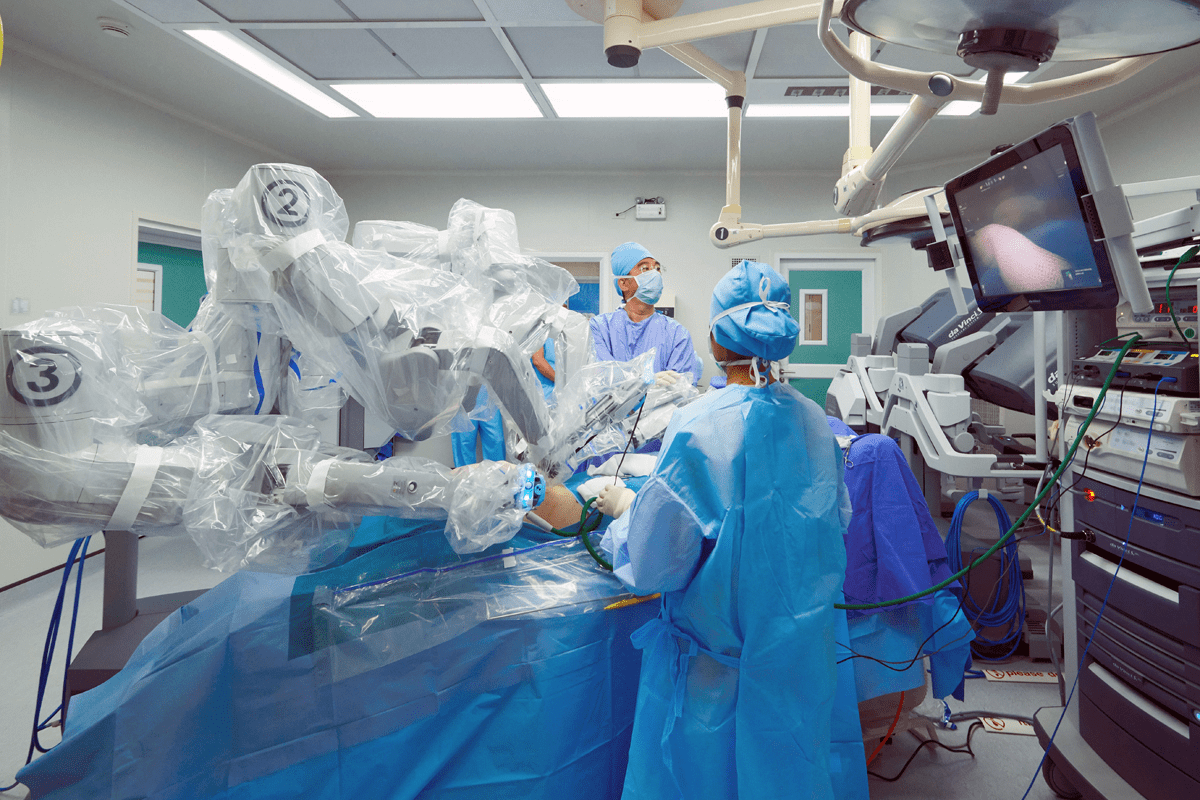
Innovative protocols and specialized care centers are making a big difference in haploidentical stem cell transplantation. Places like Liv Hospital lead the way. They use the latest technology and team up with many doctors to care for patients.
Multidisciplinary Team Approach
Success in advanced care centers comes from teamwork. Doctors like hematologists, oncologists, and immunologists work together. Together, they make sure each patient gets a treatment plan that fits their needs.
Evidence-Based Practices in Haplo Transplantation
These centers focus on using the latest research in their treatments. This keeps them up-to-date and able to offer the safest and most effective treatments.
Liv Hospital’s Approach to Haplotype Transplants
Liv Hospital is a top example of a center that has made haplotype transplant work better. They use the latest technology and focus on the patient. This way, they get the best results for those getting haploidentical stem cell transplants.
Latest Innovations in Transplant Protocols
The field of haploidentical stem cell transplantation is always getting better. New research and developments lead to better transplant methods. Advanced care centers are leading this progress, shaping the future of transplant medicine.
Conclusion: The Future of Haploidentical Transplantation
Advances in haploidentical stem cell transplant have greatly improved care for patients with blood cancers and other diseases. As we keep improving haplo transplant methods, the future looks bright. It offers hope to those without a fully matched donor.
Haploidentical transplantation is becoming more important. It makes more donors available, shortens wait times, and matches survival rates with fully matched transplants. Liv Hospital’s work shows the progress in bmt and haplo transplant technologies.
Research will keep improving, leading to better graft-versus-host disease management and infection prevention. The future of haploidentical transplantation is full of promise. We are dedicated to providing top-notch healthcare to international patients seeking advanced treatments.
FAQ
What is haploidentical stem cell transplantation?
Haploidentical stem cell transplantation uses a donor who is a half-match to the recipient. This means they share half of the recipient’s HLA markers. It’s a good option for patients who can’t find a fully matched donor.
How does haploidentical stem cell transplantation differ from traditional allogeneic bone marrow transplantation (allo BMT)?
The main difference is in who can donate. Allo BMT needs a fully matched donor. But haploidentical transplant allows for a half-match, often a family member. This makes it easier for more patients to get a transplant.
What is the significance of HLA matching in stem cell transplantation?
HLA matching is key because it lowers the risk of GVHD and graft rejection. HLA markers help the immune system tell self-cells from foreign ones.
Who can be a haploidentical donor?
Family members like parents, siblings, or children can often be half-matches. This makes it a good option for many patients.
What are the benefits of haploidentical stem cell transplantation?
It offers more donor options, quicker transplants, and works well for diverse ethnic groups. It also has survival rates similar to fully matched transplants.
What are the possible complications of haploidentical stem cell transplantation?
Risks include graft rejection, GVHD, and infections. But, better transplant methods and care have improved patient outcomes.
How is graft-versus-host disease (GVHD) managed in haploidentical transplants?
GVHD management uses immunosuppressive drugs and close monitoring. The treatment plan depends on the patient’s health and the transplant method.
What is the role of advanced care centers in haploidentical stem cell transplantation?
Centers like Liv Hospital are vital. They offer a team approach, evidence-based care, and new transplant methods. This helps improve patient results.
What does PBSCT stand for in medical terminology?
PBSCT means Peripheral Blood Stem Cell Collection. It’s a way to get stem cells from the donor’s blood.
What is the definition of BMT in medical terms?
BMT stands for Bone Marrow Transplantation, or stem cell transplant. It replaces a patient’s bone marrow with healthy stem cells, from themselves or a donor.
References
- National Center for Biotechnology Information (NCBI) / Books: https://www.ncbi.nlm.nih.gov/books/NBK536951/
- Blood / ASH Publications: https://ashpublications.org/blood/article/134/21/1802/428775/How-we-perform-haploidentical-stem-cell
- National Marrow Donor Program (NMDP) / Be The Match: https://www.nmdp.org/patients/understanding-transplant/haploidentical-transplant