Last Updated on November 27, 2025 by Bilal Hasdemir

At Liv Hospital, we recognize the significance of myocardial infarction (MI), commonly known as a heart attack, as a major threat to heart health. We prioritize trustworthy, patient-centered care to help prevent and treat this life-threatening condition.
Myocardial infarction occurs when the blood flow to the heart is severely blocked, causing damage to the heart muscle. We understand that understanding MI is crucial for both patients and healthcare providers to make informed decisions about heart health.
Key Takeaways
- Myocardial infarction (MI) is commonly known as a heart attack.
- MI occurs when blood flow to the heart is severely blocked.
- Understanding MI is crucial for heart health decisions.
- Liv Hospital provides patient-centered care for MI prevention and treatment.
- Trustworthy care is our priority for international patients.
Understanding MI: The Medical Definition
Myocardial Infarction (MI), commonly referred to as a heart attack, is a serious medical condition that occurs when the blood flow to the heart is blocked, causing damage to the heart muscle. Understanding MI is crucial for grasping the severity of a heart attack and its implications on cardiac health.
The medical definition of MI involves the interruption of blood flow to the heart, leading to tissue death. This interruption can be caused by various factors, including blockages in the coronary arteries.
The Meaning of MI in Cardiology
In cardiology, MI is a significant concern because it directly affects the heart’s ability to function properly. The heart muscle requires a constant supply of oxygen and nutrients, which is compromised during an MI.
Key factors contributing to MI include:
- Atherosclerosis: The buildup of plaque in the arteries.
- Thrombosis: The formation of blood clots that can block arteries.
- Embolism: The obstruction of an artery by an embolus (a foreign object, a blood clot, or another substance).
Myocardial Infarction: Breaking Down the Terminology
To understand MI fully, it’s essential to break down the terminology. “Myocardial” refers to the heart muscle, while “infarction” denotes the death of tissue due to a lack of blood supply.
The diagnosis of MI involves several tests, including:
- Electrocardiogram (ECG) to measure the heart’s electrical activity.
- Blood tests to detect cardiac biomarkers.
- Imaging tests like echocardiography or coronary angiography.
Understanding these terms and diagnostic methods is vital for healthcare professionals to provide appropriate care and for patients to comprehend their condition.
What Is MI in Medical Terms: A Comprehensive Explanation
The term MI, or Myocardial Infarction, refers to the damage and death of heart muscle cells due to a lack of blood supply. This condition is commonly known as a heart attack and occurs when the flow of blood to the heart is blocked, causing tissue damage.
“Myocardial Infarction is a serious medical condition characterized by the interruption of blood flow to the heart, leading to tissue damage,” as defined by medical professionals worldwide.
Defining Myocardial Infarction in Clinical Context
In clinical practice, Myocardial Infarction is diagnosed based on symptoms, electrocardiogram (ECG) changes, and elevated cardiac biomarkers. Understanding MI in this context is crucial for healthcare providers to administer appropriate treatment promptly.
How MI Differs from Other Cardiac Conditions
MI is distinct from other cardiac conditions such as angina or cardiac arrest. While angina is characterized by temporary reduction in blood flow to the heart, MI involves actual damage to the heart muscle. Acute MI can present as STEMI or NSTEMI based on the ECG pattern, further classifying the condition.
AMI Disease: Acute Myocardial Infarction
Acute Myocardial Infarction (AMI) is a medical emergency requiring immediate attention. The term AMI is often used interchangeably with MI, emphasizing the sudden onset of the condition. Prompt treatment, including medications and interventions like angioplasty, is critical to minimize damage.
As medical professionals, we emphasize that understanding the nuances of MI and its various presentations is key to providing optimal care for patients. By recognizing the signs and symptoms early, we can significantly improve outcomes.
The Pathophysiology of Myocardial Infarction
The pathophysiology of myocardial infarction involves a complex interplay of factors leading to heart muscle damage. Myocardial infarction, commonly known as a heart attack, occurs when the flow of blood to a part of the heart is blocked for a long enough time that part of the heart muscle is damaged or dies.
