Last Updated on November 26, 2025 by Bilal Hasdemir

Acute Myeloid Leukemia (AML) is a serious blood cancer that affects adults worldwide. Getting a diagnosis of AML can be scary. But, it’s good to know that chemotherapy has greatly improved treatment outcomes for many.
Chemotherapy is a key part of AML treatment. It’s often customized for each patient’s type of leukemia. For AML, doctors usually use cytarabine and anthracycline-based treatments. These can help over 60% of younger adults go into remission, which is very hopeful for many.
At Liv Hospital, we focus on innovative, patient-centered care. Knowing the cure rate and prognosis for AML is key for patients to make smart treatment choices.
Key Takeaways
- AML is a serious blood cancer, but chemotherapy can lead to remission in many patients.
- Chemotherapy is tailored to the leukemia subtype, with cytarabine and anthracycline-based regimens being standard for AML.
- The cure rate for AML varies, but over 60% of younger adults can achieve remission with chemotherapy.
- Understanding the prognosis and cure rate is essential for patients to make informed decisions.
- Liv Hospital is committed to providing world-class, patient-focused care for AML patients.
Understanding Acute Myeloid Leukemia (AML)
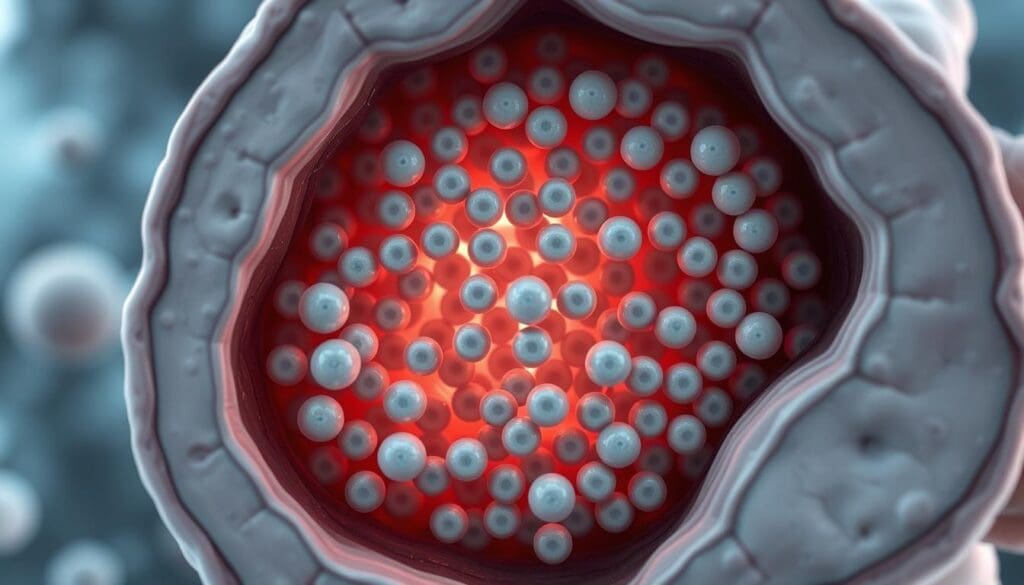
Acute myeloid leukemia (AML) is a blood cancer that messes with how blood cells are made. It’s when bad cells in the bone marrow grow too fast. This stops normal blood cells from being made.
What Defines AML as a Blood Cancer
AML is a blood cancer because it messes with blood cells and the bone marrow. The bone marrow is where blood cells are made. AML makes it hard to make healthy blood cells.
The hallmark of AML is the accumulation of immature myeloid cells in the bone marrow and peripheral blood. These cells, known as blasts, can’t fight infections or help the body make healthy blood cells.
How AML Differs from Other Leukemias
AML is different from other leukemias like CLL and ALL. CLL grows slowly and affects lymphoid cells. AML is fast-growing and affects myeloid cells.
The distinction between AML and ALL lies in the cell lineage; AML affects myeloid cells, whereas ALL involves lymphoid cells. This difference is key for choosing the right treatment.
