Last Updated on November 26, 2025 by Bilal Hasdemir

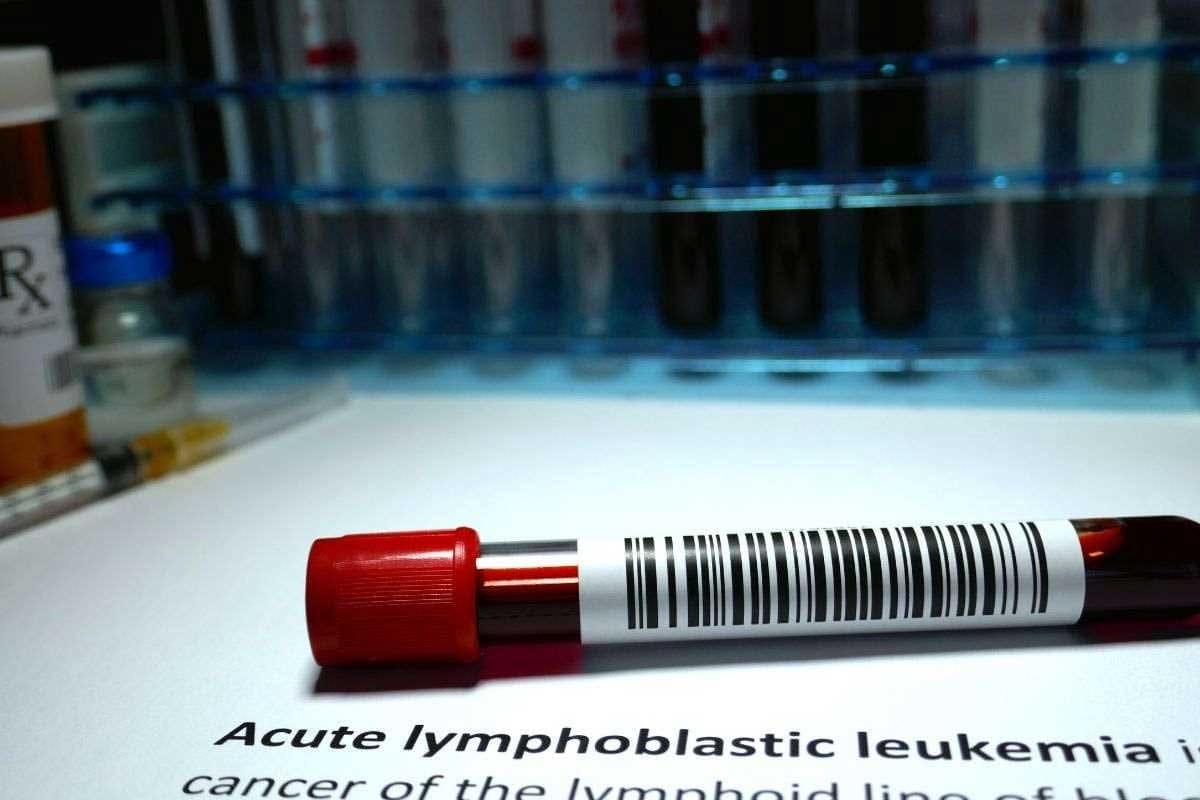
Chemotherapy is a key part of cancer treatment. It can greatly affect the body’s white blood cell (WBC) count. At Liv Hospital, we know how vital it is to watch WBC levels. This ensures patient safety and treatment success.
Chemotherapy’s effect on WBC counts is big. Regular checks are key to safely continuing treatment. Usually, a WBC count above 3,000–4,000 cells per microliter is the minimum threshold for starting chemotherapy.
We stress the need to keep WBC counts in a safe range. This range is usually between 4,000 and 11,000 cells per microliter. This helps avoid complications.
Key Takeaways
- Chemotherapy can significantly lower WBC counts.
- Regular monitoring of WBC levels is critical for patient safety.
- A WBC count above 3,000–4,000 cells per microliter is generally safe for chemotherapy.
- The acceptable WBC range for cancer patients varies based on individual health and cancer type.
