Last Updated on October 20, 2025 by

As we look into new ways to manage multiple sclerosis (MS), hematopoietic stem cell transplantation (HSCT) stands out. It’s seen as a hopeful treatment, mainly for those with severe or hard-to-treat MS.
At Liv Hospital, we aim to offer top-notch healthcare with full support for international patients. We focus on care that puts the patient first and use the latest medical techniques. This is why we’re looking into HSCT as a possible treatment for MS.
HSCT uses autologous hematopoietic stem cell transplantation (AHSCT), a method that might slow down MS. By learning how chemotherapy works in HSCT and comparing it to usual treatments, we can help those looking for advanced treatments.
Key Takeaways
- HSCT is a promising therapy for aggressive or refractory MS.
- AHSCT has shown promise in reducing MS disease activity and progression.
- Chemotherapy is key in the HSCT process.
- HSCT might be a choice for those not helped by usual treatments.
- Liv Hospital is committed to giving full care to international patients.
Understanding Multiple Sclerosis and Current Treatment Landscape

To understand multiple sclerosis (MS), we must explore its causes and treatments. MS is a chronic disease where the immune system attacks the protective covering of nerve fibers. This leads to various neurological symptoms.
The Pathophysiology of Multiple Sclerosis
MS’s causes involve genetics and the environment. These factors trigger an immune attack on the nerve fibers’ protective sheath. This damage disrupts nerve signals, causing symptoms like numbness and vision problems.
Conventional Disease-Modifying Therapies (DMTs)
DMTs are key in treating MS. They aim to reduce relapses and slow disease growth. Treatments are divided into first and second lines based on disease severity and patient needs. Common DMTs include interferons and glatiramer acetate.
While DMTs help many, their success varies. Some patients see big improvements, while others continue to experience symptoms.
Limitations of Standard MS Treatments
Standard MS treatments have their limits. They can have side effects and require long-term use. Some patients may also develop antibodies that reduce treatment effectiveness. For aggressive MS cases, these treatments may not be enough.
Research suggests Hematopoietic Stem Cell Transplantation (HSCT) could be a better option for some. It has shown to reduce relapses and inflammation better than some DMTs in certain patients.
HSCT Treatment: Fundamentals and Mechanisms

For those with Multiple Sclerosis, Hematopoietic Stem Cell Transplantation (HSCT) is a game-changer. It aims to reboot the immune system. This method has caught a lot of attention for its unique way of working and its promise of long-term disease control.
Definition and Basic Principles
Hematopoietic Stem Cell Transplantation (HSCT) is a treatment that uses hematopoietic stem cells to rebuild the immune system. It starts with killing off the old immune cells with chemotherapy. Then, the patient’s own stem cells, saved before, are given back.
This “reset” aims to get rid of immune cells that attack the body in Multiple Sclerosis.
Types of Hematopoietic Stem Cell Transplantation
There are a few types of HSCT:
- Autologous HSCT: This is the most common for MS, where the patient’s own stem cells are used.
- Allogeneic HSCT: This uses stem cells from another person, but it’s less common for MS due to risks.
How HSCT “Resets” the Immune System
The HSCT process “resets” the immune system by first killing off the old cells with chemotherapy. Then, the new stem cells create a fresh immune system. This can help stop the disease from getting worse and even reduce symptoms.
Understanding HSCT helps us see its value in treating Multiple Sclerosis. Its ability to deeply reset the immune system brings hope to those with severe or hard-to-treat disease.
