Last Updated on November 27, 2025 by Ugurkan Demir

Septoplasty is a surgery to fix a deviated nasal septum. This condition makes breathing hard. What is septoplasty? A complete definition and guide to the surgery used to straighten the nasal septum and improve breathing.
A misaligned septum can really affect your life. Septoplasty is a simple surgery. It fixes the septum to help you breathe better.
At top hospitals like Liv Hospital, they use the latest in surgery. They focus on the patient to get great results in fixing noses.
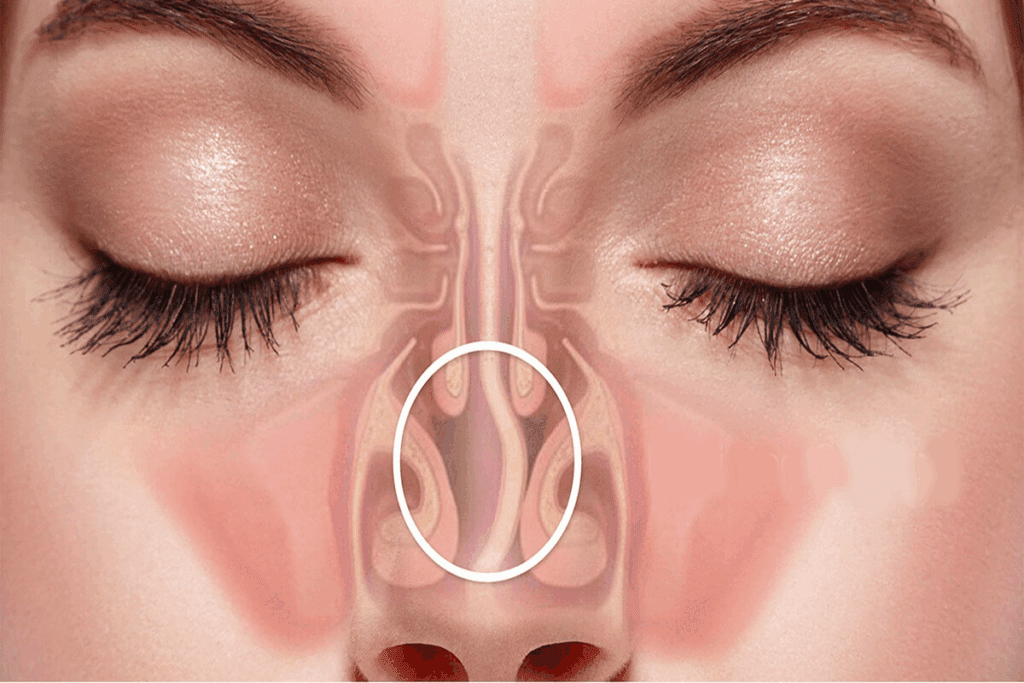
Septoplasty is a surgery to fix a deviated nasal septum. This septum is a wall of cartilage and bone that divides the nasal passages. A deviation can block airflow, causing breathing problems and other respiratory issues.
Understanding septoplasty helps people see how it can solve these problems.
Septoplasty is a surgery to fix a deviated nasal septum. It involves adjusting or removing parts of the septum to improve airflow. An otolaryngologist (ENT specialist) performs it, often under local or general anesthesia.
The main goal is to enhance respiratory function by straightening the septum. This reduces nasal obstruction, improving breathing and reducing nasal congestion. It also lowers the risk of sinus infections.
Septoplasty is often talked about with rhinoplasty. While both are nasal surgeries, they have different goals. Rhinoplasty is for cosmetic changes, and septoplasty is to improve breathing by fixing the septum.
Some people have both procedures at once, called septorhinoplasty. This way, they can fix breathing issues and improve the nose’s look in one surgery.
Septoplasty has changed a lot over time. Early attempts to fix nasal septum deviations were simple. Now, thanks to better technology and surgical methods, septoplasty is more precise and less invasive.
Today, septoplasty uses endoscopic tools for smaller cuts and quicker healing. These improvements make septoplasty a good choice for those with a deviated nasal septum.

The nasal septum is a wall made of cartilage and bone. It divides the nasal passages into two sides. A deviated septum happens when this wall is crooked, causing breathing problems.
The nasal septum has cartilage and bone parts. It’s covered by a mucous membrane that warms and humidifies the air. The septum must be straight for air to flow freely.
Key components of the nasal septum include:
Septal deviation can be caused by several factors, including:
Understanding these causes is key to diagnosing and treating septal deviation effectively.
Studies show that between 22% and over 70% of people have some septal deviation. This range varies due to study differences and diagnostic criteria.
Study Population | Prevalence of Septal Deviation |
General US Population | 22% |
Patients with Nasal Symptoms | 70% |
Surgical Candidates | 85% |
The high prevalence of septal deviation shows its importance. Accurate diagnosis and treatment can greatly improve life quality for those affected.
