Nuclear cardiac imaging is a key tool for checking heart conditions, like blockages. It helps us see how the heartworks and what’s wrong. This makes it easier to diagnose problems.
Did you know heart diseases are a top cause of death globally? Nuclear cardiac imaging is key in finding and treating these issues. Myocardial perfusion imaging and stress tests are important. They help spot blockages and plan treatments.
In this article, we’ll look at the ways nuclear cardiac imaging works. We’ll see how it helps with heart disease and what patients can expect during these tests.
Key Takeaways
- Nuclear cardiac imaging is essential for diagnosing heart conditions.
- Myocardial perfusion imaging is a key diagnostic tool.
- Stress tests help identify possible blockages.
- Nuclear cardiac imaging aids in developing effective treatment plans.
- Understanding these tests can help patients feel more prepared.
Understanding Nuclear Cardiac Imaging
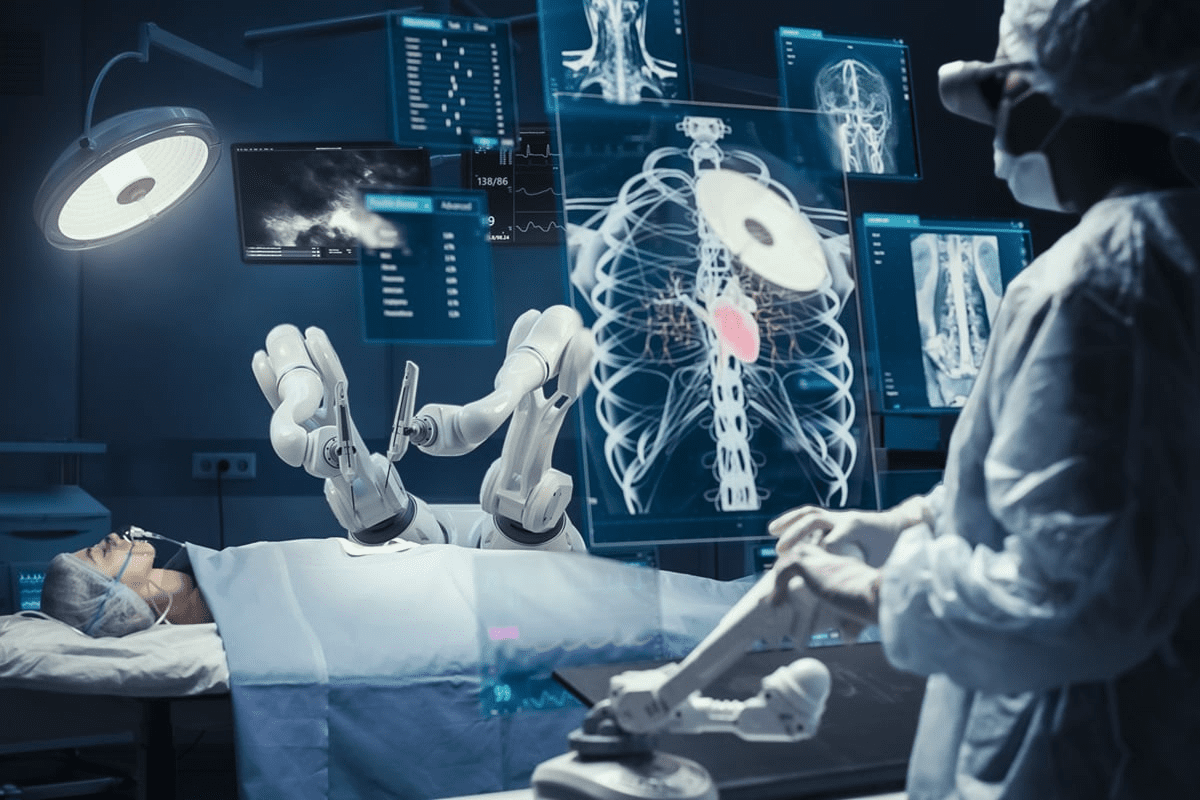
Nuclear cardiac imaging is a key tool in heart health. It lets doctors see the heart’s inner workings without surgery. This method helps doctors find and treat heart problems better.
