Last Updated on November 27, 2025 by Bilal Hasdemir
Ischemic heart disease (IHD), also known as coronary artery disease (CAD), happens when the heart muscle doesn’t get enough blood. This is because the coronary arteries are narrowed or blocked. It’s a big problem worldwide, leading to many deaths.
Studies show that IHD often comes from a heart attack. Over 800,000 Americans have a heart attack every year. EurekAlert reports that new ways to diagnose it are being looked into. These include using CXCR4-targeted PET/CT to see how the heart will work after a heart attack.
Key Takeaways
- Ischemic heart disease (IHD) is also known as coronary artery disease (CAD).
- IHD is characterized by reduced blood flow to the heart muscle.
- It is a leading cause of death worldwide.
- Acute myocardial infarction (AMI) is a major cause of IHD.
- Advanced diagnostic techniques are being developed to improve outcomes.
Understanding Ischemic Heart Disease
To grasp Ischemic Heart Disease, we need to look at its definition, its link to Coronary Artery Disease (CAD), and its worldwide impact. Ischemic Heart Disease (IHD) happens when the heart muscle doesn’t get enough blood flow. This leads to different symptoms. We’ll dive into IHD’s details, its medical terms, and how it compares to CAD.
Definition and Medical Terminology
Ischemic Heart Disease is when the heart muscle doesn’t get enough oxygen and nutrients because of less blood flow. This usually happens because the coronary arteries are narrowed or blocked. The term “ischemic” means less blood flow, and “heart disease” tells us which organ is affected.
IHD includes conditions like angina pectoris, myocardial infarction (heart attack), and sudden cardiac death. Knowing these terms is key for both patients and doctors to handle the disease well.
IHD vs. CAD: Are They the Same Condition?
Ischemic Heart Disease and Coronary Artery Disease are often mixed up, but they’re related but different. CAD is about the narrowing or blockage of the coronary arteries due to plaque buildup.
IHD is what happens when this reduced blood flow affects the heart muscle. So, CAD is the cause, and IHD is the effect. Not all CAD leads to IHD, but most IHD is caused by CAD. Knowing this is important for correct diagnosis and treatment.
Global Impact and Prevalence
Ischemic Heart Disease is a major cause of illness and death worldwide. The World Health Organization (WHO) says IHD causes over 9 million deaths each year. It’s one of the top reasons for death globally.
| Region | IHD Prevalence (%) | Annual Deaths (millions) |
|---|---|---|
| Global | 1.5 | 9.4 |
| North America | 2.1 | 1.3 |
| Europe | 2.5 | 1.8 |
| Asia | 1.2 | 5.6 |
The amount of IHD varies by area, due to lifestyle, diet, and genetics. Knowing these differences helps in making better prevention and treatment plans.
Pathophysiology of Ischemic Heart Disease
Ischemic Heart Disease (IHD) is caused by many factors that narrow and block coronary arteries. A key factor is atherosclerosis, where plaque builds up in artery walls.
Coronary Artery Narrowing and Blockage
Plaque buildup in coronary arteries narrows and blocks them. This plaque is made of lipids, inflammatory cells, and fibrous elements. As it grows, it can severely reduce blood flow to the heart.
This reduced blood flow can cause ischemia, which is worse during times of high heart activity.
Atherosclerosis Development Process
Atherosclerosis starts with endothelial dysfunction. Then, lipids and inflammatory cells enter the arterial wall. This leads to the formation of atherosclerotic plaques.
These plaques can become unstable and prone to rupture. Risk factors like hypertension, high cholesterol, diabetes, and smoking speed up this process.
Consequences of Reduced Blood Flow to Heart Muscle
Reduced blood flow to the heart muscle can cause serious problems. These include angina pectoris, myocardial infarction, and heart failure. Angina is chest pain from not enough oxygen during stress or exertion.
| Condition | Description | Consequences |
|---|---|---|
| Angina Pectoris | Chest pain due to reduced blood flow | Reduced quality of life, increased risk of MI |
| Myocardial Infarction | Death of heart muscle due to complete blockage | High morbidity and mortality, possible heart failure |
| Heart Failure | Reduced heart function due to chronic ischemia | Poor prognosis, significant impact on quality of life |
Understanding IHD’s pathophysiology is key to managing it. By tackling the causes and risk factors, healthcare can prevent its progression and improve outcomes.
