Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we focus on top-notch neurological care. We dive into the link between scar tissue on the brain and epilepsy. We see how brain scarring can cause seizures.
Cerebral scarring, or gliosis, happens after injury, infection, or surgery. It can mess with the brain’s electrical signals. This might lead to seizures and is a big part of epilepsy.
Research shows many things can cause epilepsy. These include genes, infections, and head injuries.
Key Takeaways
- Scar tissue on the brain can disrupt normal electrical signaling, potentially leading to seizures.
- Cerebral scarring is a significant factor in the development of epilepsy.
- Various factors contribute to the development of epilepsy, including genetic conditions and head trauma.
- Understanding the underlying mechanisms of epilepsy is key for managing it well.
- Liv Hospital is dedicated to advanced care for epilepsy patients.
The Nature of Scar Tissue on Brain
Scar tissue in the brain forms in a complex way. It affects how the brain works. It can happen due to injuries, infections, or other brain problems.
What Is Cerebral Scarring or Gliosis?
Cerebral scarring, or gliosis, happens when brain cells called glial cells grow more. This is the brain’s way to fix itself after damage. It tries to cover up and heal damaged spots.
Studies link scar tissue to brain injuries and infections (Blumcke I et al., 2017). The process of scarring involves many steps. It’s a mix of cell and molecular actions that lead to scar tissue.
How Scar Tissue Forms in Brain Tissue
Scar tissue in the brain starts with injury. This injury sets off inflammation. The brain’s immune cells, called microglia, release signals to start healing.
Then, astrocytes, a type of brain cell, grow more. They help form a scar. This scar can change the brain’s area around it. It might mess with how the brain works and even cause epilepsy.
The Formation Process of Brain Scarring
Brain scarring comes from many causes, like trauma and infection. It changes the brain’s cells and molecules. This leads to scar tissue replacing normal brain tissue.
We’ll look at how scarring happens and what causes it. This is important because scarring is linked to epilepsy.
Cellular Mechanisms of Scarring
Scarring in the brain, or gliosis, starts with cells like astrocytes and microglia. These cells grow and form a scar after brain injury. The scar is a dense network of cells and molecules.
This scar acts as a barrier around the damaged area. But, it can also change the area around it. This might affect nearby neurons and lead to epilepsy.
Common Causes of Brain Scarring
Many things can cause brain scarring, like head injuries, infections, and surgery. Head injuries are a big risk for epilepsy because they can cause scarring.
Infections like meningitis and encephalitis can also cause scarring. They lead to inflammation and damage. Surgery can cause scarring too, as part of healing.
Knowing these causes helps us understand the link between scarring and epilepsy. It also helps us find ways to prevent or lessen scarring’s effects.
Normal Brain Electrical Activity vs. Disrupted Signaling
The human brain has a complex network of electrical signals. These signals help with thinking and moving. Scar tissue can disrupt these signals, leading to epilepsy.
How Healthy Neural Networks Function
In a healthy brain, neural networks work through electrical and chemical signals. Neurons send information through electrical impulses. These impulses help the brain work fast and well.
Neural activity needs to be in sync for the brain to function right. This sync helps with movement and thinking. It keeps the brain’s electrical activity in check.
How Scarring Alters Electrical Pathways
Scar tissue in the brain can upset this balance. It can change how neurons talk to each other. This can lead to epileptogenic foci, areas that can cause seizures (Beaumont A et al., 2000).
Scar tissue can also make some neurons too excited. This can cause abnormal electrical discharges. Such hyperexcitability can lead to epileptic fits.
The Creation of Epileptogenic Foci
Epileptogenic foci are areas in the brain that can start seizures. Scar tissue can make these areas by changing how neurons work. This leads to persistent changes in brain electrical activity.
Understanding how these foci form is key to treating epilepsy. By finding the affected areas, doctors can create better treatment plans. This helps patients get the care they need.
What Causes Epilepsy: The Multifactorial Etiology
Epilepsy is a complex neurological disorder with many possible causes. Knowing these causes is key to creating effective treatments and supporting those with epilepsy.