Definition and Basic Principles
This imaging uses tiny amounts of radioactive tracers. These tracers stick to the heart muscle. This shows doctors where blood flow is low or where the heart might be damaged.
The idea is simple. The tracers light up where blood flows. Cameras then make pictures of the heart’s health based on this light.
Role in Cardiovascular Diagnostics
Nuclear cardiac imaging is vital for heart disease diagnosis. It’s great for checking blood flow, finding blockages, and seeing if heart tissue is alive.
It gives doctors a clear view of the heart. This helps them:
- Spot and measure heart blockages
- See if treatments are working
- Find damaged heart areas
Historical Development of Nuclear Cardiac Imaging
The first heart scans using tracers were in the 1970s. Over time, technology has made these scans much better.
Now, with SPECT and PET, doctors can see the heart in even more detail. This has led to better care and results for patients.
How Nuclear Cardiac Imaging Works
To understand nuclear cardiac imaging, we need to look at its core technologies. It uses radioactive tracers, advanced cameras, and computers to show the heart’s details.
Radioactive Tracers and Their Function
Radioactive tracers emit radiation that the imaging system picks up. These tracers target heart functions like blood flow and muscle activity. For example, Technetium-99m (Tc-99m) sestamibi or Tetrofosmin show how well the heart muscle gets blood.
The right tracer depends on what we want to see. Tc-99m tracers are often used to check if heart muscle is alive and getting enough blood.
Gamma Camera Technology
A gamma camera is key in nuclear cardiac imaging. It catches the radiation from the tracers in the heart. The camera moves around the patient, taking pictures from different sides. These pictures help make a 3D image of the heart.
Today’s gamma cameras have better detectors and collimators. This means clearer images and faster scans. Some also use SPECT technology for even more detailed heart images.
Computer Processing and Image Reconstruction
The gamma camera’s raw data is processed by computers. These algorithms fix issues like image distortion and improve picture quality.
The final images show how well the heart is working. They help us see blood flow, muscle movement, and how much blood the heart pumps out. Software tools help us measure these things and understand heart disease better.
| Component | Function | Clinical Significance |
| Radioactive Tracers | Emit radiation detected by imaging systems | Assess myocardial perfusion and viability |
| Gamma Camera | Detects gamma radiation from tracers | Captures images of heart function from multiple angles |
| Computer Processing | Reconstructs images from raw data | Provides detailed images of cardiac structure and function |
Nuclear cardiac imaging is a powerful tool for heart disease diagnosis and management. We keep improving these technologies to better help patients.
Myocardial Perfusion Imaging (MPI)
Myocardial Perfusion Imaging (MPI) is a key tool for checking heart function and finding coronary artery disease. It helps see how well the heart’s blood flows and spots problems.
Single-Photon Emission Computed Tomography (SPECT)
Single-Photon Emission Computed Tomography (SPECT) is a main method in MPI. It uses a gamma camera to track radioactive tracers in the heart. This helps find where blood flow is low.
SPECT gives doctors important info on the heart’s work. It helps find coronary artery disease and predict heart risks. It’s a key part of nuclear cardiology because it makes clear heart images.
Common Radiopharmaceuticals Used in MPI
Several radiopharmaceuticals are used in MPI, with Tc-99m sestamibi and Tl-201 thallium being top choices. These agents show where blood flow is low in the heart. The right one depends on the patient’s needs and condition.
- Tc-99m sestamibi: Known for its high image quality and favorable physical characteristics for gamma camera imaging.
- Tl-201 thallium: Often used for assessing myocardial viability due to its ability to redistribute into ischemic but viable myocardium.
Clinical Applications of MPI
MPI is used in many ways, like finding coronary artery disease and checking if treatments work. It’s great for:
- Finding patients at high risk of heart problems.
- Seeing how much ischemia there is and deciding on treatments.
- Checking if heart treatments are working and if the disease is getting worse.