Risk Factors and Causes
Many things can increase your chance of getting AML. These include genes you might have, chemicals you’ve been exposed to, and treatments like chemotherapy or radiation. Getting older also raises your risk.
- Genetic mutations and chromosomal abnormalities play a big role in AML.
- Being around certain chemicals, like benzene, can raise your risk of AML.
- Having had chemotherapy or radiation therapy can also up your risk.
Diagnosis and Classification of AML

To diagnose AML, doctors use many tools and techniques. The process is detailed and involves several steps. These steps help identify the disease and its characteristics accurately.
Diagnostic Methods
Diagnosing AML often includes a bone marrow biopsy, blood tests, and genetic analysis. A bone marrow biopsy is key as it lets doctors check bone marrow cells. This helps find out if leukemia is present and what type it is.
Blood tests are also vital for looking at blood cells and finding any oddities. Genetic analysis, like cytogenetic analysis, is used to spot genetic mutations. These mutations can affect how the disease progresses and how well it responds to treatment.
The diagnostic process is thorough. It covers checking cell morphology, immunophenotyping, and molecular testing. This ensures a full understanding of the disease.
AML Subtypes and Their Significance
AML is not just one disease but a group with different traits. The French-American-British (FAB) and World Health Organization (WHO) classifications help sort AML into subtypes. These classifications are based on cell type and differentiation level.
Knowing the subtype is key for predicting prognosis and treatment. The WHO classification is more detailed. It includes genetic and molecular traits, aiding in choosing targeted therapies.
Staging and Risk Stratification
Unlike some cancers, AML isn’t staged traditionally. Instead, risk stratification predicts treatment response and prognosis. Factors like genetic mutations, patient age, and health are assessed. This helps sort patients into risk groups.
Risk stratification changes as new genetic and molecular data emerges. It’s essential for tailoring treatment plans for AML patients.
Standard Treatment Approaches for AML
Acute Myeloid Leukemia (AML) treatment has seen big changes. We’ll look at the main ways doctors fight this disease today.
Overview of Treatment Protocols
AML treatment plans aim for remission and stopping the disease from coming back. They mix different therapies based on the patient’s health and needs. Chemotherapy is key in AML treatment, aiming to get rid of leukemia cells.
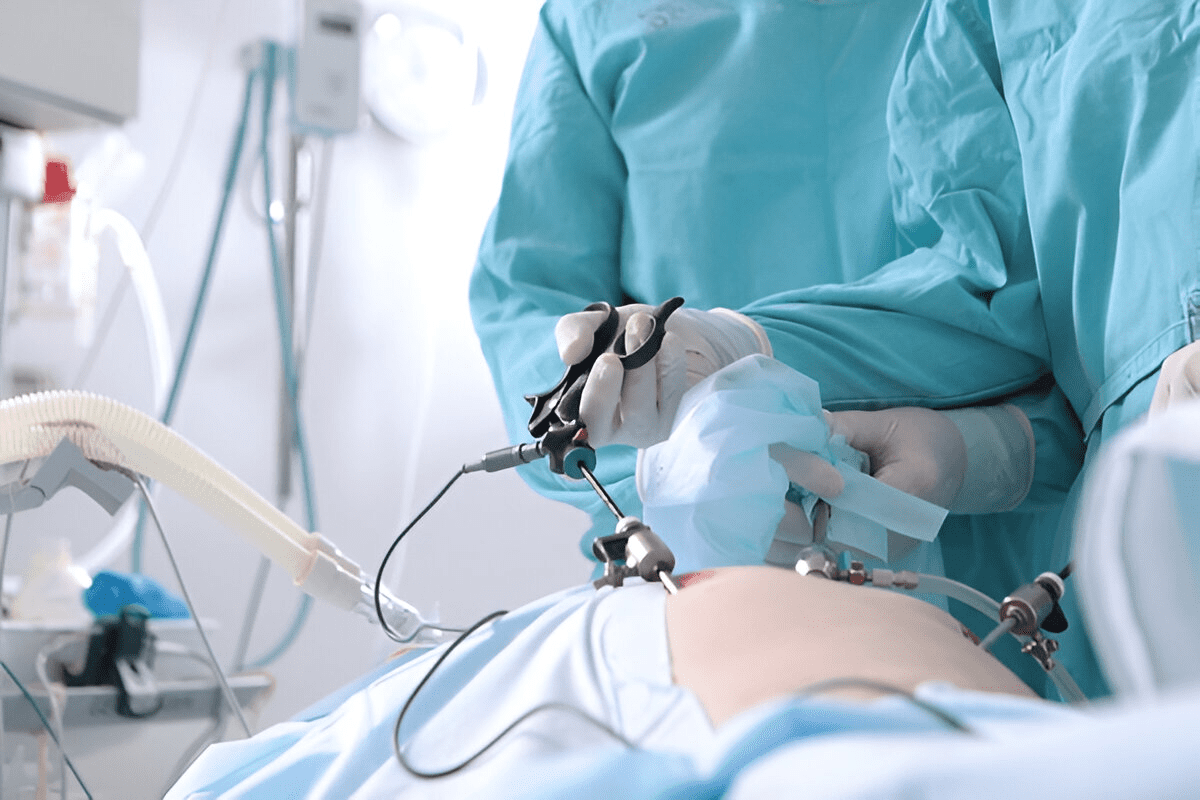