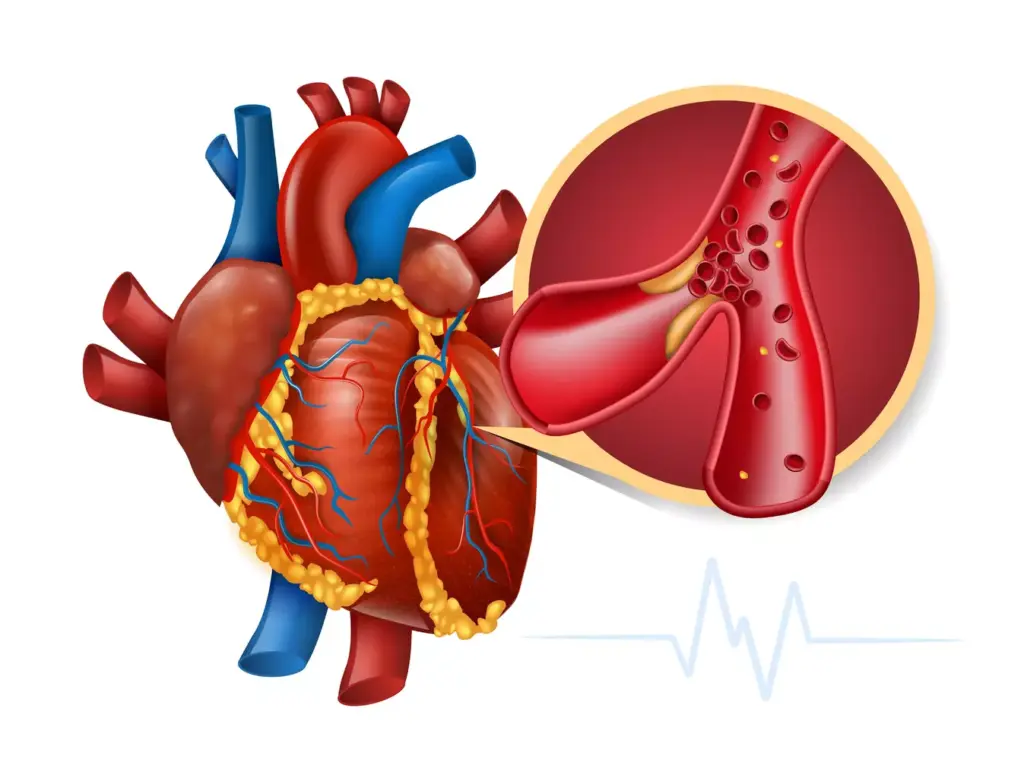
Coronary Artery Blockage: The Primary Cause
The primary cause of myocardial infarction is the blockage of a coronary artery. Coronary arteries supply blood to the heart muscle, and when one of these arteries is blocked, the heart muscle downstream from the blockage becomes damaged due to lack of oxygen and nutrients.
The Process of Heart Muscle Damage
The process of heart muscle damage during a myocardial infarction is multifaceted. Initially, the blockage of a coronary artery leads to a reduction in blood flow, causing ischemia. If the blockage persists, it results in infarction, where the heart muscle cells die due to prolonged lack of oxygen.
| Stage | Description | Time Frame |
|---|---|---|
| Ischemia | Reduced blood flow to the heart muscle | 0-30 minutes |
| Injury | Damage to the heart muscle cells | 30 minutes-2 hours |
| Infarction | Death of heart muscle cells | 2-6 hours |
Cellular Changes During an MI
During a myocardial infarction, significant cellular changes occur. The lack of oxygen and nutrients leads to cellular injury and eventually cell death. This results in an inflammatory response as the body attempts to repair the damaged tissue.
Understanding these cellular changes is crucial for developing effective treatments for myocardial infarction. By targeting the underlying pathophysiological processes, healthcare providers can improve outcomes for patients suffering from this condition.
Types of Myocardial Infarction
The diverse nature of Myocardial Infarction necessitates a nuanced understanding of its different types. Myocardial Infarction (MI) can be classified based on electrocardiogram (ECG) patterns, clinical presentation, and other factors. This classification is crucial for determining the appropriate treatment strategy and predicting patient outcomes.