MPI gives detailed info on heart blood flow and function. This helps doctors make better choices for their patients. It leads to better care for those with heart disease.
Nuclear Stress Testing: A Primary Heart Test for Blockage
We use nuclear stress testing to see how the heart works under stress. It helps us find blockages. This test is key for checking coronary artery disease and finding the right treatment.
Exercise Stress Testing Protocol
Exercise stress testing checks the heart’s function when active. Patients usually walk on a treadmill or bike while we watch their heart rate and blood pressure. We increase the exercise to stress the heart and see how it works.
The test happens in a place where doctors can watch closely. They can quickly help if there’s a problem. We aim to get the heart rate up to a certain level, based on age and fitness.
Pharmacological Stress Testing Options
For those who can’t do exercise testing, we have pharmacological stress testing. This uses medicine to make the heart work like it would with exercise, without needing to move much.
We use adenosine, regadenoson, or dobutamine for this test. The right medicine depends on the patient’s health and history. Our team picks the best one for accurate results.
“Pharmacological stress testing has become an indispensable tool in our diagnostic arsenal, providing a reliable option for those who can’t do traditional exercise testing.”
” A Cardiologist
Interpreting Nuclear Stress Test Results
Understanding nuclear stress test results takes skill and knowledge of the heart. Our team looks at the images to find any problems with blood flow. The results show if there are blockages or other heart issues, helping us decide on treatment.
A normal test means the heart is okay under stress. But an abnormal test might show blockages or other heart problems. Based on the results, we might suggest more tests or treatment. We work with patients to create a plan that meets their needs.
Positron Emission Tomography (PET) in Cardiac Imaging
PET scans are key in cardiology, showing how well the heart works and its structure. We use PET imaging to get detailed views of the heart’s function and structure.
PET Radiopharmaceuticals for Cardiac Studies
PET radiopharmaceuticals are essential in heart imaging. We use tracers like Rubidium-82 and Nitrogen-13 ammonia to see how blood flows to the heart muscle. These tracers help spot areas where blood flow is low.
The right PET radiopharmaceutical depends on the question we’re trying to answer and what’s available. Nitrogen-13 ammonia is great for checking blood flow because it’s absorbed well by the heart.
Advantages of Cardiac PET over SPECT
Cardiac PET has big advantages over SPECT. It offers better detail and more accurate corrections for body parts in the way, making it more accurate for diagnosis.
PET also lets us measure blood flow and how well the heart handles stress. This is key for figuring out how serious heart disease is and how to treat it.
Clinical Applications of Cardiac PET
PET has many uses in cardiology. We use it to find heart disease, see if heart tissue can recover, and check if treatments work.
PET is also great for seeing who might need heart surgery. It helps us know if fixing blocked arteries will help the heart work better.
In summary, cardiac PET is a powerful tool for managing heart disease. It helps us understand and treat heart problems better.
Gated Blood Pool Imaging (MUGA Scan)

Gated Blood Pool Imaging, also known as MUGA scan, is a way to check how well the heart works. It uses a special test to see how the heart’s ventricles function. This is very helpful in checking for heart damage from some treatments.
Procedure and Technique
The MUGA scan uses a tiny bit of radioactive tracer to see the heart’s blood. It matches the heart’s rhythm with the patient’s ECG. This lets doctors check the heart’s function at different times in its cycle.
The test is done in a special room with a gamma camera. The camera takes pictures of the heart. Then, a computer turns these pictures into moving images of the heart’s work.
Evaluation of Ventricular Function
The MUGA scan is great for checking how well the heart’s ventricles work. It gives a precise measure of the left ventricle’s ejection fraction (LVEF). This is key to knowing how well the heart pumps blood.
| Parameter | Description | Normal Value |
| LVEF | Left Ventricular Ejection Fraction | 55-70% |
| RVEF | Right Ventricular Ejection Fraction | 40-60% |
Applications in Cardiotoxicity Monitoring
The MUGA scan is also key in watching patients who might get heart damage from treatments. It helps doctors see if the heart is getting damaged early on. This way, they can change the treatment to keep the heart safe.