The Role of Chemotherapy as Primary Treatment
Chemotherapy is the main treatment for AML. It uses drugs like cytarabine and anthracyclines to kill leukemia cells. The choice of chemotherapy depends on the patient’s age, health, and AML type. Induction chemotherapy tries to get the patient into remission first. Then, consolidation therapy helps keep the disease away.
Stem Cell Transplantation Options
Stem cell transplantation can cure AML by replacing bad bone marrow with healthy cells. There are two types: allogeneic (from a donor) and autologous (using the patient’s own cells). The choice depends on the patient’s risk and if a donor is available.
Targeted Therapies and Immunotherapies
Targeted therapies and immunotherapies are new options for AML treatment. They aim to target leukemia cells without harming normal cells. For example, FLT3 inhibitors and IDH inhibitors have shown promise in trials.
Chemotherapy Regimens for AML
Chemotherapy for AML is divided into three stages: induction, consolidation, and maintenance. Each stage has a unique purpose.
Induction Chemotherapy
Induction chemotherapy is the first step. It aims to kill leukemia cells in the bone marrow. The main goal is to make the number of leukemia cells undetectable.
We use a mix of drugs, like cytarabine and anthracyclines, to achieve this goal.
Consolidation Therapy
After achieving remission, consolidation therapy follows. It targets any remaining leukemia cells that are hard to find. This phase is key to lowering the risk of relapse.
High-dose cytarabine or other drugs are often used in this phase.
Maintenance Treatment
Maintenance treatment is sometimes given after consolidation. This phase uses less intense chemotherapy for a longer time.
Cytarabine and Anthracycline Mechanisms
Cytarabine stops leukemia cells from growing by messing with DNA. Anthracyclines work by breaking DNA strands, which kills leukemia cells.
- Cytarabine is given through an IV or under the skin.
- Anthracyclines are given through an IV.
Administration Methods and Duration
The length and way of giving chemotherapy can change based on the plan and patient. Induction is short, but consolidation and maintenance can last months or years.
Knowing about the different chemotherapy phases and the drugs used is key to fighting AML. We make treatment plans that fit each patient’s needs for the best results.
Is Acute Myeloid Leukemia Curable?
Understanding if Acute Myeloid Leukemia (AML) is curable is complex. It depends on many factors that affect treatment success. The idea of a “cure” in AML is not simple. It changes based on the disease and how it’s treated.