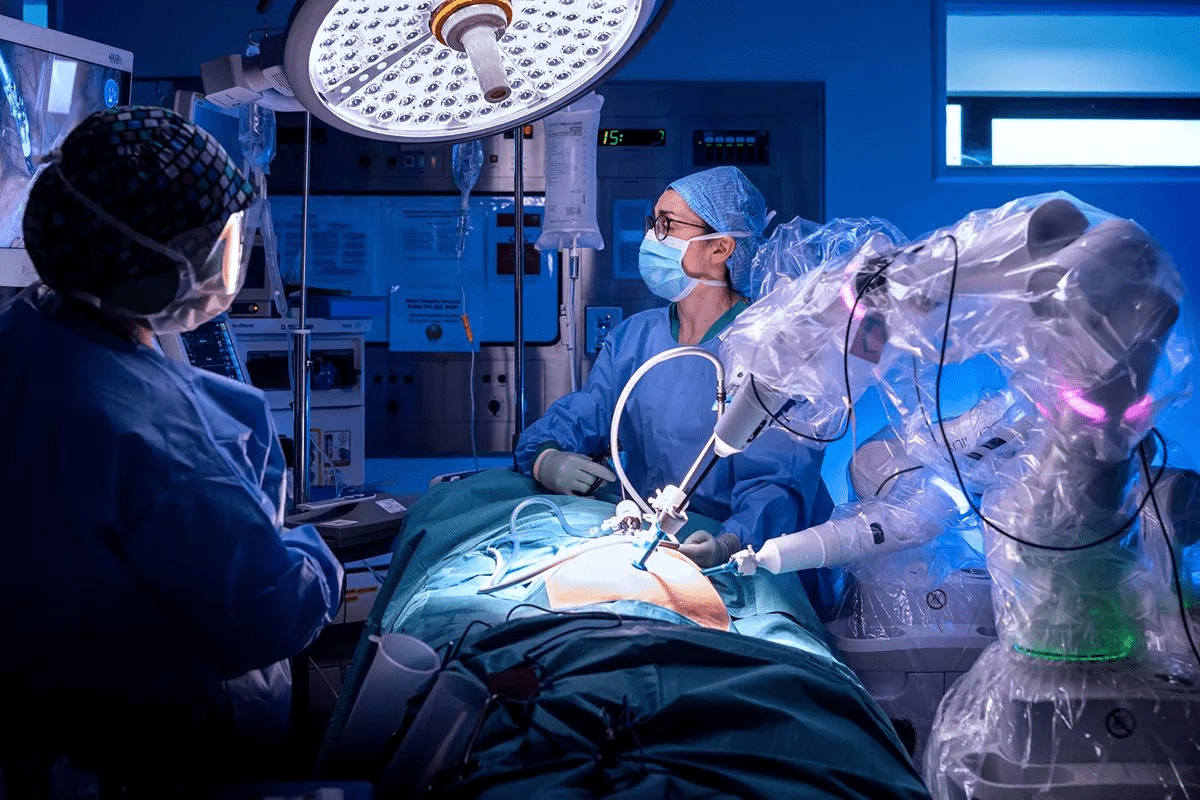
The HSCT Procedure for MS Patients
The HSCT procedure for MS patients involves several critical steps. At Liv Hospital, we have refined this process to ensure the best possible outcomes for our patients.
Pre-Transplant Evaluation and Preparation
Before undergoing HSCT, patients must undergo a thorough evaluation. This evaluation assesses their overall health and suitability for the procedure. Our team of specialists conducts a series of tests and consultations.
We also prepare patients emotionally and physically for the treatment. This includes explaining what to expect during each stage.
Pre-transplant evaluation is key. It helps identify any risks or complications that could arise. Our team reviews the patient’s medical history and current health status. This ensures the HSCT procedure is tailored to their specific needs.
Stem Cell Collection Process
The next step is the stem cell collection process. This involves mobilizing stem cells from the bone marrow into the bloodstream. Then, apheresis collects these cells.
We use state-of-the-art technology to make the collection process efficient and safe. Patients are closely monitored to manage any side effects. The collected stem cells are prepared for reinfusion after the conditioning regimen.
Conditioning Regimen (Chemotherapy)
The conditioning regimen, typically involving chemotherapy, is a critical component. This step is necessary to ablate the patient’s immune system. It makes way for the reinfused stem cells to rebuild a healthy immune system.
We carefully design the chemotherapy protocol. This balances efficacy with safety, minimizing side effects. For more detailed information on chemotherapy in HSCT for MS, visit our dedicated page on stem cell therapy for MS.
Stem Cell Reinfusion and Engraftment
After completing the conditioning regimen, the collected stem cells are reinfused into the patient’s bloodstream. This process is similar to a blood transfusion and is generally well-tolerated. The reinfused stem cells then migrate to the bone marrow, where they begin to produce new immune cells.
Engraftment is the final step. Here, the new immune system starts to function. Patients are monitored closely during this period. This ensures successful engraftment and manages any complications that may arise.