Risk Factors for Developing IHD
Knowing the risk factors for Ischemic Heart Disease (IHD) is key to preventing and managing it. Many factors can lead to IHD. Identifying these can help us take steps to lower our risks.
Modifiable Risk Factors
Modifiable risk factors are things we can change. They include lifestyle choices and medical treatments. Key modifiable risk factors for IHD are:
- Smoking: Smoking damages blood vessels and increases the risk of blockages.
- Hypertension: High blood pressure can narrow and harden arteries, raising IHD risk.
- Diabetes: Diabetes can harm blood vessels and nerves, increasing IHD risk.
- High Cholesterol: High levels of LDL cholesterol can cause artery blockages, raising IHD risk.
- Obesity and Physical Inactivity: Being overweight or inactive can increase the risk of conditions leading to IHD.
By managing these modifiable risk factors, we can lower our chances of getting IHD.
Non-modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. These include:
- Age: IHD risk grows with age, with most cases in people over 65.
- Family History: A family history of IHD, even at a young age, raises risk.
- Gender: Men face higher IHD risk than women, but women’s risk increases after menopause.
- Genetic Predisposition: Some genetic conditions can increase IHD risk.
While we can’t change non-modifiable risk factors, knowing them helps us focus on modifiable ones. This way, we can reduce our overall risk.
By tackling both modifiable and non-modifiable risk factors, we can prevent or manage IHD effectively.
Clinical Manifestations of Ischemic Heart Disease
It’s key to know the different signs of Ischemic Heart Disease (IHD) for early treatment. IHD shows up in many ways, each affecting treatment and results.
Angina Pectoris: Types and Symptoms
Angina pectoris is a common sign of IHD. It feels like chest pain or discomfort due to heart not getting enough blood. This pain can spread to arms, back, neck, or jaw.
There are stable angina and unstable angina. Stable angina follows a pattern, while unstable angina is unpredictable and may mean a heart attack is coming.
“Angina is a warning sign that the heart is not getting enough oxygen-rich blood,” says why it’s important to notice and treat it.
Myocardial Infarction (Heart Attack)
A heart attack happens when a part of the heart doesn’t get enough blood. This is usually because of a blockage in a coronary artery. Symptoms include severe chest pain, shortness of breath, nausea, and feeling very tired.
Silent Ischemia: The Hidden Danger
Silent ischemia is when the heart doesn’t get enough blood without pain. It’s dangerous because it can cause a heart attack without warning. It’s more common in people with diabetes and can be found through tests like an electrocardiogram (ECG) during stress tests.
Heart Failure as a Consequence of Chronic Ischemia
Chronic ischemia can lead to heart failure. This is when the heart can’t pump enough blood for the body. Symptoms include dyspnea (shortness of breath), feeling very tired, and swelling in the legs.
Knowing the signs of IHD is vital for quick action. “Early detection and management of IHD can greatly improve patient outcomes and quality of life,” shows why being aware and proactive is so important.
Ischemic Heart Disease Diagnosis: Initial Assessment
Healthcare providers start by looking at a patient’s medical history, symptoms, and physical exam. This helps find who needs more tests.
Medical History and Symptom Evaluation
Looking at a patient’s medical history is key. We check for things like high blood pressure, diabetes, and high cholesterol. We also look at family history of heart disease.
Symptoms like angina pectoris, shortness of breath, and feeling tired are important. Knowing when and why these symptoms happen helps us understand how bad the heart disease is.
For example, people who smoke or don’t move much are at higher risk. A detailed look at symptoms can show patterns that point to IHD, like chest pain when active and better when resting.
Physical Examination Findings
A physical exam gives us clues about IHD. We listen for an S4 heart sound, which might mean the heart isn’t working right. We also look for signs of artery disease or fatty deposits in the skin.