Defining “Cure” in the Context of AML
In AML, a “cure” means the disease is gone and won’t come back. But, what counts as a cure can change. It depends on how long the remission lasts and the patient’s health. We talk about complete remission and functional cure to grasp the situation better.
Complete Remission vs. Functional Cure
Complete remission means no leukemia cells are found in the bone marrow or blood. Blood cell counts are normal. A functional cure means the patient stays disease-free for a long time, often five years or more after treatment. Knowing the difference between these two is key to understanding how well AML treatment works.
Current Cure Rate Statistics
The cure rate for AML changes a lot. It depends on age, health, and the AML subtype. Younger patients usually do better than older ones. Studies show that the cure rate for AML patients who get allogeneic stem cell transplant can be between 30% and 50% or more, based on risk.
| Age Group | Cure Rate Range |
|---|---|
| Young Adults (18-40) | 40% – 60% |
| Middle-Aged Adults (41-60) | 20% – 40% |
| Older Adults (Over 60) | 10% – 20% |
These numbers show why treatment needs to be tailored to each patient. They also highlight the need for more research. This is to improve AML treatment results for all ages and risk levels.
Factors Affecting AML Prognosis
AML prognosis depends on many factors. These include the patient’s health and the disease itself. Knowing these factors helps us choose the best treatment and predict how well a patient will do.
Age and Overall Health
Age is a big factor in AML prognosis. Older adults often have a harder time because their bodies are weaker. They also might have other health issues.
Being in good health is important too. Patients who are healthier can usually handle stronger treatments better.
We look at how well a patient can do things before starting tough treatments. If they can handle it, they might do better with aggressive treatments.
Genetic and Molecular Markers
Genetic and molecular markers are key in figuring out AML prognosis. Some genetic changes, like FLT3-ITD mutations, mean a worse outlook. But, other changes, like NPM1 mutations without FLT3-ITD, might be better.
By looking at these markers, we can tailor treatments to fit each patient’s leukemia. This makes treatments more effective.
Response to Initial Treatment
How well a patient does after the first treatment is very important. If they get into complete remission, it’s a good sign. It means they might live longer.
We watch how patients react to treatment closely. If they do well, we keep going. But if not, we might change our plan to help them more.
Comorbidities and Complications
Having other health problems or complications can affect AML prognosis a lot. Patients with other health issues might face more risks during treatment. We have to manage these risks carefully.
We try to prevent complications with supportive care. This includes preventing infections and watching for signs of treatment side effects. By tackling these issues early, we can make patients’ lives better and longer.
AML Survival Rates by Age Group
Age is a key factor in how well patients with Acute Myeloid Leukemia (AML) do. The chances of survival vary a lot based on age. This makes age very important in predicting how well a patient will do.
Prognosis for Young Adults (18-40)
Young adults with AML usually have a better chance of recovery than older ones. They often have fewer health problems and can handle stronger treatments. Younger patients are more likely to get rid of the cancer completely and live longer.
Middle-Aged Adults (41-60)
Middle-aged adults have a middle ground in AML survival chances. They are generally healthier than older adults but may have health issues and certain leukemia types that affect treatment. It’s important to consider their health and leukemia type when choosing treatment.
Older Adults (Over 60)
Older adults face big challenges with AML. They often have more health problems, less energy, and more serious leukemia types. This means they usually have lower survival rates and may not handle strong chemotherapy as well. We need to find treatments that work well but are also gentle on them.
Five-Year Survival Statistics
Five-year survival rates give us a good idea of long-term AML outcomes. The survival chances for AML patients vary a lot by age. Here’s a table showing these differences:
| Age Group | Five-Year Survival Rate |
|---|---|
| 18-40 years | 40-50% |
| 41-60 years | 20-30% |
| Over 60 years | 5-10% |
These numbers highlight how important age is in AML survival. We keep learning about AML and working on treatments that fit each age group better. Our goal is to help patients of all ages live longer and better lives.
