
Do you worry about sudden heart palpitations or chest fluttering? We get it. Feeling scared and unsure about irregular heartbeats is normal. Paroxysmal atrial flutter is a heart rhythm problem. It causes rapid, regular heartbeats in the upper chambers of the heart. These episodes can come and go without warning.
At Liv Hospital, we’re here to help. Our team of experts is up-to-date on the latest treatments for this condition. We want to help you understand what causes these episodes and how long they last. Knowing this helps us manage your condition better.
Key Takeaways
- Paroxysmal atrial flutter is a type of supraventricular tachycardia.
- Episodes of atrial flutter can be unpredictable and vary in duration.
- Understanding the causes and risks is key to managing the condition.
- Liv Hospital offers top-notch cardiology care.
- Our expertise helps patients manage their condition and improve their quality of life.
The Nature of Paroxysmal Atrial Flutter
To understand paroxysmal atrial flutter, we need to look at its electrical activity and key features. It’s a type of arrhythmia with a fast, regular heart rhythm. We’ll explore its definition, electrical patterns, and how it differs from other heart rhythm issues.
Definition and Electrical Activity Patterns
Paroxysmal atrial flutter starts and stops suddenly, lasting from minutes to days. It happens when the heart’s upper chambers (atria) have an abnormal electrical circuit. This leads to a fast heartbeat.
The heart’s electrical activity in the atria is regular and rapid, usually between 250 to 300 beats per minute. This condition is marked by a “sawtooth” pattern on an electrocardiogram (ECG). This pattern is due to the re-entrant electrical circuit causing the atria to contract quickly.
Distinguishing Features from Other Arrhythmias
One main difference of paroxysmal atrial flutter is its regular rhythm. Unlike atrial fibrillation, which has an irregular heartbeat. Here are some key differences:
- Regular vs. Irregular Rhythm: Atrial flutter has a regular rhythm, whereas atrial fibrillation is characterized by an irregular heartbeat.
- ECG Pattern: The “sawtooth” pattern on an ECG is typical for atrial flutter, whereas atrial fibrillation shows a more chaotic pattern.
- Heart Rate: Atrial flutter typically has a faster heart rate than atrial fibrillation, though this can vary.
Knowing these differences is key for accurate diagnosis and treatment. By recognizing the unique traits of paroxysmal atrial flutter, doctors can create effective management plans.
Duration and Patterns of Atrial Flutter Episodes
Knowing how long atrial flutter episodes last is key to managing the condition. Atrial flutter makes the heart beat too fast, at 250-300 beats per minute. How long these episodes last can vary a lot from person to person.
Typical Episode Timeframes: Minutes to Days
Atrial flutter episodes can last from a few minutes to several days. The time they last can change a lot, making it hard to guess when or how long they’ll last. Some might stop on their own, but others need medical help.
Factors That Influence Episode Length
Many things can change how long atrial flutter episodes last. These include heart problems, lifestyle, and other health issues. For example, hypertension and obesity can make episodes more frequent and longer. Knowing these factors helps in finding better ways to manage the condition.
Healthcare providers can create better treatment plans by understanding what affects episode length. This might include treating underlying health issues, changing lifestyle habits, and using the right medicines.
Identifying Symptoms During an Atrial Flutter Episode
It’s key to spot the signs of atrial flutter early for quick medical help. Atrial flutter can show different symptoms, from mild to serious.
Common Symptoms: Palpitations and Chest Flutter
People with atrial flutter often feel palpitations. This is a fast or irregular heartbeat in the chest. Some might also notice a chest flutter, which can worry them about their heart.
Other common signs include:
- Irregular heartbeat
- Shortness of breath
- Fatigue
- Lightheadedness
Severe Manifestations: Dizziness and Fainting
In serious cases, atrial flutter can cause dizziness or fainting. These happen when blood pressure drops too low. If you feel these symptoms, get help right away.
Knowing the symptoms of atrial flutter is vital for heart health. If you notice any unusual signs, see a doctor. This way, you can manage your condition better and get the right treatment.
Understanding Paroxysmal Atrial Flutter Mechanisms
It’s key to know how paroxysmal atrial flutter works to manage it well. This condition causes the heart’s upper chambers to beat too fast. This can lead to serious symptoms and health issues if not treated.
The Electrical Circuit Problem
Paroxysmal atrial flutter is mainly caused by an electrical issue in the heart. This issue often comes from a loop of electrical activity. This loop makes the heart beat fast and regularly.
Things like heart disease, high blood pressure, and some medicines can cause this loop. These factors can mess with the heart’s electrical paths.
Heart Rates During Episodes: 250-300 BPM
When someone has paroxysmal atrial flutter, their heart beats very fast. It usually goes from 250 to 300 beats per minute. This fast heart rate can cause symptoms like feeling dizzy, having trouble breathing, and feeling like the heart is skipping beats.