Studies show that epilepsy can come from genetics, development, and acquired factors (Engel J Jr., 1993). Let’s dive into these factors.
Genetic Factors in Epilepsy
Genetics play a big role in epilepsy. Research has found several genetic mutations that raise the risk of epilepsy. These mutations can change how brain cells work, causing seizures.
Some important genetic factors include:
- Mutations in genes for ion channels or neurotransmitter receptors
- Genetic syndromes like tuberous sclerosis complex
- Family history of epilepsy
Developmental and Congenital Causes
Developmental and congenital issues can also lead to epilepsy. These problems can affect brain development, increasing seizure risk.
Examples of these causes include:
- Cortical dysplasia
- Brain malformations
- Perinatal brain injury
Acquired Causes Including Brain Scarring
Acquired causes, like brain scarring, are also big contributors to epilepsy. Brain scarring can happen from injuries, infections, or strokes.
Brain scarring can create areas in the brain that cause seizures. This involves changes in cells and molecules that disrupt normal brain function.
Understanding epilepsy’s many causes helps us see its complexity. It shows why we need tailored treatments for each person.
How Traumatic Brain Injury Leads to Epilepsy
Research shows a strong link between traumatic brain injury and epilepsy. Head trauma can lead to seizures, a hallmark of epilepsy. This condition is marked by recurring seizures.
The Connection Between Head Trauma and Seizures
Head trauma can alter brain function in immediate and lasting ways. This can lead to epilepsy. The injury’s severity greatly affects the risk of developing epilepsy.
Studies reveal that severe injuries, like those with penetrating trauma or significant bleeding, increase epilepsy risk.
The risk of epilepsy after a brain injury varies. Factors include injury severity, early seizures, and brain damage extent. A study found a 4-7% risk of post-traumatic epilepsy, but severe injuries raise this risk.
Post-Traumatic Epilepsy: Mechanisms and Risk Factors
Post-traumatic epilepsy involves scar tissue, neural network changes, and neuron excitability shifts. Various factors, like injury severity and genetic predisposition, influence this process.
- Severity of the initial injury
- Presence of intracranial hemorrhage
- Genetic predisposition
- Early seizures after the injury
Knowing these risk factors helps identify those at high risk. It also guides preventive and treatment efforts.
Timeline from Injury to Seizure Development
The time from injury to epilepsy can differ greatly. Some may have seizures soon after, while others may wait months or years.
| Time Frame | Risk of Developing Epilepsy |
| Within 1 year | Higher risk, if early seizures occur |
| 1-5 years | Moderate risk, based on injury severity and other factors |
| More than 5 years | Lower but ongoing risk, needing constant monitoring |
Monitoring is key for those with brain injuries. Early epilepsy detection and treatment can greatly improve outcomes.
What Brings On Epileptic Fits Related to Scarring
It’s important to know what causes epileptic fits in people with brain scarring. This knowledge helps manage epilepsy better. Brain scarring can cause epilepsy, and finding seizure triggers is key to good care.
Seizure Triggers in Patients with Brain Scarring
Many things can set off seizures in those with brain scarring. Stress, sleep deprivation, and some medicines are among them. These can make it easier for a seizure to happen (Leidy NK et al., 1999).
Every person’s triggers are different. So, finding out what triggers each person’s seizures is vital. This helps create a treatment plan that works just for them.
The Threshold Theory of Seizure Generation
The threshold theory says there’s a certain point before a seizure happens. In those with brain scarring, this point is often lower. When a trigger is applied, it can cross this threshold, causing a seizure.
This theory shows how brain scarring, triggers, and seizures are connected.
Common Precipitating Factors
There are several common things that can lead to seizures in people with brain scarring. These include:
- Stress: Both physical and emotional stress can trigger seizures.
- Sleep Deprivation: Not getting enough sleep can make seizures more likely.
- Certain Medications: Some medicines can affect how likely seizures are.
- Hormonal Changes: Changes in hormone levels can also affect seizures.
Knowing these common triggers helps us help patients avoid them. This can lower the chance of seizures happening.