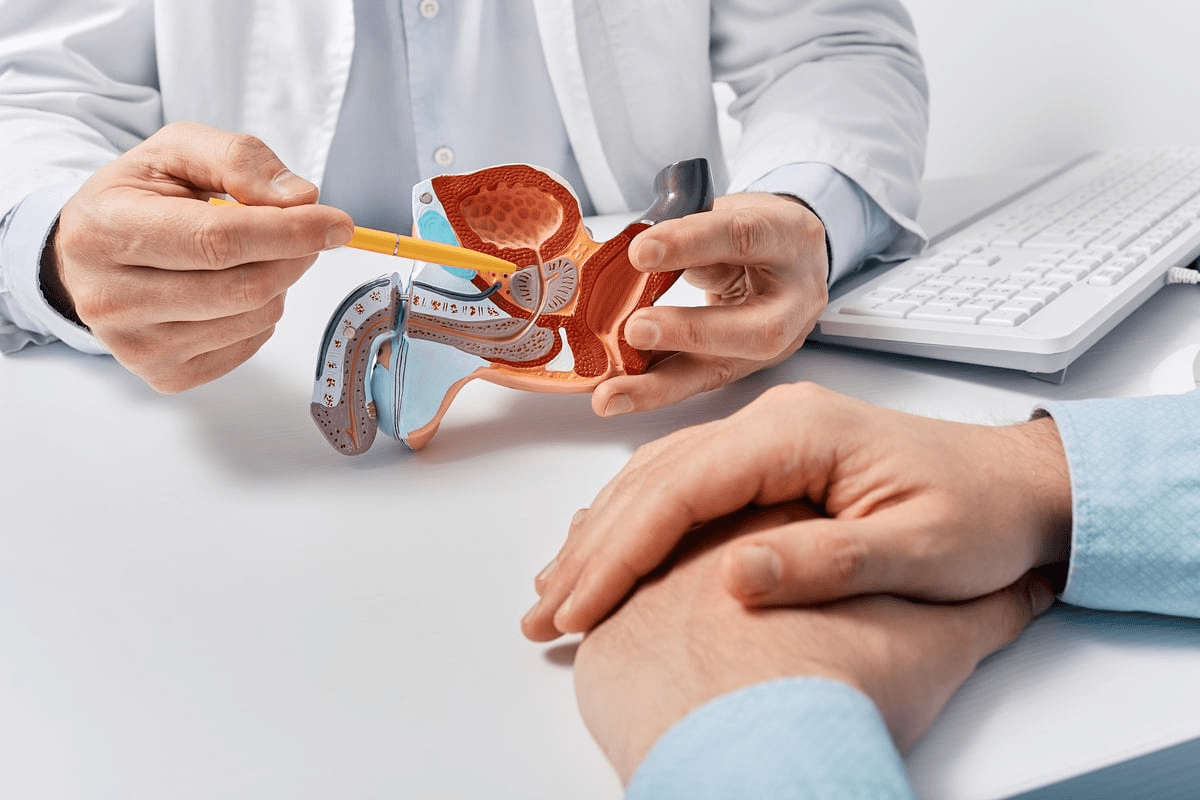
The Critical Role of Chemotherapy in HSCT for MS
Chemotherapy is key in Hematopoietic Stem Cell Transplantation (HSCT) for Multiple Sclerosis (MS). It gets rid of the old immune cells before adding new stem cells. This is vital for a new start for the immune system, which is essential for treating MS.
Why Immune System Ablation is Necessary
Chemotherapy is used to stop the immune system from attacking itself in MS patients. MS happens when the immune system mistakenly attacks the nerves. This leads to problems with communication between the brain and the body. By removing these bad immune cells, chemotherapy helps create a new, healthy immune system from the stem cells.
Types of Chemotherapy Regimens Used
There are many chemotherapy regimens used in HSCT for MS, each with its own use. The right one depends on the patient’s health, how severe their MS is, and what treatments they’ve had before.
| Chemotherapy Regimen | Description | Intensity |
|---|---|---|
| BEAM (Carmustine, Etoposide, Cytarabine, Melphalan) | A commonly used regimen that combines multiple chemotherapeutic agents. | High |
| Cyclophosphamide | Often used in combination with other agents or as part of a conditioning regimen. | Moderate to High |
| ATG (Anti-Thymocyte Globulin) | Used to deplete T-cells and prevent graft-versus-host disease. | Varies |
Managing Chemotherapy Side Effects
It’s important to manage chemotherapy side effects to keep patients safe and comfortable during HSCT. Side effects include nausea, fatigue, hair loss, and a higher risk of infections. To help, doctors use anti-nausea meds, nutrition support, and ways to prevent infections.