- Liv Hospital prioritizes patient-centered care and rigorous monitoring of WBC counts during chemotherapy.
Understanding White Blood Cells and Their Function
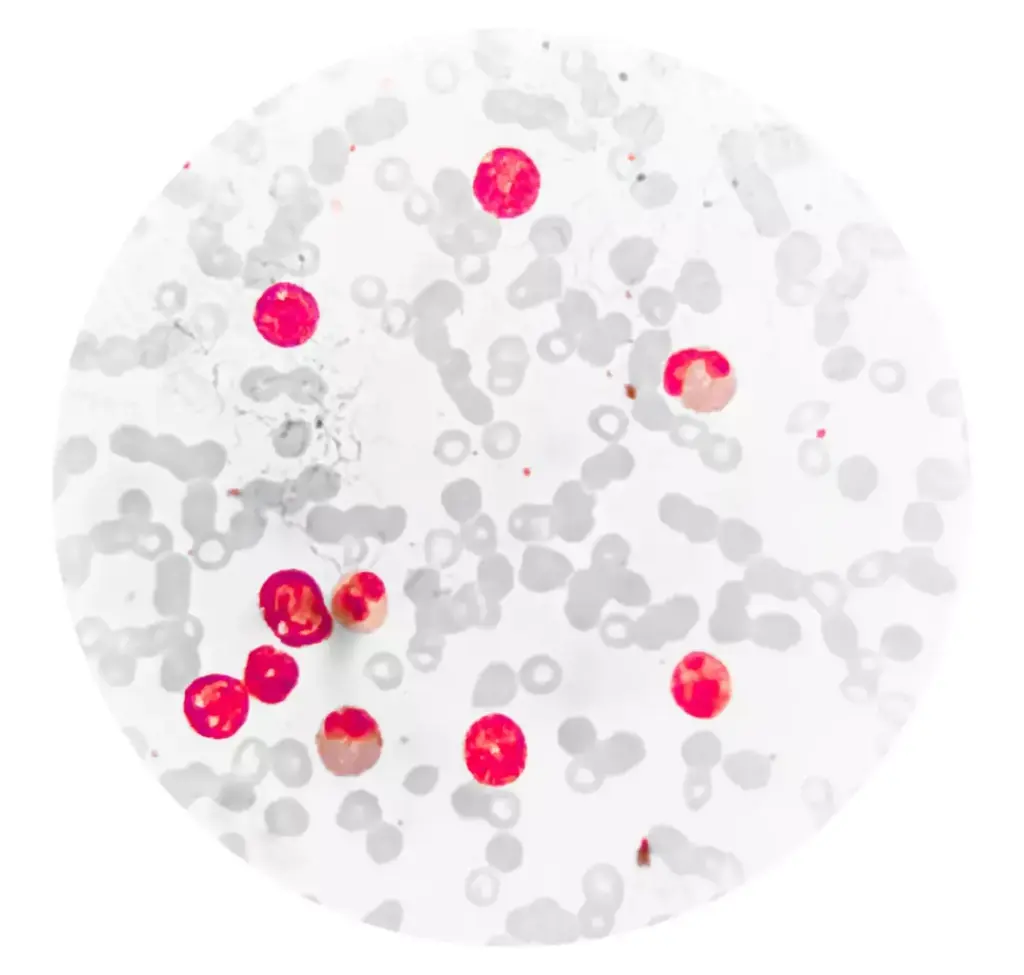
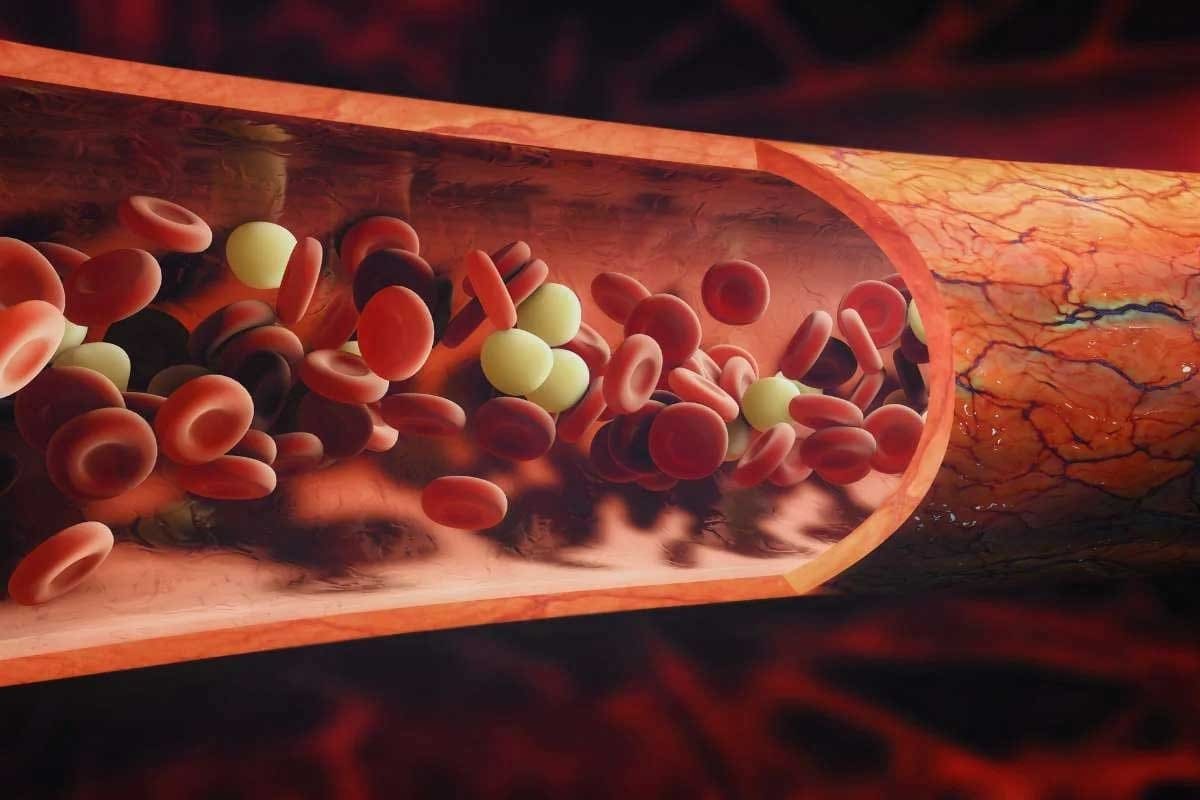
White blood cells are key to our immune system. They help fight infections. Made in the bone marrow, they move through the blood and lymphatic system. Knowing about white blood cells helps us understand how our body fights disease.
Types of White Blood Cells
There are many types of white blood cells, each with its own job. The main types are:
- Neutrophils: These cells fight bacterial infections first.
- Lymphocytes: Including B cells and T cells, they help with viral infections and more.
- Monocytes: They turn into macrophages, which clean up and digest harmful stuff.
- Eosinophils: They help with parasitic infections and allergic reactions.
- Basophils: They help with inflammation, mainly in allergic reactions.
A medical expert says, “The variety in white blood cells helps the immune system fight many pathogens.”
“The immune system’s ability to adapt to various threats is largely due to the different types of white blood cells and their specialized functions.”
Normal White Blood Cell Count Ranges
A normal white blood cell count is between 4,000 and 11,000 cells per microliter. This can change slightly based on lab standards. For those with cancer, undergoing chemotherapy, counts often drop below normal.
| Category | WBC Count (cells/μL) |
|---|---|
| Normal | 4,000 – 11,000 |
| Low (Leukopenia) | < 4,000 |
| High (Leukocytosis) | > 11,000 |
Cancer patients often have lower WBC counts during chemotherapy. This makes them more likely to get infections. Keeping an eye on white blood cell counts is important for managing chemotherapy risks.
The Relationship Between Chemotherapy and White Blood Cells

Chemotherapy is a key treatment for cancer. It affects white blood cells, making patients more likely to get infections. This is because chemotherapy lowers WBC counts.