STEMI: ST-Elevation Myocardial Infarction
ST-Elevation Myocardial Infarction, commonly referred to as STEMI, is a type of MI characterized by a complete blockage of a coronary artery. This blockage results in significant damage to the heart muscle due to prolonged lack of blood flow. On an ECG, STEMI is identified by ST-segment elevation, indicating the area of the heart affected by the blockage. Prompt medical intervention is critical in STEMI cases to minimize heart damage.
NSTEMI: Non-ST-Elevation Myocardial Infarction
Non-ST-Elevation Myocardial Infarction, or NSTEMI, occurs when there is a partial blockage of a coronary artery. Unlike STEMI, NSTEMI does not show ST-segment elevation on an ECG. Instead, it may be diagnosed through other ECG changes or elevated cardiac biomarkers. NSTEMI patients often present with chest pain or other symptoms similar to STEMI but require different management strategies.
Other Classification Systems
Apart from the STEMI and NSTEMI classification, MI can also be categorized based on the underlying cause, such as spontaneous MI or MI secondary to another medical condition. Additionally, MI can be classified into different types based on the presence of certain biomarkers or the location of the infarct. Understanding these different classification systems helps in tailoring treatment to the individual patient’s needs.
We recognize that the classification of Myocardial Infarction is not limited to STEMI and NSTEMI. Other types, such as Type 2 MI, which occurs in the context of ischemia due to either increased oxygen demand or decreased supply, are also important. The complexity of MI classification underscores the need for a comprehensive approach to diagnosis and treatment.
Myocardial Infarction Zones: Understanding the Affected Areas
Understanding the different zones affected by myocardial infarction is crucial for effective treatment and management. When a myocardial infarction occurs, it doesn’t just damage a single area; rather, it creates multiple zones of impact within the heart.
Zone of Necrosis: The Infarct Core
The zone of necrosis, also known as the infarct core, is the area of the heart muscle that has died due to the lack of blood supply. This region is irreversibly damaged and is the central area of the infarct.
The extent of the necrotic zone can vary depending on several factors, including the duration of the occlusion, the presence of collateral circulation, and the metabolic demands of the myocardium.
Zone of Injury: The Surrounding Tissue
Surrounding the zone of necrosis is the zone of injury. This area consists of damaged myocardial cells that are at risk of progressing to necrosis if the ischemia persists. The zone of injury is potentially salvageable with prompt and appropriate treatment.
Timely intervention, such as reperfusion therapy, can help mitigate the damage in this zone, potentially improving patient outcomes.
Zone of Ischemia: The Outer Region
The outermost region is the zone of ischemia, where the myocardial cells are ischemic but still viable. This zone is characterized by reduced blood flow, but the cells have not yet undergone irreversible damage.
Effective management of myocardial infarction involves not only treating the infarct itself but also addressing the surrounding zones to prevent further damage.
Let’s examine the characteristics of these zones in a comparative format:
| Zone | Characteristics | Potential Outcome |
|---|---|---|
| Zone of Necrosis | Irreversible damage, cell death | Permanent damage |
| Zone of Injury | Damaged cells, potentially salvageable | Salvageable with timely treatment |
| Zone of Ischemia | Ischemic but viable cells | Reversible with appropriate management |
As noted by a leading cardiologist, “The concept of myocardial infarction zones highlights the complexity of heart attack damage and underscores the importance of timely and targeted interventions.”
“The goal of MI management is not just to treat the infarct but to preserve the surrounding myocardium.”
We understand that managing myocardial infarction effectively requires a comprehensive approach that considers the different zones affected by the condition.
Signs and Symptoms of MI
Recognizing the signs and symptoms of myocardial infarction is crucial for timely medical intervention. Myocardial infarction, commonly referred to as a heart attack, occurs when the blood flow to the heart is severely blocked, causing damage to the heart muscle.
Classic Symptoms of a Heart Attack
The classic symptoms of a heart attack include chest pain or discomfort, often described as a feeling of pressure, tightness, or heaviness in the chest. This pain can radiate to the arms, back, neck, jaw, or stomach. Other common symptoms include shortness of breath, cold sweats, nausea, and lightheadedness.
Atypical Presentations
Not everyone experiences the classic symptoms of a heart attack. Some individuals may have atypical presentations, which can include fatigue, dizziness, or palpitations. Women, in particular, are more likely to experience atypical symptoms such as shortness of breath, nausea, or back and jaw pain.