The fast heart rate comes from the abnormal electrical activity in the atria. The heart’s lower chambers also beat fast, but not as quickly as the atria.
| Heart Rate (BPM) | Symptoms | Complications |
|---|---|---|
| 250-300 | Palpitations, dizziness, shortness of breath | Heart failure, stroke, decreased cardiac output |
| < 250 | Mild palpitations, fatigue | Potential for increased risk of thromboembolism |
| > 300 | Severe palpitations, syncope, chest pain | Increased risk of heart failure, severe hemodynamic compromise |
Knowing how these mechanisms affect heart rate is vital. It helps doctors diagnose and treat paroxysmal atrial flutter effectively.
Primary Causes of Atrial Flutter
Atrial flutter can be caused by heart and non-heart factors. It happens when the heart’s electrical system gets disrupted.
Cardiovascular Conditions
Many heart problems can lead to atrial flutter. These include:
- Coronary Heart Disease: Poor blood flow to the heart muscle can cause electrical issues.
- Heart Failure: When the heart can’t pump well, it may change shape and function, causing atrial flutter.
- Myocardial Infarction: A heart attack can harm the heart’s electrical paths.
- Hypertension: High blood pressure can make the heart muscle thick, raising arrhythmia risk.
Non-Cardiac Contributing Factors
Non-heart factors also play a big role in atrial flutter. These include:
- Lung Diseases: Issues like emphysema and chronic bronchitis can harm heart function and lead to atrial flutter.
- Thyroid Problems: Both too much and too little thyroid hormone can affect heart rhythm.
- Sleep Apnea: This can cause heart stress and rhythm changes due to oxygen level swings.
- Diabetes and Kidney Disease: These can harm the heart through metabolic and fluid balance changes.
Lifestyle choices like binge drinking and obesity can also increase atrial flutter risk. Knowing these causes helps in managing and preventing the condition.
The Connection Between Respiratory Illnesses and Heart Flutter
Respiratory conditions like emphysema can put a lot of strain on the heart. This strain can lead to arrhythmias, such as atrial flutter. We will look into how these conditions affect the heart and contribute to atrial flutter.
Bronchitis and Its Impact on Cardiac Function
Bronchitis, which inflames the bronchial tubes, can harm the heart. When we have bronchitis, our lungs work harder. This makes the heart work even harder, which can cause heart flutter or atrial flutter in some people.
The inflammation from bronchitis can also cause systemic inflammation. This affects the heart’s function. It’s important to consider how respiratory and cardiac health are connected when treating bronchitis.
Emphysema and Chronic Lung Diseases
Emphysema, a type of COPD, can also harm the heart. The damage to the alveoli means less oxygen exchange. This makes the heart work harder, which can strain it and lead to arrhythmias.
Chronic lung diseases, including COPD, increase the risk of atrial fibrillation (AFib) and atrial flutter. The reasons include hypoxia, systemic inflammation, and the heart’s increased workload.
| Respiratory Condition | Impact on Heart Health | Risk of Atrial Flutter |
|---|---|---|
| Bronchitis | Increased strain due to reduced airflow | Moderate |
| Emphysema | Reduced oxygen exchange, increased heart workload | High |
| COPD | Systemic inflammation, hypoxia | High |
It’s key to understand how respiratory illnesses and heart flutter are connected. By recognizing the heart risks of these diseases, we can offer better care to our patients.
Diagnostic Approaches for Paroxysmal Atrial Flutter
We use many tools to find and treat paroxysmal atrial flutter. To diagnose it, we look at the heart’s electrical signals. We also look for the special patterns of atrial flutter.