We check for signs of heart failure too, like jugular venous distension or peripheral edema. These can happen if IHD is not treated.
Cardiac Biomarkers and Blood Tests
Cardiac biomarkers are very important for diagnosing IHD, mainly in heart attacks. We check for troponin and creatine kinase to see if the heart is damaged.
We also test blood for cholesterol, sugar, and other things that can increase heart disease risk. These tests help us understand how much risk a patient has and what to do next.
By using medical history, symptoms, physical exam, and biomarkers, we can accurately diagnose IHD. Then, we can plan the best treatment.
Advanced Diagnostic Methods for Ischemic Heart Disease
We use many advanced tests to diagnose and treat ischemic heart disease. These tests help doctors see how well the heart works and its structure. This helps in making the right diagnosis and treatment plan.
Electrocardiogram (ECG/EKG) Interpretation
An electrocardiogram (ECG or EKG) is a key tool that shows the heart’s electrical activity. It tells us about the heart’s rhythm, rate, and how electricity moves through it. Reading ECG results is vital for spotting ischemic heart disease, as it can show signs of heart damage.
Key ECG findings in IHD include:
- ST-segment changes (elevation or depression)
- T-wave inversion
- Q-waves that show past heart damage
Stress Testing Protocols
Stress tests are important for checking how the heart works under stress. This stress can be from exercise or medicine. They help find out if there’s heart damage and how much, helping decide on treatment.
| Stress Test Type | Description | Indications |
|---|---|---|
| Exercise Stress Test | Patient exercises on a treadmill or stationary bike while ECG and blood pressure are monitored. | Assess for ischemia, evaluate exercise tolerance. |
| Pharmacological Stress Test | Medications (e.g., adenosine, dobutamine) are used to simulate exercise effects on the heart. | Patients unable to perform physical exercise, assess for ischemia. |
Non-invasive Cardiac Imaging
Non-invasive heart imaging gives detailed views of the heart’s structure and function. These include:
- Echocardiography: Uses ultrasound to see heart chambers, valves, and how well they work.
- Cardiac MRI: Gives detailed images of the heart’s structure and function, useful for checking if tissue is alive or scarred.
- Coronary CT Angiography: Shows the coronary arteries and finds blockages or plaque.
Invasive Coronary Angiography: The Gold Standard
Invasive coronary angiography is the top method for finding coronary artery disease. It involves putting dye into the coronary arteries through a catheter. This gives clear X-ray images of the heart’s blood flow.
This procedure is very useful for:
- Confirming coronary artery disease and how bad it is
- Helping decide on treatments like angioplasty and stenting
- Looking at the heart’s blood vessels before surgery
By using these advanced tests, we can accurately diagnose and manage ischemic heart disease. This improves patient care and outcomes.
Treatment Approaches for Ischemic Heart Disease
Managing ischemic heart disease requires a detailed plan. This plan includes lifestyle changes, medicines, and procedures to open blocked arteries. Every patient is different, so we tailor our care to meet their needs.
Lifestyle Modifications
Changing your lifestyle is key in managing ischemic heart disease. Eating a healthy diet, like one full of fruits, veggies, and lean proteins, is important. Also, regular exercise and quitting smoking are essential.
Dietary Changes: Eating less saturated fats, cholesterol, and sodium helps. We suggest foods rich in omega-3s, like fatty fish. Limit processed and sugary foods.
Exercise and Physical Activity: Exercise boosts heart health and overall well-being. Aim for 150 minutes of moderate activity or 75 minutes of vigorous activity weekly. Include muscle-strengthening activities two or more times a week.
Pharmacological Management
Medicines are a big part of treating ischemic heart disease. We use various drugs to control symptoms, slow disease, and prevent complications. These include drugs to prevent blood clots, lower heart rate, widen blood vessels, and lower cholesterol.
- Antiplatelet Agents: Medications like aspirin prevent blood clots.
- Beta-blockers: These drugs reduce the heart’s workload and oxygen demand.
- Nitrates: Nitrates relax blood vessels, improving heart muscle blood flow.