Knowing the signs of a deviated septum can help you decide if septoplasty is needed. A deviated septum can cause many symptoms that affect your life. We will list the common signs and symptoms that might need septoplasty.
A deviated septum often makes breathing hard because of nasal blockage. If the septum is off-center, it can block one or both nasal passages. This makes it hard to breathe through the nose.
This blockage can lead to breathing through the mouth. This can cause dry mouth and other breathing problems.
A deviated septum can also cause snoring and sleep apnea. When you can’t breathe through your nose, you breathe through your mouth. This increases the chance of snoring.
In severe cases, it can cause sleep apnea. This is when breathing stops and starts while you sleep. Both conditions can hurt your sleep quality and health.
People with a deviated septum often get sinus infections (sinusitis) again. This is because of the bad airflow and drainage in the nasal passages. Also, the dryness from blockage can cause nosebleeds.
These infections and nosebleeds can mean you might need septoplasty.
If you have trouble breathing, keep getting sinus infections, snore a lot, or have trouble sleeping, see an otolaryngologist. They can check how bad your nasal septum deviation is. They might suggest septoplasty as treatment.
Symptom | Description | Potential Impact |
Breathing Difficulties | Nasal obstruction causing difficulty breathing through the nose | Mouth breathing, dry mouth, respiratory issues |
Snoring and Sleep Apnea | Nasal obstruction leading to snoring and potentially sleep apnea | Poor sleep quality, health complications |
Recurrent Sinus Infections | Abnormal airflow and drainage issues causing sinusitis | Recurring infections, facial pain, pressure |
Nosebleeds | Dryness and irritation causing nasal bleeding | Frequent nosebleeds, nasal discomfort |
Finding the right treatment for a deviated septum starts with a detailed diagnosis. We use a mix of physical checks, special tests, and scans to see how the nasal septum is doing.
The first step is a thorough check-up. We use anterior rhinoscopy to look into the nasal cavity. This helps us see if the septum is off and how it affects breathing.
Nasal palpation is also done to feel for any soft spots or odd shapes. These checks tell us a lot about the septum and if we need more tests.
Nasal endoscopy is key for looking at the nasal septum and its area. A flexible or rigid endoscope is put into the nose to see the nasal passages and sinuses up close. It finds any blockages or odd shapes that might be causing problems.
Imaging tests are important for figuring out if septoplasty is needed. CT scans give clear pictures of the nasal septum, sinuses, and nearby areas. They show how big the septum’s bend is and if there’s any sinus infection.
X-rays might be used sometimes to look at the nasal passages and sinuses. But CT scans are usually better because they show more detail.
By looking at the results from physical checks, nasal endoscopy, and scans, we can accurately diagnose a deviated septum. This way, we make sure patients get the best treatment for their needs.
There are non-surgical ways to deal with a deviated septum before trying septoplasty. These options can help some people feel better without surgery.
There are medicines to help with a deviated septum. Decongestants can lessen nasal stuffiness. Antihistamines can help with allergies that make breathing harder. Nasal corticosteroids also reduce swelling in the nose.
It’s important to talk to an ear, nose, and throat doctor to find the right medicine. Everyone reacts differently to these drugs.
Nasal strips are a simple way to open up the nose. They stick to the nose and can help during sleep.
Other devices, like nasal dilators, can also help. They don’t fix the septum but can ease symptoms for some.
If these non-surgical methods don’t work, septoplasty might be next. A doctor will decide this after checking how well treatments have worked and how bad the symptoms are.
Knowing when these treatments don’t work is key. We’ll help you figure out what to do next based on your situation.
Understanding septoplasty is key for those thinking about it. We’ll walk you through the steps, from start to finish.
Before septoplasty, a detailed check-up is done. This includes a physical exam, nasal endoscopy, and CT scans.
Key steps in preoperative preparation include:
Septoplasty can be done with local or general anesthesia. Local anesthesia numbs the area, while general anesthesia makes you unconscious.
The choice of anesthesia is typically determined by:
The procedure starts with an incision on one side of the nasal septum. Then, the deviated parts are realigned or removed. The exact method depends on the case.
The surgical process generally includes:
Septoplasty surgery lasts from 30 to 90 minutes. Most patients go home the same day. Some might need to stay for observation.
Factors influencing the duration of the surgery include:
Septoplasty recovery is a detailed process. It involves post-operative care, pain management, and activity levels. Understanding these steps is key to a smooth recovery.
The first days after surgery are critical. Monitoring your condition closely and following instructions are essential. Having someone with you for 24 hours is recommended.
Immediate care includes:
Managing pain is a big part of recovery. We give pain medication to help. It’s important to take it as directed and report any severe pain or side effects.