Managing Side Effects and Complications
Managing side effects of AML treatment is key to better patient outcomes. We face many challenges in AML treatment. It’s important to tackle the side effects and complications that can happen.
Common Side Effects of AML Treatment
AML treatment can cause a variety of side effects. These range from mild to severe. Common issues include fatigue, nausea, hair loss, and a higher risk of infections. These side effects can really affect a patient’s life quality.
Common Side Effects:
- Fatigue
- Nausea and vomiting
- Hair loss
- Increased risk of infections
- Mucositis
Infection Risk and Prevention
AML treatment makes patients more prone to infections. We stress the need for infection prevention. This includes:
- Frequent hand hygiene
- Avoiding close contact with sick people
- Keeping vaccinations up-to-date
Long-Term Health Considerations
Long-term health is vital for AML survivors. We watch for late effects of treatment. This includes heart problems and secondary cancers.
Cardiac Effects
Some treatments for AML can harm the heart. We team up with cardiologists to manage these risks.
Secondary Malignancies
There’s a chance of getting secondary cancers after AML treatment. We stress the need for ongoing care to catch any issues early.
| Long-Term Complication | Risk Factors | Management Strategies |
|---|---|---|
| Cardiac Effects | Anthracycline chemotherapy, radiation therapy | Regular cardiac monitoring, lifestyle modifications |
| Secondary Malignancies | Previous chemotherapy or radiation, genetic predisposition | Long-term follow-up, surveillance for early detection |
By tackling these side effects and complications, we can enhance care and outcomes for AML patients.
Recurrence and Relapse: What to Expect
It’s important for AML patients to know about recurrence and relapse risks. Relapse happens when leukemia comes back after treatment. We’ll look at what increases this risk and what to do if it happens.
Risk Factors for Relapse
Several things can make AML relapse more likely. Genetic and molecular markers are key; some mutations make leukemia harder to treat. Age and health also matter, as older or sicker patients face higher risks.
How well a patient responds to treatment is also important. Those who don’t fully respond or have a short remission are at higher risk. We watch these patients closely to adjust their treatment.
Treatment Options After Relapse
When AML relapses, treatment choices depend on several factors. These include how long the first remission lasted, the patient’s health, and any new genetic changes. Re-induction chemotherapy is often used to try to get a second remission.
For some, stem cell transplantation might be a chance for a cure. We also look into targeted therapies and immunotherapies for managing relapsed AML.
Prognosis Following Recurrence
The outlook after AML relapse varies a lot. Important factors include how long the first remission lasted, the patient’s age, and health. A longer first remission usually means a better chance after relapse.
We create a treatment plan for each patient, considering their unique situation and AML details. This personalized approach aims to improve their chances of a good outcome.
Advances Improving AML Outcomes
AML treatment is changing fast, thanks to new ideas in precision medicine and clinical trials. We’re seeing big changes in how we treat this complex disease.
Novel Therapeutic Approaches
New ways to treat AML are being developed. These include targeted therapies that target specific genetic changes in leukemia cells.
Targeted therapies are showing great promise. For example, FLT3 inhibitors are now key in treating patients with FLT3 mutations.
Precision Medicine in AML
Precision medicine is changing AML treatment. It tailors treatments to each patient based on their leukemia’s genetic makeup.
Next-generation sequencing (NGS) and other advanced tests help understand AML’s genetics. This lets doctors choose the best treatments for each patient.
Clinical Trials and Emerging Treatments
Clinical trials are key in finding new AML treatments. They give patients access to new therapies and help us learn more about AML.
New treatments being tested include checkpoint inhibitors, adoptive T-cell therapies, and other immunotherapies.
| Treatment Type | Description | Potential Benefits |
|---|---|---|
| FLT3 Inhibitors | Targeted therapy for AML with FLT3 mutations | Improved response rates, possible longer survival |
| Checkpoint Inhibitors | Immunotherapy that boosts the immune system | Better immune response against tumors |
| Adoptive T-cell Therapies | Immunotherapy using genetically modified T-cells | Possible long-lasting remissions |
Future Directions in AML Management
As we learn more about AML, treatments will keep getting better. Using artificial intelligence and machine learning could make treatments even more personalized.