Chemotherapy impacts the bone marrow, where white blood cells are made. The bone marrow creates all blood cells, including white blood cells. These cells fight infections.
How Chemotherapy Affects the Bone Marrow
Chemotherapy targets fast-growing cells, like cancer cells and those in the bone marrow. A document on white blood cell colony-stimulating factors explains how it can reduce white blood cell production in the bone marrow.
This reduction can cause neutropenia, where the neutrophil count drops below normal. Neutrophils are key in fighting infections.
Timeline of WBC Reduction After Chemotherapy
The time it takes for WBC counts to drop after chemotherapy varies. It depends on the type of chemotherapy and the patient’s health. Usually, WBC counts start to fall a few days after treatment.
Doctors say the risk of infection is highest when neutrophil counts are lowest. This is usually 7-14 days after chemotherapy. It’s a critical time for patients to be careful to avoid infections.
It’s important to keep an eye on white blood cell counts during this time. Regular blood tests help doctors adjust treatment plans. This ensures the patient’s care is tailored to their needs.
What Is the Minimum WBC Count for Chemotherapy?
Finding the right white blood cell (WBC) count for chemotherapy is key to keeping patients safe. Chemotherapy can hurt the bone marrow’s ability to make white blood cells. These cells are important for fighting off infections.
Before starting chemotherapy, we look at the minimum WBC counts. A count of 3,000–4,000 cells per microliter is usually safe. But, this number can change based on the treatment, the cancer type, and the patient’s health.
Standard Minimum Thresholds
Healthcare providers use guidelines to check if a patient is at risk of infection or other problems during chemotherapy. These guidelines are based on research and rules from oncology groups.
| WBC Count (cells/μL) | Interpretation |
|---|---|
| > 4,000 | Generally considered safe for chemotherapy |
| 3,000 – 4,000 | May require caution or monitoring |
| May be considered too low for chemotherapy |
Absolute Neutrophil Count (ANC) Importance
The Absolute Neutrophil Count (ANC) is a key part of the WBC count. It measures the number of neutrophils, which fight infections. An ANC of at least 1,000 cells/mm³ is needed to lower the risk of infection during chemotherapy.
“The ANC is a more specific indicator of the risk of infection than the total WBC count, as it directly measures the cells most responsible for combating bacterial infections.”
We use the ANC to decide if a patient is ready for chemotherapy. It helps us watch for neutropenia, a condition with too few neutrophils.
Knowing the minimum WBC count and ANC helps doctors make safe choices for chemotherapy. This way, we can reduce risks and get the best results for patients.
Neutropenia: When White Blood Cell Counts Fall Dangerously Low
Chemotherapy can lower your white blood cell count, leading to neutropenia. This condition has too few neutrophils. It’s a serious side effect that raises the risk of infections.
Defining Neutropenia
Neutropenia happens when your neutrophil count is too low. A normal count is between 1,500 and 8,000 cells per microliter. If it drops below 1,000, you’re at risk for infections.
Infection Risks with Low Neutrophil Counts
Neutropenia weakens your body’s defense against infections. Infections can quickly become severe and even life-threatening if not treated fast.
| ANC Level | Infection Risk | Recommended Action |
|---|---|---|
| 1,000 – 1,500 | Moderate | Monitor for signs of infection |
| 500 – 999 | High | Seek medical attention if symptoms occur |
| Below 500 | Very High | Immediate medical attention required |
It’s key to understand neutropenia and its effects during chemotherapy. Knowing the risks helps us manage patient care better. This way, we can lessen the condition’s severity.
Monitoring White Blood Cell Counts During Cancer Treatment
When you’re getting cancer treatment, like chemotherapy, it’s key to watch your white blood cell (WBC) counts. We do regular blood tests to see how your WBC counts are changing. This helps us decide if we need to change your treatment plan.
Frequency of Blood Tests
How often you get blood tests can change. It depends on your cancer type, the treatment you’re getting, and your health. Usually, we test your blood once or twice a week when you’re getting treatment. This helps us catch any big changes in your WBC counts early.