Is Scar Tissue on the Brain Dangerous?
Scar tissue on the brain can be a big worry for health. It’s important to look at both the short and long-term effects. This helps us understand the dangers it poses.
Immediate and Long-term Risks
Scar tissue on the brain can cause problems right away and later on. It can lead to headaches, nausea, and vomiting. Over time, it might cause epilepsy, cognitive issues, and changes in behavior.
Studies show that scar tissue can mess with brain electrical signals. This can create epileptogenic foci – spots that can start seizures. It’s key to watch for seizure signs in these patients.
Beyond Epilepsy: Other Possible Complications
While epilepsy is a known risk, there are others too. Patients might face:
- Cognitive problems, like memory loss and trouble focusing
- Behavioral changes, like mood swings and irritability
- Motor issues, such as weakness or paralysis
- Emotional problems, like anxiety and depression
These issues can really affect a patient’s life. So, finding good ways to manage them is vital.
Factors That Determine Clinical Significance
The importance of scar tissue on the brain varies. It depends on:
- The scar’s location and size
- Why the scarring happened
- If there are other brain conditions
- The patient’s overall health and past medical issues
Knowing these factors helps doctors create better treatment plans. This way, they can lower the risks from brain scar tissue.
Common Locations of Epileptogenic Scar Tissue
The location of scar tissue in the brain is key to understanding epilepsy risk. Studies show that scarring in the hippocampus and cortex can lead to seizures.
Hippocampal Scarring and Temporal Lobe Epilepsy
Hippocampal scarring often causes temporal lobe epilepsy. This condition starts in the temporal lobe. The hippocampus is vital for memory and navigation.
Scarring in the hippocampus can come from many sources. These include:
- Traumatic brain injury
- Infections like encephalitis
- Febrile seizures
This scarring can disrupt brain activity. It can create epileptogenic foci, areas that can start seizures.
Cortical Scarring and Focal Seizures
Cortical scarring happens in the cerebral cortex, the brain’s outer layer. It’s involved in processing sensory info and controlling movement. Scarring can come from trauma, stroke, or infection.
Focal seizures start in a specific brain area. The type of seizure depends on the scarring’s location and size.
Other Critical Brain Regions
Scarring in other brain areas can also lead to epilepsy. For example, scarring in the amygdala, near the hippocampus, can cause temporal lobe epilepsy.
To grasp how scar tissue location affects epilepsy risk, let’s look at the data below:
| Brain Region | Association with Epilepsy | Common Causes of Scarring |
| Hippocampus | High risk of temporal lobe epilepsy | Trauma, infections, febrile seizures |
| Cerebral Cortex | Focal seizures depending on location | Trauma, stroke, infections |
| Amygdala | Contributes to temporal lobe epilepsy | Infections, trauma |
Knowing where and why scar tissue forms is key to treating epilepsy.