“The use of MUGA scan in monitoring cardiotoxicity has become a standard practice in oncology, allowing for the safe administration of potentially cardiotoxic therapies.”
Nuclear Medicine Review
By using MUGA scans often, doctors can make sure treatments are safe for the heart. This helps keep patients healthy and safe.
Cardiac Sarcoid and Amyloid Imaging
Diagnosing cardiac sarcoid and amyloid uses advanced imaging, with nuclear medicine key. These conditions harm the heart’s structure and function. They can lead to serious problems if not caught and treated early.
FDG PET for Cardiac Sarcoidosis
Fluorodeoxyglucose Positron Emission Tomography (FDG PET) is a key tool for cardiac sarcoidosis. This condition causes granulomatous tissue to invade the heart. It can lead to heart failure or arrhythmias. FDG PET spots active inflammation in the heart, helping diagnose and treat early.
To prepare for FDG PET, you must follow dietary rules. This makes inflamed areas stand out. It’s great for seeing how much disease is present and how well treatment is working.
Pyrophosphate Imaging for Cardiac Amyloidosis
Pyrophosphate imaging, with Technetium-99m pyrophosphate (Tc-PYP), is key for cardiac amyloidosis, like ATTR. It’s very good at finding amyloid in the heart.
Pyrophosphate imaging helps diagnose cardiac amyloidosis and tell it apart from other heart diseases. It’s also useful for figuring out how much amyloid is in the heart. This helps doctors decide on the best treatment.
Clinical Impact and Patient Management
Accurate diagnosis of cardiac sarcoidosis and amyloidosis with nuclear imaging greatly impacts patient care. It leads to more effective treatments, improving patient outcomes. For cardiac sarcoidosis, early use of FDG PET means starting treatment sooner. This can prevent lasting damage.
For cardiac amyloidosis, pyrophosphate imaging helps choose the right treatments for ATTR amyloidosis. This includes medicines that stabilize transthyretin or gene silencers. Knowing the exact diagnosis and how much disease is present lets doctors track treatment success. They can then adjust treatment plans as needed.
Hybrid Imaging Techniques
Hybrid imaging techniques have changed how we diagnose heart problems. They mix different imaging methods to understand heart health better.
SPECT/CT Systems
SPECT/CT systems combine SPECT’s function info with CT’s anatomy. This mix boosts accuracy by pinpointing SPECT findings better.
Key Benefits of SPECT/CT:
- Improved diagnostic accuracy
- Better localization of abnormalities
- Enhanced assessment of cardiac function and anatomy
PET/CT in Cardiac Applications
PET/CT merges PET’s metabolic info with CT’s anatomy. It’s great for checking heart viability and finding coronary artery disease.
Experts say, “The mix of PET and CT has greatly helped in diagnosing and treating heart diseases.”
“PET/CT has emerged as a powerful tool in cardiac imaging, giving insights into both the heart’s anatomy and function.
| Modality | Clinical Application | Benefits |
| PET/CT | Myocardial viability assessment | Accurate detection of viable myocardium |
| PET/CT | Coronary artery disease detection | Enhanced sensitivity and specificity |
PET/MRI: Emerging Applications
PET/MRI is a new hybrid modality. It combines PET’s metabolic info with MRI’s soft tissue detail. It’s promising for checking cardiac sarcoidosis and amyloidosis.
Potential applications of PET/MRI include:
- Comprehensive assessment of cardiac inflammation
- Detailed evaluation of cardiac structure and function
- Monitoring of disease progression and response to treatment
Radiation Safety and Considerations
Nuclear cardiac imaging uses small amounts of radioactive tracers to diagnose heart disease. This method is effective but involves exposure to ionizing radiation. It’s important to talk about radiation safety in this context.
Patients might worry about radiation exposure. But, it’s key to balance the benefits of these tests against the risks. These tests help diagnose coronary artery disease and guide treatment.
Typical Radiation Doses in Nuclear Cardiac Imaging
The radiation dose from these tests varies. For example, a myocardial perfusion imaging study might have a dose of 9-12 mSv. This is higher than the average annual background radiation of 3.1 mSv.