Table: Typical Blood Test Frequency During Chemotherapy
| Treatment Phase | Frequency of Blood Tests | Purpose |
|---|---|---|
| Before Chemotherapy | Once | Baseline WBC count |
| During Chemotherapy | 1-2 times a week | Monitor WBC count changes |
| After Chemotherapy | As directed by healthcare provider | Recovery monitoring |
Interpreting Your Blood Test Results
It’s important to understand your blood test results. Your healthcare team will explain them to you. But knowing what the numbers mean can help you understand your treatment better. A normal WBC count is between 4,500 and 11,000 cells per microliter. If it’s lower, you might have neutropenia, which we need to manage to avoid infections.
Talking about your blood test results with your healthcare provider is key. They can help you understand how they affect your treatment plan.
By keeping a close eye on your WBC counts and understanding your blood test results, we can manage the risks of chemotherapy. This helps us work together to get the best results for you.
When Chemotherapy May Be Delayed or Adjusted
Chemotherapy dosing is very personal in cancer treatment. It often changes based on blood counts. Deciding to delay or adjust chemotherapy is complex. It involves weighing the risks and benefits of continuing or stopping treatment.
Decision-Making Process for Treatment Continuation
Choosing to keep going with chemotherapy or to delay it is based on several key factors. These include the patient’s white blood cell count, overall health, and the type of cancer. Our medical team looks at these factors to decide what’s best for each patient.
If a patient’s white blood cell count is too low, we might delay chemotherapy. This is to avoid serious infections. But if the count is okay, treatment can go ahead as planned.
Dose Modifications Based on Blood Counts
Changing the dose of chemotherapy is common. It helps us tailor treatment to each patient’s needs. By adjusting the dose based on blood counts, we can lower the risk of bad side effects. At the same time, we keep the treatment effective.
| White Blood Cell Count | Chemotherapy Dose Adjustment | Rationale |
|---|---|---|
| Below 1,000 cells/μL | Delay treatment | High risk of infection |
| 1,000-1,500 cells/μL | Reduce dose by 25% | Moderate risk; reduce intensity |
| Above 1,500 cells/μL | Proceed with planned dose | Low risk; standard treatment |
By watching blood counts and adjusting chemotherapy doses, we offer personalized care. This care aims to balance effective cancer treatment with minimizing side effects.
Clinical Protocols to Improve WBC Count During Chemotherapy
To lower the risk of infection during chemotherapy, doctors use several methods. These strategies help keep white blood cell counts stable. This is key to supporting patients through their treatment.
Growth Factors: Filgrastim and Pegfilgrastim
Growth factors help the bone marrow make more white blood cells. Filgrastim and pegfilgrastim are two types that work well. They help prevent neutropenia and infections during chemotherapy.
- Filgrastim is given daily, starting a day or two after chemotherapy.
- Pegfilgrastim is given once per chemotherapy cycle, lasting longer.
A policy document from UHC Provider shows these growth factors are effective. They can greatly reduce neutropenia and related issues.
Antibiotic Prophylaxis and Treatment
Antibiotic prophylaxis is also important in preventing infections during chemotherapy. Antibiotic prophylaxis uses antibiotics to prevent infections in patients with low white blood cell counts.
- Doctors choose antibiotics based on the patient’s risk factors and chemotherapy type.
- The length of antibiotic use varies based on the patient’s needs and treatment.
Using growth factors and antibiotic prophylaxis together can greatly reduce infection risk. This is important for patients with low white blood cell counts during chemotherapy.
Elevated White Blood Cell Counts After Chemotherapy
Elevated white blood cell counts after chemotherapy can mean the body is recovering or facing complications. We’ll look at what causes high WBC counts after treatment. We’ll also talk about when patients should worry.
Potential Causes of High WBC After Treatment
There are many reasons why WBC counts might go up after chemotherapy. Some include:
- Infection or inflammation
- Bone marrow recovery
- Use of growth factors like filgrastim or pegfilgrastim
- Reaction to certain medications
- Underlying medical conditions
Finding out why WBC counts are high is key to proper care. We’ll cover why watching blood test results is important after chemotherapy.