- Statins: Statins lower cholesterol, reducing artery plaque buildup.
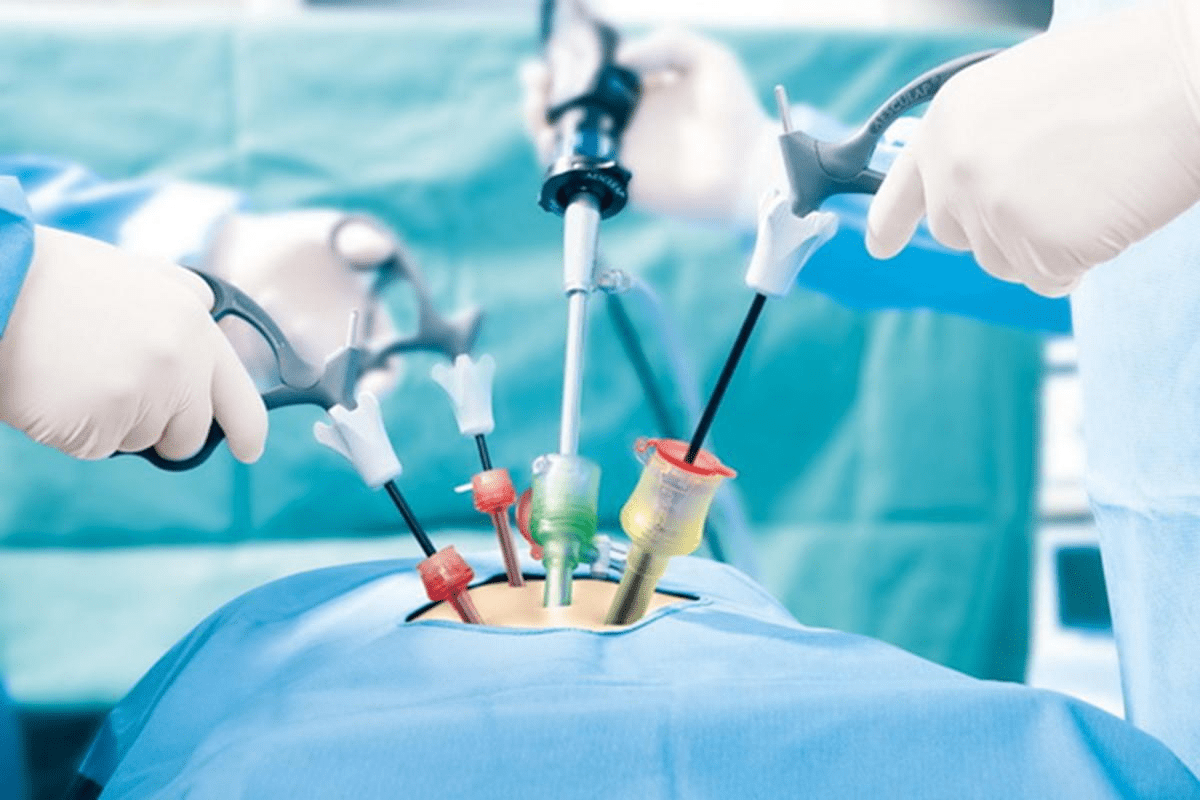
Revascularization Procedures
For some, opening blocked arteries is needed. We consider CABG and PCI, including angioplasty and stenting, to restore blood flow.
Coronary Artery Bypass Grafting (CABG): CABG uses grafts to bypass blocked arteries. This improves blood flow to the heart.
Percutaneous Coronary Intervention (PCI): PCI uses a stent to open blocked arteries. It’s often chosen for specific cases or those at high surgical risk.
By combining lifestyle changes, medicines, and procedures, we create a detailed treatment plan. This plan meets the unique needs of each patient with ischemic heart disease.
Prevention and Early Detection Strategies
We can lower the risk of Ischemic Heart Disease by focusing on prevention and early detection. This is key for those at high risk. Effective strategies include lifestyle changes, medical treatments, and regular check-ups.