Differences from Cancer Chemotherapy Protocols
Chemotherapy for HSCT in MS is similar to cancer treatment but has key differences. MS treatment aims to be less harsh and focuses on stopping the immune system from attacking itself. The treatment plans are made to be effective but also to protect the patient’s quality of life.
Comparative Efficacy: HSCT vs. Standard MS Therapies
MS treatment is always getting better. Looking at how HSCT stacks up against standard therapies helps both patients and doctors. It’s key to know what each treatment offers and its limits.
Relapse Rate Reduction Comparisons
Research shows HSCT can cut down on relapses in people with relapsing-remitting MS. A study in a top medical journal found HSCT greatly lowers annual relapse rates. Some patients even stop having relapses altogether.
“HSCT has been linked to a big drop in relapse rates,” say experts. “It’s a hopeful treatment for those with aggressive MS.”
Impact on Disease Progression Metrics
HSCT also seems to slow or stop disease progression in some patients. This is a big plus over standard treatments that just slow it down.
Our review of studies shows HSCT can lead to better disability outcomes. This is based on the Expanded Disability Status Scale (EDSS).
MRI Outcomes and Lesion Activity
MRI results are key to seeing how well MS treatments work. HSCT has been shown to lower lesion activity and improve MRI results. This means less inflammation in the brain.
- Reduced gadolinium-enhancing lesions on MRI
- Decrease in new T2 lesions
- Stabilization or reduction in brain atrophy
Quality of Life Improvements
HSCT also brings big quality of life gains for MS patients. By cutting down on disease activity and possibly stopping it from getting worse, HSCT helps patients keep their skills and independence.
As we learn more about HSCT in MS treatment, it’s clear it’s a valuable choice for some patients. It offers not just health benefits but also a better life quality.
Patient Selection: Ideal Candidates for HSCT Stem Cell for MS
HSCT is seen as a hopeful treatment for tough MS cases. Finding the right patients is key. We look at many factors to make sure HSCT is safe and effective for each person.
MS Subtypes Most Responsive to Treatment
Some MS types do better with HSCT. Relapsing-remitting MS patients who haven’t gotten better with usual treatments are top picks. We also look at aggressive or quickly getting worse MS cases. HSCT can “reset” the immune system, helping these patients.
Age and Disease Duration Considerations
Age and how long you’ve had MS matter a lot. Younger patients with a shorter disease duration usually do better. They often have fewer health problems and a stronger immune system, which helps with recovery.
Prior Treatment Response Factors
Those who haven’t done well with many treatments or have bad side effects might get HSCT. We check how well they’ve done with previous treatments and the severity of side effects. For more on who can get HSCT, check Liv Hospital’s page on BM Transplantation.
Contraindications and Exclusion Criteria
Some health issues make HSCT not possible. These include severe organ problems, active infections, and serious brain issues. We do detailed checks to find out if these issues would make HSCT risky or not effective.
By picking patients carefully, we aim to make HSCT work best for them. This way, each person gets the right treatment for their specific needs.
Risks and Side Effects of HSCT and MS
For those thinking about HSCT for MS, knowing the risks is key. HSCT might help manage MS, but it comes with possible complications and side effects. It’s important to understand these.
Immediate Post-Procedure Complications
The HSCT process includes chemotherapy, which can cause immediate side effects. These include:
- Infections: The immune system is weakened, making infections more likely.
- Nausea and Vomiting: Chemotherapy can lead to nausea and vomiting, which are treated with medication.
- Hair Loss: Hair loss is common due to the chemotherapy.
- Fatigue: Feeling very tired is a common side effect during recovery.
These immediate issues are usually managed in the hospital. Patients get support to help deal with these effects.
Long-Term Health Considerations
After the immediate recovery, there are long-term health issues to consider for HSCT patients:
- Infertility: Chemotherapy might make it hard to have children.