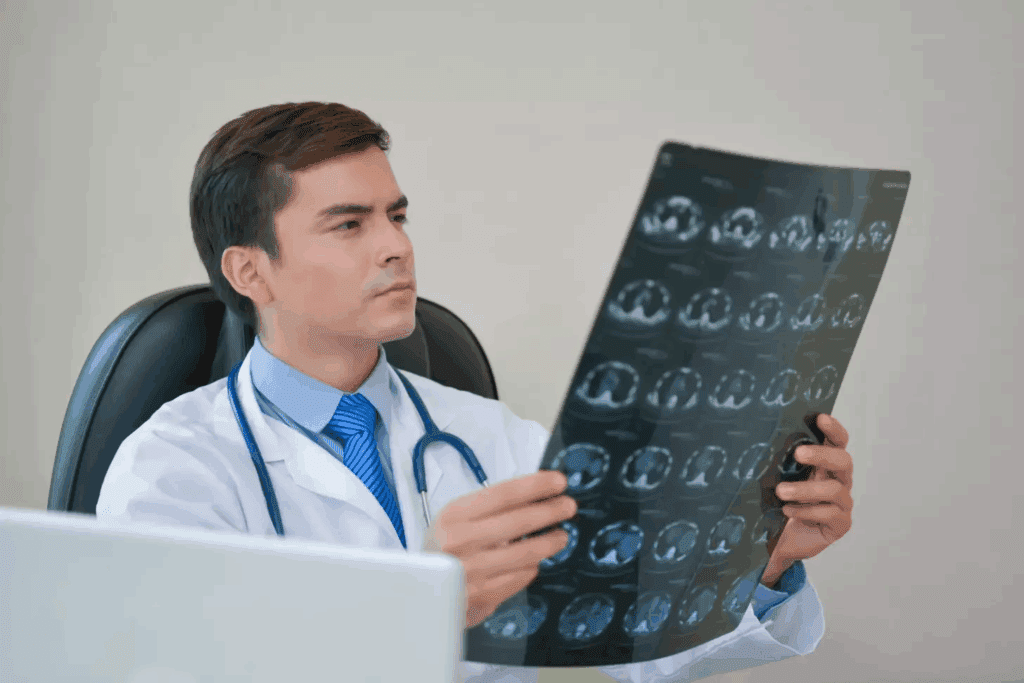
Diagnosing Scar Tissue-Related Epilepsy
Diagnosing scar tissue-related epilepsy needs both imaging and clinical checks. It’s key to manage epilepsy well. This way, doctors can make treatment plans that fit each patient’s needs.
Imaging Techniques for Detecting Brain Scarring
Imaging is key in finding scar tissue-related epilepsy. Magnetic Resonance Imaging (MRI) is top for spotting brain scarring. It shows where, how big, and what kind of scar tissue is, helping figure out if it causes seizures.
Studies show MRI is great for finding brain scarring and diagnosing epilepsy. It spots scars that CT scans miss. Advanced MRI methods like high-resolution and functional MRI help even more.
Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) also help. They check brain function and find abnormal activity. This info links scar tissue to seizures.
Clinical Evaluation and History Taking
Imaging isn’t the only thing. Clinical checks and history are also vital. A good medical history can show why brain scarring happened. It also helps understand the patient’s seizure history.
Doctors do a full check of the patient’s brain and body. They look at thinking, movement, and senses. This helps see how scar tissue affects the brain and finds seizure triggers.
- A detailed seizure history, including the frequency, severity, and characteristics of seizures
- A thorough medical history, including any previous head injuries or infections
- A neurological examination to assess cognitive function, motor skills, and sensory abilities
By using imaging, clinical checks, and history, doctors can accurately diagnose scar tissue-related epilepsy. Then, they can create a treatment plan that works.
Treatment Approaches for Scar Tissue-Induced Epilepsy
Dealing with epilepsy caused by scar tissue needs a variety of methods. Each patient’s needs and their epilepsy’s specifics are key. A complete approach is essential.
Antiepileptic Medications and Their Efficacy
Antiepileptic drugs (AEDs) are often the first choice for managing seizures from scar tissue-induced epilepsy. These drugs help stabilize abnormal brain electrical activity. We have many AEDs, including:
- Traditional AEDs: Such as carbamazepine and valproate, which work for different seizure types.
- Newer AEDs: Like lamotrigine and levetiracetam, which might be easier to tolerate and have fewer side effects.
Choosing the right AED depends on several factors. These include the type of seizure, the patient’s age, and any other health conditions. Sometimes, we need to try different drugs or combinations to find the best one.
Surgical Options for Removing Epileptogenic Scar Tissue
For those with drug-resistant epilepsy, surgery might be an option. Surgery aims to remove or disconnect the part of the brain that causes seizures. Techniques include:
- Lesionectomy: Removing the scar tissue or lesion itself.
- Lobectomy: Taking out a larger part of the brain lobe with the seizure area.
- Multiple subpial transections: Stopping seizures from spreading while keeping brain function.
Before surgery, we do detailed tests like EEG, MRI, and sometimes invasive monitoring. This helps find the exact area causing seizures.
Neuromodulation Techniques
For those not suited for surgery or who have failed surgery, neuromodulation offers alternatives. These include:
- Vagus Nerve Stimulation (VNS): A device that sends electrical impulses to the vagus nerve.