These doses are higher, but they provide important diagnostic information. This information is not available through other means.
Risk-Benefit Analysis
When thinking about nuclear cardiac imaging, a risk-benefit analysis is essential. The benefits of accurate diagnosis often outweigh the risks of radiation exposure. For many, this information can be lifesaving.
There is a small risk of cancer from radiation exposure. But, this risk is small compared to the benefits of the diagnostic information. Studies estimate the lifetime risk of cancer from these procedures.
- The benefits of nuclear cardiac imaging include accurate diagnosis of coronary artery disease.
- Guidance for appropriate treatment decisions based on imaging results.
- Potential for improved patient outcomes through early and accurate diagnosis.
Strategies to Minimize Radiation Exposure
We are committed to reducing radiation exposure. Several strategies help achieve this goal:
- Use of lower dose protocols: Advances in technology and protocol optimization allow for reduced doses without losing diagnostic accuracy.
- Selection of appropriate radiopharmaceuticals: Choosing radiopharmaceuticals with lower doses or those that allow for lower administered activities.
- Alternative imaging techniques: Considering alternative imaging modalities that do not involve ionizing radiation, such as echocardiography or cardiac MRI, when appropriate.
By using these strategies, we can reduce radiation exposure. This way, we maintain the high-quality diagnostic information healthcare providers rely on.
Comparing Nuclear Imaging to Other Cardiac Diagnostic Methods
It’s key to know how different heart imaging methods work. We look at nuclear imaging alongside other important tests like coronary angiography and echocardiography. This helps in making the right diagnosis and treatment plan.
Coronary Angiography and Cardiac Catheterization
Coronary angiography shows the heart’s arteries in detail. It’s done during cardiac catheterization. A catheter injects dye into the arteries. This method gives clear pictures of the arteries but doesn’t check blood flow or heart health.
Nuclear imaging, like myocardial perfusion imaging (MPI), shows how well the heart gets blood. It spots areas where the heart might not get enough blood. This info helps with what coronary angiography can’t show.
Coronary CT Angiography
Coronary CT angiography is a non-invasive test. It uses CT scans to see the heart’s arteries. It’s good for people at low to moderate risk of heart disease. But, it doesn’t give the detailed blood flow info that nuclear imaging does.
- Coronary CT angiography is less invasive than traditional coronary angiography.
- It gives clear images of the heart’s arteries.
- It’s great for checking if there’s big heart disease.
Echocardiography and Stress Echocardiography
Echocardiography uses sound waves to see the heart. It’s a non-invasive way to check the heart’s shape and how it works. Stress echocardiography checks how the heart does under stress.
Echocardiography is good for looking at the heart’s structure and function. But, nuclear imaging gives more detailed info on blood flow and heart health.
Cardiac MRI
Cardiac MRI (CMR) gives detailed heart images without radiation. CMR can see how well the heart works, find scar tissue, and check function. It’s best for complex heart issues or when other tests don’t help.
Looking at these heart tests, each has its own strengths and weaknesses. The right test depends on the patient’s condition, what the doctor needs to know, and what’s available.
Knowing what each heart imaging method can do helps doctors make better choices. This leads to better care for patients.
Advancements and Future Directions in Nuclear Cardiac Imaging
New discoveries in radiopharmaceuticals and imaging tech are changing nuclear cardiac imaging. We’re exploring new areas that could be very important.
New Radiopharmaceuticals Under Development
New radiopharmaceuticals are key for better nuclear cardiac imaging. They aim to be more precise, giving clearer images and accurate diagnoses. Researchers are working on tracers that can better see heart health and detect inflammation.
Some exciting new radiopharmaceuticals include:
- Fluorine-18 labeled compounds: These have a longer half-life and lower positron energy, improving imaging.
- Novel myocardial perfusion agents: They help better see blood flow to the heart muscle.