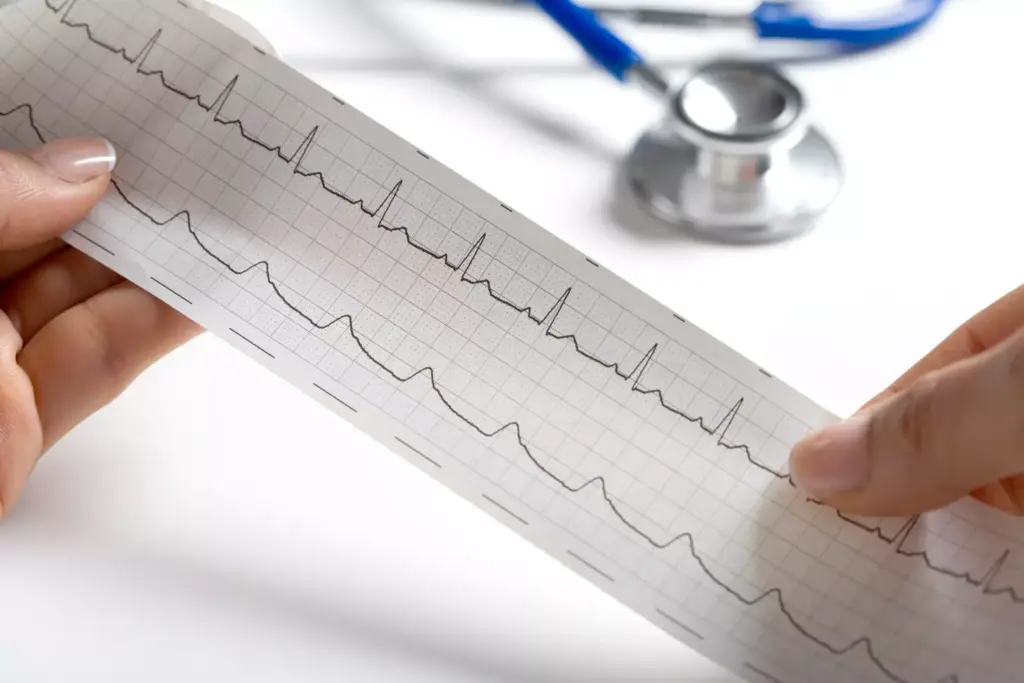
Electrocardiogram and Holter Monitoring
An electrocardiogram (EKG) is key. It records the heart’s electrical signals. It spots the “sawtooth” pattern of atrial flutter. Holter monitoring records the heart for 24 hours. It catches episodes that happen now and then.
Both tests are vital for spotting paroxysmal atrial flutter. They show how it affects the heart.
Advanced Diagnostic Techniques
There are more ways to understand atrial flutter. Advanced diagnostic techniques include:
- Event monitors that track the heart’s rhythm for longer.
- Echocardiograms that show the heart’s shape and how it works.
- Electrophysiology studies that map the heart’s electrical paths.
These methods help confirm the diagnosis. They also guide the treatment plan.
Treatment Strategies for Managing Atrial Flutter
Managing atrial flutter needs a mix of quick and long-term plans. We’ll look at how to handle it, from immediate actions to more serious steps.
Acute Episode Management
When atrial flutter hits, we aim to slow the heart and get it back to normal. We use beta-blockers or special drugs to do this. Sometimes, we need to shock the heart back to rhythm with electrical cardioversion.
Acute Episode Management Strategies:
- Medications to control heart rate
- Anti-arrhythmic drugs to restore normal rhythm
- Electrical cardioversion for immediate rhythm restoration
Long-term Control Methods
For keeping it under control long-term, we prevent future episodes and lessen symptoms. This includes ongoing meds, lifestyle changes, and watching the heart. For those with frequent episodes, catheter ablation is an option.
Long-term Control Strategies:
- Ongoing medication to prevent episodes
- Lifestyle changes to reduce symptoms
- Catheter ablation for recurrent cases
Catheter Ablation and Surgical Options
Catheter ablation is a small procedure that destroys the bad electrical path in the heart. For some, surgery or other treatments might be needed.
| Treatment Option | Description | Benefits |
|---|---|---|
| Catheter Ablation | Minimally invasive procedure to destroy abnormal electrical pathways | High success rate, reduces recurrence |
| Surgical Ablation | Surgical intervention to treat atrial flutter | Effective for complex cases, can be combined with other surgeries |
| Medications | Ongoing drug therapy to control symptoms and prevent episodes | Non-invasive, can be tailored to individual needs |
Every patient is different, so we tailor treatments. By using these methods, we can manage atrial flutter well and improve our patients’ lives.
Comparing Atrial Flutter and Atrial Fibrillation
Atrial flutter and atrial fibrillation are both types of heart rhythm problems. They have different electrical patterns. Knowing these differences is key to treating them well.
Differences in Electrical Patterns
Atrial fibrillation has chaotic atrial activity, with many irregular electrical impulses. On the other hand, atrial flutter shows a more regular pattern. This pattern is often seen as a “sawtooth” or “flutter” wave on an electrocardiogram (ECG).
Here’s a table to show the differences:
| Characteristics | Atrial Flutter | Atrial Fibrillation |
|---|---|---|
| Electrical Pattern | Regular, sawtooth pattern | Chaotic, irregular |
| ECG Appearance | Distinct flutter waves | No distinct P waves |
| Heart Rate | Typically 250-300 BPM | Variable, often rapid |
Overlapping Features and Coexistence
Atrial flutter and atrial fibrillation can happen together or change into each other. Some people may have both at different times. This makes it hard to diagnose and treat.
Shared risk factors like heart disease and lung problems add to the challenge. These factors make managing these heart rhythm issues more complex.
It’s important for doctors to understand the differences and similarities between atrial flutter and atrial fibrillation. This knowledge helps them create better treatment plans. By recognizing both the differences and similarities, we can improve how we manage these heart rhythm problems.