- Responsive Neurostimulation (RNS): A system that detects and responds to abnormal brain activity with targeted stimulation.
- Deep Brain Stimulation (DBS): Stimulates specific brain areas to lower seizure frequency.
These methods can cut down on seizures and improve life quality for many.
Emerging Therapies and Research Directions
Research into epilepsy treatment is always moving forward. Some promising areas include:
- Gene therapy: Targets genetic causes of epilepsy.
- Stem cell therapy: Looks into the possibility of regrowing brain cells.
- Advanced neuromodulation: Works on making stimulation techniques even better.
These new treatments offer hope for better treatments in the future. As research goes on, we learn more about epilepsy and find better ways to manage it.
Conclusion
It’s important to understand how scar tissue on the brain relates to epilepsy. This knowledge helps us find better ways to manage the condition. Studies show that scar tissue and epilepsy are connected in a complex way.
We’ve looked into what scar tissue on the brain is and how it forms. It disrupts the brain’s electrical signals, causing epilepsy. Epilepsy can come from many sources, like genetics, development, or injury, and scar tissue plays a big part.
To wrap it up, the connection between scar tissue and epilepsy is complex. More research is needed to find good treatments. By studying this connection and using a complete approach to care, we can help patients more. This will lead to better health care for everyone.
FAQ
What is the link between scar tissue on the brain and epilepsy?
Scar tissue on the brain can disrupt normal brain activity. This can lead to seizures by creating areas in the brain that cause them.
What is cerebral scarring or gliosis?
Cerebral scarring, or gliosis, is when scar tissue forms in the brain. This usually happens after injury, infection, or brain damage.
How does scar tissue form in brain tissue?
Scar tissue forms in the brain through a complex process. It involves the activation of glial cells and the deposition of scar tissue proteins.
What are the common causes of brain scarring?
Brain scarring can be caused by head trauma, infections, stroke, and other brain injuries.
How does scarring alter electrical pathways in the brain?
Scarring can change how electrical signals move in the brain. It can create abnormal connections and disrupt normal neural networks, leading to seizures.
What is the multifactorial etiology of epilepsy?
Epilepsy has many causes, including genetic, developmental, and acquired factors. Brain scarring is one of these factors.
Can head trauma cause epilepsy?
Yes, head trauma can increase the risk of developing epilepsy. It can lead to scar tissue in the brain that causes seizures.
What brings on epileptic fits related to scarring?
Various factors can trigger seizures related to scarring. These include changes in brain chemistry, sleep deprivation, and stress.
Is scar tissue on the brain always dangerous?
Not all scar tissue on the brain is dangerous. But it can increase the risk of epilepsy and other complications, depending on its location and extent.
How is scar tissue-related epilepsy diagnosed?
Doctors use imaging techniques like MRI and a thorough medical history to diagnose epilepsy related to scar tissue.
What are the treatment approaches for scar tissue-induced epilepsy?
Treatments include antiepileptic medications, surgery to remove the scar tissue, and neuromodulation techniques. New therapies are also being explored.
Can surgical removal of epileptogenic scar tissue cure epilepsy?
In some cases, removing the scar tissue can greatly reduce or stop seizures. But the success depends on the scar’s location and extent.
What are the emerging therapies for scar tissue-induced epilepsy?
New treatments include advanced medications, surgical techniques, and neuromodulation methods like gene therapy and stem cell therapy.
Where is epileptogenic scar tissue commonly located?
Scar tissue that causes seizures is often found in areas like the hippocampus, temporal lobe, and other critical brain regions.
References:
- PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC4516165/
- ScienceDirect: https://www.sciencedirect.com/science/article/abs/pii/0014488686902359
- The New England Journal of Medicine (NEJM): https://www.nejm.org/doi/full/10.1056/NEJMoa1703784
- News Medical: https://www.news-medical.net/news/20161109/Brain-surgery-helps-remove-scar-tissue-causing-seizures-in-epilepsy-patients.aspx