- Inflammation-targeting tracers: These can spot and track heart inflammation.
| Radiopharmaceutical | Application | Advantages |
| Fluorine-18 Flurpiridaz | Myocardial Perfusion Imaging | Improved image quality, better diagnostic accuracy |
| 68Ga-DOTATATE | Cardiac Sarcoidosis Imaging | High sensitivity for detecting cardiac sarcoidosis |
Technological Innovations in Imaging Equipment
New tech in imaging equipment is also vital for nuclear cardiac imaging. Modern gamma cameras and PET scanners have better resolution and faster speeds. They also do a better job of quantifying images.
A recent study said, “Advances in detector tech and image algorithms have greatly improved nuclear cardiac imaging.”
“The use of advanced tech like cadmium-zinc-telluride (CZT) detectors has changed the game. It makes imaging faster and more accurate.”
Journal of Nuclear Cardiology
Artificial Intelligence Applications
Artificial intelligence (AI) is being used more in nuclear cardiac imaging. It helps analyze images and improve diagnosis accuracy. AI can also predict patient outcomes.
AI’s main uses in nuclear cardiac imaging are:
- Automated image analysis: AI helps measure perfusion defects and heart function.
- Predictive modeling: AI predicts patient risk based on imaging and clinical data.
- Image enhancement: AI improves image quality with advanced techniques.
As we keep adding these advancements to our work, nuclear cardiac imaging will get even better. It will help us diagnose and manage heart disease more effectively.
Conclusion
Nuclear cardiac imaging has changed how we diagnose heart problems. It offers many ways to find heart issues and blockages. We’ve looked at methods like myocardial perfusion imaging and positron emission tomography. Each one gives us different views of the heart’s function.
It’s important to pick the right test for each patient. Knowing the good and bad of each imaging method helps doctors. This way, they can give care that fits each person’s needs.
We’re always working to make nuclear cardiac imaging better. Our goal is to provide top-notch healthcare. We use the newest diagnostic tools to help patients and improve heart care.
FAQ
What is nuclear cardiac imaging, and how does it help diagnose heart conditions?
Nuclear cardiac imaging uses tiny amounts of radioactive tracers. It helps see the heart and its blood flow. This tool is key in finding heart problems like blockages by showing the heart’s structure and how it works.
What is the difference between a nuclear stress test and a regular stress test?
A nuclear stress test uses a radioactive tracer to see the heart’s blood flow during exercise. A regular stress test only checks the heart’s electrical activity and blood pressure during exercise.
What is myocardial perfusion imaging (MPI), and how is it used in diagnosing coronary artery disease?
MPI is a nuclear imaging type that checks the heart’s blood flow at rest and stress. It spots areas with less blood flow, showing blockages or damage in coronary artery disease.
What are the benefits of using Positron Emission Tomography (PET) in cardiac imaging?
PET gives detailed images of the heart’s structure and function. It’s very accurate, helps see if heart tissue is alive, and finds coronary artery disease better.
How does gated blood pool imaging (MUGA scan) evaluate ventricular function?
The MUGA scan uses a radioactive tracer to see the heart’s ventricles. It checks how well they work by measuring the ejection fraction, which is the blood pumped out with each heartbeat.
What is the role of hybrid imaging techniques, such as SPECT/CT and PET/CT, in cardiac imaging?
Hybrid imaging combines different types, like SPECT or PET with CT. It gives both functional and anatomical info. This makes diagnosis more accurate and helps in treatment planning.
How can radiation exposure be minimized during nuclear cardiac imaging?
To lower radiation, use the least amount of tracer needed. Optimize imaging and use technologies that reduce dose.
How does nuclear cardiac imaging compare to other cardiac diagnostic methods, such as coronary angiography and cardiac MRI?
Nuclear imaging shows the heart’s blood flow and viability. Coronary angiography shows the heart’s structure. Cardiac MRI gives detailed structural and functional info. The right choice depends on the question and patient needs.
What are the future directions in nuclear cardiac imaging, and how will they impact patient care?
New radiopharmaceuticals and technologies will improve nuclear cardiac imaging. Emerging uses, like artificial intelligence, will also enhance patient care.