Other ways to ease discomfort include:
Recovery times vary, but most see big improvements in a few weeks. Here’s a general guide:
Timeframe | Expected Recovery Progress |
1-2 weeks | Significant reduction in nasal congestion and swelling |
2-4 weeks | Gradual improvement in breathing and less nasal discharge |
4-6 weeks | Most patients return to normal activities, with continued improvement in nasal function |
Following activity restrictions is important for a successful recovery. Avoid:
By following these guidelines and our post-operative instructions, you can reduce the risk of complications. This ensures the best outcome from your septoplasty surgery.
Septoplasty, like any surgery, has its own risks and complications. It’s generally safe, but knowing these risks is key for making informed choices.
After septoplasty, you might feel nasal congestion, swelling, or discomfort. Some people might feel temporary numbness or changes in their nose’s sensation. These effects usually go away in a few weeks.
Minor bleeding or bruising around the nose and eyes can also happen. These are usually easy to manage with the right care after surgery.
Though rare, serious issues can occur. These include big bleeding, infection, or a hole in the nasal septum. In some cases, the nose’s shape might change.
It’s important to know about these serious risks and talk to your doctor about them.
After septoplasty, the nasal septum might move again over time. Some might also face dryness or crusting in their nose.
Understanding these long-term effects is important for managing your expectations and getting the best results from the surgery.
The need for a second surgery after septoplasty varies. Some studies show up to 15% of patients might need another surgery. The complexity of the initial issue and the surgery method play a big role.
Talking to a qualified doctor about the chance of needing a second surgery can help set realistic goals.
Understanding insurance for septoplasty can be tricky. Patients must consider several factors to figure out what they’ll pay out of pocket. Septoplasty is often needed when a deviated septum blocks the nose too much.
To get insurance for septoplasty, it must be medically necessary. An ear, nose, and throat doctor (ENT) will check how bad the blockage is. They’ll also see how it affects your life.
Key factors that determine medical necessity include:
The price of septoplasty varies a lot. It depends on where you are, the surgeon’s fee, and the hospital costs. On average, septoplasty can cost between $3,000 and $8,000 or more in the US.
Cost Component | Average Cost Range |
Surgeon’s Fee | $1,500 – $3,500 |
Facility Fee | $1,000 – $3,000 |
Anesthesia Fee | $500 – $1,500 |
If you have insurance, your costs can be much lower. You might pay between $500 to $2,000. This depends on your deductible, copays, and coinsurance.
It’s important to know what your insurance covers before septoplasty. Here are some key questions to ask your insurance provider:
If insurance doesn’t cover enough or costs are too high, there are financing options. Many healthcare providers offer payment plans. This lets patients pay for septoplasty in smaller amounts over time.
Some common financing options include:
When thinking about septoplasty, it’s key to make a well-informed choice. Knowing what the surgery does, its good points, and possible downsides helps. This way, patients can decide if it’s the right choice for them.
We’ve looked at septoplasty from different angles. We’ve talked about what it is, why it’s done, and how it’s diagnosed. We’ve also discussed possible problems that might come up.
Deciding on septoplasty means looking at the good sides against the bad. It’s also important to think about other ways to fix the issue. Talking to an ear, nose, and throat doctor is a big step. They can help figure out the best treatment for you.
By carefully thinking about septoplasty and getting advice from experts, people can make a choice that fits their needs and health goals.
Septoplasty is a surgery to fix a deviated nasal septum. This is the cartilage and bone that divides the nasal cavity. It aims to improve breathing and reduce nasal blockage.
A deviated nasal septum happens when the thin wall between the nasal passages is off-center. This makes one side smaller, causing breathing issues and congestion.
Symptoms include nasal congestion and trouble breathing. You might also have nosebleeds, facial pain, and a loss of smell. Some people snore, have sleep apnea, or get sinus infections often.
The surgery starts with an incision on the septum’s side. Then, the deviated parts are fixed or removed. The mucosal lining is reattached. It’s done under anesthesia, and the method varies based on the case.
Recovery time is usually one to two weeks. Swelling and bruising take a few days to a week to go down. You might feel nasal congestion and discomfort for weeks.
Risks include bleeding, infection, and changes in the nose’s shape. Serious problems are rare. Always talk about risks with your surgeon.
Insurance coverage varies. If the surgery is needed to fix a deviated septum, it might be covered. Check with your insurance to see what’s covered.
Yes, septoplasty can be done with other surgeries like turbinate reduction. This can be more efficient and shorten recovery time.
You’ll need a thorough check-up by an otolaryngologist. Stop smoking and avoid certain medications. Arrange for a ride home after surgery.
Non-surgical options include nasal strips and medications. But, they don’t fix the septum’s deviation. Septoplasty is considered when these options fail.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!