Silent Myocardial Infarctions
In some cases, myocardial infarctions can occur without noticeable symptoms, known as silent myocardial infarctions. These events are often discovered during later medical examinations or tests for unrelated conditions. Diabetes and older age are risk factors associated with silent MIs.
Understanding the range of possible symptoms is vital for both patients and healthcare providers to recognize and respond to myocardial infarctions effectively. Prompt medical attention can significantly improve outcomes and reduce the risk of complications.
Diagnosing Myocardial Infarction
To diagnose myocardial infarction (MI), we rely on a combination of electrocardiogram (ECG) findings, cardiac biomarkers, and imaging studies. These diagnostic tools help healthcare professionals confirm the presence of MI and guide appropriate treatment.
Electrocardiogram (ECG) Findings
An electrocardiogram (ECG) is a crucial initial diagnostic tool for MI. It records the electrical activity of the heart, providing insights into the heart’s rhythm and potential areas of damage. Key ECG findings indicative of MI include ST-segment elevation, ST-segment depression, and Q-waves.
ECG Findings in MI:
| ECG Finding | Description | Clinical Significance |
|---|---|---|
| ST-Segment Elevation | Elevation of the ST segment above the baseline | Indicative of STEMI, a type of MI where a major coronary artery is occluded |
| ST-Segment Depression | Depression of the ST segment below the baseline | May indicate ischemia or NSTEMI, suggesting partial occlusion of a coronary artery |
| Q-Waves | Deep, wide Q-waves on the ECG | Often signify a previous MI, indicating areas of scarred heart muscle |
Cardiac Biomarkers
Cardiac biomarkers are proteins released into the bloodstream when heart muscle is damaged. Troponin T and troponin I are highly specific biomarkers for myocardial damage. Elevated levels of these biomarkers are a key indicator of MI.
Imaging Studies
Imaging studies, such as echocardiography and cardiac MRI, provide additional information about the heart’s structure and function. These tests can help identify areas of damaged heart muscle and assess the heart’s overall function.
By combining ECG findings, cardiac biomarkers, and imaging studies, we can accurately diagnose MI and develop an effective treatment plan.
Risk Factors for Developing MI
The risk of developing myocardial infarction (MI) is influenced by a combination of modifiable and non-modifiable factors. Understanding these risk factors is crucial for prevention and management.
Modifiable Risk Factors
Modifiable risk factors are those that can be changed or controlled through lifestyle modifications or medical interventions. Key modifiable risk factors for MI include:
- Hypertension: High blood pressure is a significant risk factor for MI, as it can cause damage to the coronary arteries.
- Diabetes: Diabetes mellitus increases the risk of MI due to its effects on blood vessels and nerves.
- Smoking: Smoking is a major risk factor for MI, as it damages the lining of the coronary arteries and reduces blood flow to the heart.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque buildup in the coronary arteries, increasing the risk of MI.
- Obesity and Physical Inactivity: Being overweight and leading a sedentary lifestyle contribute to the development of other risk factors, such as hypertension and diabetes.
Non-Modifiable Risk Factors
Non-modifiable risk factors are those that cannot be changed. These include:
- Age: The risk of MI increases with age, particularly after the age of 45 for men and 55 for women.
- Family History: A family history of early heart disease is a significant risk factor for MI.
- Genetic Predisposition: Certain genetic conditions can increase the risk of developing MI.
- Gender: Men are generally at higher risk of MI than women, especially at younger ages.
Managing modifiable risk factors is crucial for preventing MI. By understanding and addressing these factors, individuals can significantly reduce their risk of experiencing a myocardial infarction.
The History and Epidemiology of MI
The history of myocardial infarction (MI) is a complex narrative that spans centuries, reflecting our evolving understanding of this critical cardiac condition. As we explore this topic, we will examine the historical context, global impact, and statistical data related to MI, highlighting its significance as a leading cause of morbidity and mortality worldwide.
Historical Understanding of Heart Attacks
The concept of MI has undergone significant transformations since its initial recognition. Early descriptions of heart attacks date back to the late 19th and early 20th centuries, when physicians began to correlate clinical symptoms with post-mortem findings of coronary artery occlusion and myocardial damage.