The future of AML treatment will mix old and new approaches. This offers hope for better outcomes for patients and doctors.
Conclusion
Acute Myeloid Leukemia (AML) is a complex disease that needs a detailed treatment plan. We talked about the cure rate and how well patients do, based on the disease’s types and risk factors.
There are different ways to treat AML, like chemotherapy, stem cell transplants, and targeted therapies. How well these work depends on the patient’s age, health, and genetic markers.
New ways to manage AML, like precision medicine, are making treatments better. It’s key to have a treatment plan that fits each patient’s needs and the latest research.
Knowing about AML and its treatments helps patients and doctors work together. This way, they can aim for the best outcome and increase the chances of beating this tough disease.
FAQ
Can acute myeloid leukemia be cured?
Yes, some people with acute myeloid leukemia (AML) can be cured. But, it depends on many things. These include the patient’s age, health, and how well they respond to treatment.
What is the cure rate for AML?
The cure rate for AML changes based on the patient’s age and other factors. Younger patients and those with certain genetic markers tend to have a higher cure rate.
Is AML curable in older adults?
Older adults face a tougher battle with AML. Yet, some can achieve remission and possibly be cured. But, the cure rate is generally lower for this age group.
What are the treatment options for AML?
Treatments for AML include chemotherapy, stem cell transplantation, targeted therapies, and immunotherapies. The right treatment depends on the patient’s health, genetic markers, and how they first respond to treatment.
How does chemotherapy work for AML?
Chemotherapy is a main treatment for AML. It kills leukemia cells in the bone marrow. Doctors often use cytarabine and anthracycline-based regimens.
What is the role of stem cell transplantation in AML treatment?
Stem cell transplantation replaces the patient’s bone marrow with healthy stem cells. This can lead to a cure. It’s often used after chemotherapy has worked.
What are the common side effects of AML treatment?
Side effects of AML treatment include infection risk, fatigue, hair loss, and nausea. Long-term effects like cardiac issues and secondary cancers can also happen.
Can AML relapse after treatment?
Yes, AML can come back after treatment. The risk of relapse depends on several factors. These include how well the patient first responds to treatment and genetic markers.
What are the treatment options after AML relapse?
After AML relapse, treatments include more chemotherapy, stem cell transplantation, and targeted therapies. The choice depends on the patient’s health and previous treatments.
What is the prognosis for AML patients?
The prognosis for AML patients varies. It depends on age, health, genetic markers, and treatment response. Younger patients with favorable genetic markers usually have a better outlook.
Are there any new treatments being developed for AML?
Yes, new treatments for AML are being developed. These include novel therapies, precision medicine, and immunotherapies. Clinical trials are ongoing to test their safety and effectiveness.
What is the five-year survival rate for AML?
The five-year survival rate for AML varies. It depends on age and other factors. Generally, younger patients and those with favorable genetic markers have a higher survival rate.
How does age affect AML prognosis?
Age is a big factor in AML prognosis. Older adults usually have a poorer prognosis than younger patients.
What is the impact of genetic markers on AML prognosis?
Genetic markers, like certain chromosomal abnormalities, greatly affect AML prognosis. Patients with favorable genetic markers tend to have a better prognosis.
References
- American Cancer Society (ACS): https://www.cancer.org/cancer/types/acute-myeloid-leukemia/treating/response-rates.html
- National Cancer Institute (NCI): https://www.cancer.gov/types/leukemia/hp/adult-aml-treatment-pdq
- Haematologica: https://haematologica.org/article/view/haematol.2024.285805
- National Center for Biotechnology Information (NCBI) / PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC11966364/
- UT Health San Antonio News: https://news.uthscsa.edu/cracking-cancers-code-new-research-identifies-novel-drug-target-for-acute-myeloid-leukemia-treatment/