- Secondary Autoimmune Disorders: There’s a chance of getting other autoimmune diseases after HSCT.
- Organ Damage: The treatment can harm organs like the liver and kidneys.
It’s vital for patients to talk to their doctors about these risks. This helps understand the long-term effects.
Mortality Rates in Current Practice
Mortality rates for HSCT have gone down thanks to better technology and care. Today, the death rate is usually between 1-3%. But, this can change based on several factors. These include the patient’s health, the treatment used, and the experience of the treatment center.
“The risk of dying from HSCT for MS is not small, but it has dropped a lot. This is thanks to better patient selection, treatment, and care after transplant.” – Expert in HSCT for MS
Risk-Benefit Analysis Compared to Standard Therapies
When thinking about HSCT for MS, it’s important to compare the risks and benefits to standard treatments. For some, the chance of better disease control and fewer relapses might be worth the risks of HSCT.
Deciding on HSCT involves looking at several things. These include how severe the disease is, how well previous treatments worked, and the patient’s overall health. Talking to a doctor is key to making a well-informed choice.
HSCT Success Rates and Long-Term Outcomes
Hematopoietic stem cell transplantation (HSCT) is a new hope for MS patients. It’s a treatment that can change the course of the disease for many. As more data comes in, it’s clear that HSCT can make a big difference.
Results for Relapsing-Remitting MS
HSCT works well for patients with relapsing-remitting MS. It reduces relapse rates and slows disease progression. For example, a study found that over 80% of relapsing-remitting MS patients stayed disease-free at five years after transplant.
The benefits of HSCT for relapsing-remitting MS are many:
- Reduced annualized relapse rate
- Slowing or halting of disease progression as measured by EDSS
- Improved or stabilized neurological function
- Significant reduction in MRI lesion activity
Outcomes for Progressive Forms of MS
While HSCT results for relapsing-remitting MS are promising, progressive MS outcomes are more varied. Research shows that HSCT can slow or stabilize disease progression in some progressive MS patients. The benefits might not be as strong as in relapsing-remitting MS.
A recent study found that patients with progressive MS who had HSCT saw a big drop in disability progression. Some even showed improvement in their neurological function.
Factors Predicting Treatment Success
Finding out who will do well with HSCT is key. Research has found several important factors:
- Younger age at the time of transplant
- Shorter disease duration
- Presence of inflammatory activity on MRI
- Absence of significant disability
Five and Ten-Year Follow-up Data
Long-term data is vital to understand HSCT’s lasting benefits. Studies with five and ten-year follow-ups have given us valuable insights.
A recent study showed that HSCT provided lasting benefits for MS patients. A significant number stayed free from disease progression at ten years after transplant. This highlights HSCT’s ability to control MS for a long time in the right patients.
The Patient Journey Through HSCT Treatment
The journey through HSCT treatment for MS is complex. It includes many stages from start to finish. This detailed process aims to give patients the best results from this advanced therapy.
Physical and Emotional Preparation
Before starting HSCT, patients must get ready physically and emotionally. Physical preparation means a full medical check-up to check health and find risks. This might include heart tests, lung function tests, and tests for infections. Emotional preparation is also key, as patients face stress and uncertainty. Counseling and support groups help patients and their families during this tough time.
Hospital Stay and Immediate Recovery
The hospital stay for HSCT usually lasts 2 to 4 weeks. During this time, patients are watched closely for any quick problems. Post-transplant care in the hospital deals with side effects like nausea, tiredness, and infection risk. Medical staff are always ready to help, ensuring a smooth recovery.
Post-Transplant Rehabilitation
After leaving the hospital, patients start a vital recovery phase. This time is for slowly getting better and rebuilding the immune system. They follow a special recovery plan that might include physical therapy, nutrition advice, and mental support. This helps them recover well and improve their life quality.
Long-Term Monitoring Requirements
Long-term monitoring is key after HSCT to watch how patients do and catch any late problems. Regular check-ups with the healthcare team are vital. They track disease activity, immune system recovery, and overall health. This ongoing care ensures the treatment plan is adjusted as needed and patients get the support they need.
Liv Hospital’s HSCT program shows its focus on patient care. It offers a supportive and structured environment throughout treatment. Understanding the HSCT journey helps patients prepare for its challenges and benefits.