Over the years, our understanding of MI has evolved, influenced by advances in diagnostic techniques, such as electrocardiography (ECG) and cardiac biomarkers, as well as therapeutic strategies, including thrombolysis and percutaneous coronary intervention (PCI).
Global Impact and Statistics
Myocardial infarction is a major public health concern globally, affecting millions of people each year. According to the World Health Organization (WHO), cardiovascular diseases, including MI, are the leading cause of death worldwide, accounting for over 17.9 million deaths annually.
To better understand the global impact of MI, let’s examine some key statistics:
| Region | MI Incidence Rate (per 100,000) | Mortality Rate (per 100,000) |
|---|---|---|
| Global | 205 | 85 |
| North America | 240 | 70 |
| Europe | 220 | 80 |
| Asia | 180 | 90 |
MI as a Leading Cause of Mortality
The significance of MI as a leading cause of mortality cannot be overstated. Despite advances in treatment and prevention, MI remains a major contributor to cardiovascular mortality worldwide. Understanding the historical context, global impact, and statistical data related to MI is crucial for developing effective strategies to reduce its burden.
As we continue to navigate the complexities of MI, it is clear that a multifaceted approach is necessary to address this critical public health issue. By acknowledging the history and epidemiology of MI, we can better appreciate the challenges that lie ahead and work towards improving cardiovascular health outcomes globally.
Treatment Approaches for Myocardial Infarction
Treating myocardial infarction effectively necessitates a multifaceted approach, including emergency interventions and long-term care. We will explore the various treatment strategies available for managing MI.
Emergency Interventions
Emergency interventions are critical in the management of myocardial infarction. These include thrombolysis and primary percutaneous coronary intervention (PCI), which are aimed at restoring blood flow to the heart muscle.
Thrombolysis involves the administration of clot-busting drugs to dissolve the occluding thrombus, while primary PCI involves the mechanical opening of the blocked artery using angioplasty and stenting.
Medications for MI Management
Medications play a crucial role in the management of myocardial infarction. These include antiplatelet agents, beta-blockers, ACE inhibitors, and statins, which help in reducing morbidity and mortality.
- Antiplatelet agents prevent the formation of new clots.
- Beta-blockers reduce the workload on the heart.
- ACE inhibitors help in managing blood pressure and reducing strain on the heart.
- Statins lower cholesterol levels, reducing the risk of further MI.
Surgical and Catheter-Based Treatments
Surgical and catheter-based treatments are also vital in the management of MI. These include coronary artery bypass grafting (CABG) and PCI.
| Treatment | Description | Indications |
|---|---|---|
| Primary PCI | Mechanical opening of the blocked artery | STEMI, large NSTEMI |
| CABG | Surgical bypass of blocked coronary arteries | Complex coronary disease, failed PCI |
| Thrombolysis | Administration of clot-busting drugs | STEMI, when primary PCI is not available |
These treatments are selected based on the patient’s condition, the severity of the MI, and other clinical factors.
Advances in Cardiac Care and MI Management
Recent years have seen a paradigm shift in the treatment and management of myocardial infarction due to advances in cardiac care. We have witnessed significant improvements in patient outcomes, thanks to the integration of modern technologies, innovative treatment protocols, and a more comprehensive understanding of cardiac health.
Modern Approaches to Reducing Mortality
The reduction of mortality rates in MI patients has been a primary focus of recent advancements. We have seen the introduction of more effective emergency interventions, including the use of advanced cardiac life support systems and rapid transportation to specialized cardiac centers.
One of the key strategies has been the implementation of timely reperfusion therapies, such as thrombolysis and primary percutaneous coronary intervention (PCI). These interventions have been shown to significantly reduce mortality and improve outcomes in patients with acute myocardial infarction.
“The timely application of reperfusion therapies is crucial in reducing mortality and improving outcomes in patients with acute myocardial infarction.”
Multidisciplinary Healthcare Teams
The importance of multidisciplinary healthcare teams cannot be overstated in the management of MI. We bring together cardiologists, emergency medicine specialists, nurses, and other healthcare professionals to provide comprehensive care.
| Team Member | Role in MI Management |
|---|---|
| Cardiologist | Diagnosis, treatment, and long-term management of MI |
| Emergency Medicine Specialist | Initial assessment and stabilization of the patient |
| Nurse | Patient care, education, and support |
Academic Protocols and International Standards
Adherence to academic protocols and international standards is crucial in ensuring that patients receive the best possible care. We follow guidelines set by organizations such as the American Heart Association and the European Society of Cardiology.