Primary Prevention in High-Risk Individuals
Finding people at high risk of Ischemic Heart Disease is important. Risk factors like high blood pressure, diabetes, high cholesterol, and smoking are key. We advise high-risk individuals to follow a heart-healthy lifestyle. This includes eating well, staying active, and quitting smoking.
“The American Heart Association stresses the need for a healthy lifestyle to prevent heart diseases,” experts say.
Screening Recommendations
Regular screenings are key for early detection. Adults over 40 should get regular check-ups. These include blood pressure, lipid, and glucose tests. Screening catches risk before symptoms appear, allowing for early action.
- Blood pressure measurement
- Lipid profiling
- Blood glucose testing
Importance of Regular Check-ups
Regular visits are vital for catching Ischemic Heart Disease early. They let doctors track risk factors and adjust treatments. They also educate patients.
“Regular health check-ups are key for heart health and preventing Ischemic Heart Disease complications,” cardiologists say.
Emerging Technologies in Early Detection
New medical tech is helping us detect Ischemic Heart Disease sooner. Tools like coronary artery calcium scoring and advanced imaging are vital. They help in early diagnosis and risk assessment.
Using these new technologies and following screening guidelines can greatly improve outcomes. It helps those at risk of Ischemic Heart Disease.
Conclusion: Living with and Managing Ischemic Heart Disease
Managing Ischemic Heart Disease (IHD) well is key to a better life and less risk of problems. We’ve covered what IHD is, its risks, how it’s diagnosed, and how it’s treated.
Living with IHD means making big lifestyle changes, getting medical help, and keeping an eye on your health. Working with doctors, you can make a plan that fits you. This plan might include eating right, exercising, and taking your medicines as told.
Handling IHD is a big job that needs constant help and advice. We urge people with IHD to learn as much as they can about their condition. If you notice any symptoms or have worries, see a doctor right away. By being proactive in managing IHD, you can lower your chance of heart problems and get healthier.
FAQ
What is ischemic heart disease (IHD)?
Ischemic heart disease, also known as coronary artery disease, happens when the coronary arteries narrow or block. This reduces blood flow to the heart muscle.
Is IHD the same as coronary artery disease (CAD)?
Yes, IHD and CAD are the same thing. CAD is a more specific term for the disease in the coronary arteries. IHD focuses on how it affects the heart muscle.
What are the risk factors for developing IHD?
Risk factors include things you can change like high blood pressure, high cholesterol, smoking, and diabetes. Non-changeable factors include age, family history, and genetics.
How is IHD diagnosed?
Doctors use a medical history, physical exam, and tests like ECG and stress tests to diagnose IHD. They also use cardiac imaging.
What are the symptoms of IHD?
Symptoms include chest pain, shortness of breath, and fatigue. In severe cases, it can lead to a heart attack. Some people may not show symptoms at all.
Can IHD be prevented?
Yes, you can prevent or delay IHD by managing risk factors. This includes lifestyle changes and medical treatment.
What are the treatment options for IHD?
Treatments include lifestyle changes, medicines, and procedures like angioplasty or bypass surgery.
How can I manage my condition if I have IHD?
Work with your doctor, make lifestyle changes, take your medicines, and go to regular check-ups. This helps manage IHD well.
What is the significance of early detection in IHD?
Early detection means you can get treatment quickly. This can prevent heart attacks and improve outcomes for people with IHD.
Are there emerging technologies for early detection of IHD?
Yes, new imaging and diagnostic technologies are being developed. They aim to improve early detection and management of IHD.
Reference:
- “2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease” – Circulation. https://www.ncbi.nlm.nih.gov/pubmed/37471501/ (professional.heart.org)
- “ESC Guidelines for the management of chronic coronary syndromes” – European Heart Journal. https://academic.oup.com/eurheartj/article/45/36/3415/7743115 (OUP Academic)
- “Ischemic Heart Disease – Cardiovascular Disability” – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK209964/ (NCBI)
“Diagnosis of Stable Ischemic Heart Disease” – American Academy of Family Physicians (AAFP). https://www.aafp.org/pubs/afp/issues/2013/1001/p469.html (aafp.org)