Stroke Risk and Complications of Untreated Flutter
Untreated atrial flutter can cause serious problems, like a higher chance of stroke and heart failure. This condition makes blood pool and clot in the heart. These clots can then travel to the brain, leading to a stroke.
Clot Formation Mechanisms
The way clots form in atrial flutter is due to the heart’s irregular beat. This irregular rhythm causes blood to stay in the atria. Clot formation is a serious risk because it can lead to stroke or other problems if the clots move through the blood.
A medical expert said, “The risk of stroke in patients with atrial flutter is significant. Anticoagulation therapy is often needed to lower this risk.”
This condition shows how important it is to manage atrial flutter properly to avoid these problems.
| Condition | Stroke Risk | Management Strategy |
|---|---|---|
| Atrial Flutter | High | Anticoagulation Therapy |
| Atrial Fibrillation | High | Anticoagulation Therapy |
Heart Failure and Other Long-term Consequences
Untreated atrial flutter can also cause heart failure over time. The heart’s inefficient rhythm can weaken it. This makes it hard for the heart to pump blood well.
Long-term consequences include heart failure and a lower quality of life. This is due to ongoing symptoms and the emotional impact of living with an unmanaged condition.
We stress the need for early diagnosis and treatment. This can prevent these issues and improve patient results.
Living with Paroxysmal Atrial Flutter
Thriving with paroxysmal atrial flutter means being proactive about health. It’s about making lifestyle changes and learning to manage episodes. This condition requires big adjustments and smart self-care plans.
Lifestyle Modifications to Reduce Episodes
Changing your lifestyle can cut down on atrial flutter episodes. It’s important to control high blood pressure, thyroid disease, diabetes, and obesity. Also, limit alcohol and stimulants to reduce episodes.
For more tips on managing atrial fibrillation.
Self-Management During an Episode
Being ready for an episode can help manage paroxysmal atrial flutter. Stay calm and try to slow your heart rate with relaxation techniques like deep breathing or meditation. Keeping a symptom journal can also help spot triggers and patterns.
By using these strategies, you can live better and enjoy your daily life more, even with atrial flutter.
Conclusion
Understanding and managing paroxysmal atrial flutter is key to improving patients’ lives. It requires a mix of medical treatment, lifestyle changes, and education. We’ve looked into this condition, its symptoms, and treatment options.
Healthcare providers can create detailed care plans by knowing the causes and how atrial flutter works. Making lifestyle changes, like staying healthy and managing stress, helps too. These steps can lessen how often and how bad episodes get.
As cardiology advances, focusing on patient education and support is vital. Working together with patients and doctors can lead to better results. This way, we can make life better for those with paroxysmal atrial flutter.
What is paroxysmal atrial flutter?
Paroxysmal atrial flutter is a fast heart rhythm in the upper chambers of the heart. It starts and stops suddenly. Episodes can last from a few minutes to days.
How long can an atrial flutter episode last?
Episodes can last from minutes to days. Many things affect how long it lasts, like the heart rate and health conditions.
What are the common symptoms of atrial flutter?
Symptoms include heart palpitations, chest flutter, dizziness, and fainting. Symptoms vary from person to person.
What causes atrial flutter?
It’s often caused by heart disease and lung conditions like bronchitis and emphysema.
How is atrial flutter diagnosed?
Doctors use an electrocardiogram (ECG) and Holter monitoring to check the heart. They might also use advanced tests.
What is the difference between atrial flutter and atrial fibrillation?
Both are heart rhythm problems. But atrial flutter has a regular rhythm, while atrial fibrillation is irregular and fast.
Can atrial flutter increase the risk of stroke?
Yes, it can because it can cause blood clots. Managing it is key to prevent stroke.
How is atrial flutter treated?
Treatment includes managing episodes and long-term control. Procedures like catheter ablation and surgery are also options.
Can lifestyle changes help manage paroxysmal atrial flutter?
Yes, making lifestyle changes can help. Self-management during episodes also improves quality of life.
What is the connection between respiratory illnesses and atrial flutter?
Respiratory illnesses can harm the heart and lead to atrial flutter.
What are the complications of untreated atrial flutter?
Without treatment, it can cause heart failure and stroke risk. Early treatment is key to avoid these problems.
References
- WebMD. (2024, January 12). Atrial flutter: Types, symptoms, causes, tests … Retrieved from https://www.webmd.com/heart-disease/atrial-fibrillation/atrial-flutter WebMD
- American Heart Association. (2025, March 26). What is atrial flutter? Retrieved from https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af/atrial-flutter www.heart.org
- National Health Service. (2025, January 13). Atrial fibrillation. Retrieved from https://www.nhs.uk/conditions/atrial-fibrillation/ nhs.uk



