These guidelines are based on the latest research and provide a framework for the diagnosis, treatment, and management of MI. By following these protocols, we can ensure that our patients receive evidence-based care that is tailored to their specific needs.
In conclusion, the advances in cardiac care and MI management have significantly improved patient outcomes. We continue to evolve and refine our approaches, ensuring that our patients receive the highest quality care possible.
Conclusion: Living After MI and Future Directions
Understanding what is MI in medical terms is crucial for patients who have experienced a myocardial infarction. Myocardial infarction definition encompasses the damage caused to the heart muscle due to a blockage in the coronary arteries. As we have discussed, timely diagnosis and treatment are vital in managing MI.
Living after MI requires ongoing care and support. At Liv Hospital, we provide advanced cardiac care and comprehensive support for international patients. Our multidisciplinary teams work together to ensure that patients receive the best possible treatment and guidance on managing their condition.
Understanding MI in healthcare is not just about treating the condition; it’s also about providing patients with the necessary tools and resources to lead a healthy life after MI. We are committed to delivering world-class healthcare with complete support for our patients.
As we move forward, future directions in MI management will continue to evolve with advancements in medical technology and treatment protocols. Our focus remains on providing high-quality care and support to patients, ensuring they receive the best possible outcomes.
FAQ
What is MI in medical terms?
MI, or myocardial infarction, is a medical condition where the heart muscle is damaged due to a lack of blood flow, commonly known as a heart attack.
What is the difference between STEMI and NSTEMI?
STEMI (ST-Elevation Myocardial Infarction) and NSTEMI (Non-ST-Elevation Myocardial Infarction) are two types of myocardial infarctions. STEMI is characterized by a complete blockage of a coronary artery, while NSTEMI is a partial blockage.
What are the classic symptoms of a heart attack?
Classic symptoms of a heart attack include chest pain or discomfort, shortness of breath, pain or discomfort in one or both arms, the back, neck, jaw, or stomach, and feeling weak, light-headed, or faint.
What are the risk factors for developing MI?
Risk factors for developing MI include modifiable factors such as high blood pressure, high cholesterol, smoking, and diabetes, as well as non-modifiable factors such as age, family history, and genetic predisposition.
How is MI diagnosed?
MI is diagnosed using a combination of electrocardiogram (ECG) findings, cardiac biomarkers, and imaging studies such as echocardiography or angiography.
What are the treatment approaches for MI?
Treatment approaches for MI include emergency interventions such as thrombolysis or primary percutaneous coronary intervention (PCI), medications to manage symptoms and prevent further damage, and surgical or catheter-based treatments to restore blood flow to the heart.
What is the significance of understanding MI zones?
Understanding MI zones, including the zone of necrosis, zone of injury, and zone of ischemia, is crucial for diagnosing and managing MI, as it helps healthcare providers assess the extent of damage to the heart muscle.
How can MI be prevented?
MI can be prevented by managing modifiable risk factors such as high blood pressure, high cholesterol, and smoking, as well as maintaining a healthy lifestyle through regular exercise and a balanced diet.
What is the global impact of MI?
MI is a leading cause of mortality worldwide, with a significant impact on global health and economies. Understanding the epidemiology of MI is crucial for developing effective prevention and treatment strategies.
What are the advances in cardiac care and MI management?
Advances in cardiac care and MI management include modern approaches to reducing mortality, multidisciplinary healthcare teams, and academic protocols and international standards that improve patient outcomes and quality of care.
References:
• National Center for Biotechnology Information. (2023). Myocardial infarction – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK537076/
• Wikipedia. (n.d.). Myocardial infarction – Wikipedia. https://en.wikipedia.org/wiki/Myocardial_infarction
• American Heart Association. (n.d.). What is a heart attack? https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks
• NHS. (n.d.). Heart attack – NHS. https://www.nhs.uk/conditions/heart-attack
• American Heart Association. (2007). Universal definition of myocardial infarction. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.107.187397