Accessing HSCT: Treatment Centers and Financial Considerations
HSCT is a promising treatment for Multiple Sclerosis. But, getting access to it can be tricky. We need to look at the top treatment centers, the cost, and the full programs offered by hospitals.
Insurance Coverage and Reimbursement Status
Insurance can be a big hurdle for HSCT. Some plans cover it, but others don’t or need extra approvals. You should check your coverage and understand how to get reimbursed.
Working with the treatment center’s financial team can help with insurance issues and find financial help.
Liv Hospital’s HSCT Program
Liv Hospital has a top-notch HSCT program for MS. It has a team of experts and modern facilities. Their program includes all steps from before the transplant to aftercare.
Their program is tailored for each patient. Liv Hospital is known for its innovative treatments and focus on patients.
International Treatment Options
International options can offer specialized care and new therapies not found at home. Countries like the U.S., Germany, and Sweden are popular for medical tourism.
When looking at international options, check the team’s qualifications, care quality, and costs. Also, think about travel and accommodation for you and your caregivers.
Conclusion: The Evolving Role of HSCT in MS Treatment
HSCT for MS has become a promising treatment. It offers hope to patients with aggressive or treatment-resistant MS. By “resetting” the immune system, HSCT has shown to reduce disease activity and slow progression in some patients.
The role of HSCT in MS treatment is changing with new research and advancements. As we learn more about MS and improve HSCT techniques, we’ll see better patient selection and treatment outcomes.
More research is needed to fully understand HSCT’s benefits and risks for MS. Studies will help us know more about long-term effects and find the best patients for treatment. As we make progress in MS treatment, HSCT will become more important in managing the disease.
By focusing on HSCT research, we can improve patient care and offer new hope to those with MS.
FAQ
What is HSCT treatment for MS?
HSCT (Hematopoietic Stem Cell Transplantation) is a treatment for Multiple Sclerosis. It uses chemotherapy to remove the immune system. Then, it replaces it with new stem cells, effectively “resetting” the immune system.
How does HSCT compare to conventional MS therapies?
HSCT is more effective than traditional treatments in reducing relapses and slowing disease progression for some patients.
What is the role of chemotherapy in HSCT for MS?
Chemotherapy is used to destroy the immune system. This allows for the introduction of new stem cells. The type and intensity of chemotherapy depend on the HSCT protocol.
What are the possible risks and side effects of HSCT for MS?
Risks and side effects include immediate complications and long-term health issues. Mortality risks are also present. Yet, the benefits often outweigh the risks for certain patients, like those with aggressive MS.
Who is a good candidate for HSCT?
Good candidates have relapsing-remitting MS, are young, and have had the disease for a short time. They should not have responded well to traditional treatments. Criteria can vary by treatment center.
What is the success rate of HSCT for MS?
Success rates depend on MS subtype, patient age, and disease duration. Studies show significant relapse rate reductions and quality of life improvements for many patients.
What is the patient journey through HSCT like?
The journey includes preparation, hospital stay, rehabilitation, and long-term monitoring. Each step is vital for success.
What are the long-term outcomes of HSCT for MS?
Long-term data show HSCT can lead to sustained disease activity reductions and quality of life improvements. Five and ten-year follow-ups support its efficacy.
Is HSCT a cure for MS?
While not a cure, HSCT can significantly alter the disease course for many. It may lead to long-term freedom from disease activity.
What is the future of HSCT in MS treatment?
HSCT’s role in MS treatment is evolving with ongoing research. It is becoming a key option for certain patients.
References
- Burt, R. K., Craig, J. C., Oliveira, M., & others. (2013). Hematopoietic Stem Cell Therapy for Multiple Sclerosis: Top 10 Lessons Learned. Frontiers in Neurology / PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3557353/ PMC
- ClinicalTrials.gov. (n.d.). A Study of Autologous Hematopoietic Stem Cell Transplantation in Multiple Sclerosis (NCT04047628). Retrieved from https://clinicaltrials.gov/study/NCT04047628 ClinicalTrials
- (Duplicate of #2) Burt, R. K., Craig, J. C., Oliveira, M., & others. (2013). Hematopoietic Stem Cell Therapy for Multiple Sclerosis: Top 10 Lessons Learned. Frontiers in Neurology / PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3557353/ PMC