When to Be Concerned About Elevated Counts
An elevated WBC count can mean recovery or a problem that needs attention. Patients should watch for symptoms like fever, chills, or signs of infection.
| Symptom | Possible Indication |
|---|---|
| Fever | Infection or inflammation |
| Chills | Severe infection |
| Swollen lymph nodes | Infection or reaction to treatment |
If you have these symptoms and a high WBC count, see your doctor right away. They can check your condition and tell you what to do next.
Knowing why WBC counts go up after chemotherapy helps patients take charge of their recovery. By working with their healthcare team, patients can manage post-chemotherapy care well. This leads to the best possible results.
Acceptable WBC Range in Cancer Patients
The white blood cell (WBC) range for cancer patients changes based on several things. These include the cancer type and the patient’s health. For adults, a normal WBC count is between 4,000 and 11,000 cells per microliter. But, for those with cancer, this range might be different.
General Guidelines for Different Cancer Types
Each cancer and treatment has its own WBC range guidelines. For example:
| Cancer Type | Acceptable WBC Range |
|---|---|
| Breast Cancer | 3,000 – 10,000 cells/μL |
| Lymphoma | 2,500 – 9,000 cells/μL |
| Leukemia | 1,500 – 8,000 cells/μL (may vary based on subtype) |
These are general guidelines. They can change based on the patient’s health, how they’re responding to treatment, and other factors.
Individual Variations in WBC Thresholds
WBC thresholds can vary from person to person. This depends on the cancer type, the patient’s health, and the treatment. For instance, some patients might be at higher risk of infections because of a lower WBC count. This could mean they need a more careful approach to treatment.
Every patient is different. What’s okay for one patient might not be the same for another. So, doctors keep a close eye on WBC counts. They adjust treatment plans to help patients get the best results.
Knowing the acceptable WBC range for cancer patients helps us manage risks better. It also improves how we care for them.
Infection Prevention Strategies During Low WBC Periods
Chemotherapy can lower white blood cell counts, making infections more likely. It’s key to take steps to prevent infections. Patients with low white blood cell counts need to be careful to avoid getting sick.
Hygiene and Dietary Precautions
Good hygiene is a must to fight off infections. Patients should wash their hands often. This is important after using the bathroom, before eating, and after coughing or sneezing. If soap and water aren’t around, hand sanitizer is a good substitute.
What you eat matters too. Avoid raw or undercooked foods like raw eggs and unpasteurized dairy. Cooking food well and handling it safely can help prevent infections.
| Hygiene Practice | Benefit |
|---|---|
| Frequent Handwashing | Reduces transmission of pathogens |
| Avoiding Close Contact with Sick Individuals | Minimizes exposure to possible infections |
| Using Hand Sanitizer | Works against many pathogens when soap and water aren’t there |
When to Seek Medical Attention
Even with precautions, knowing when to see a doctor is important. Call your healthcare provider if you have a fever over 100.4°F, chills, sore throat, or signs of infection like redness or swelling.
Key Signs to Watch For:
- Fever or chills
- Sore throat or mouth sores
- Unusual cough or shortness of breath
- Pain or burning when urinating
- Unusual vaginal discharge or itching
Being aware of these signs and acting fast can help prevent serious problems.
Conclusion: Managing Your Blood Counts Through Cancer Treatment
Managing white blood cell (WBC) counts is key to successful cancer treatment. Understanding WBC counts helps patients navigate their treatment better. We’ve talked about the importance of monitoring WBC counts, the dangers of low counts, and how to manage them.
Managing blood counts during cancer treatment is a team effort. Patients getting chemotherapy need to know about their WBC counts and the risks of neutropenia. By following the advice given, patients can lower their risk of infection and get the best results.
Guidance on managing WBC counts is vital for a successful treatment. We stress the importance of sticking to treatment plans, going for regular blood tests, and following infection prevention strategies. Working closely with healthcare providers helps patients manage their WBC counts well and achieve the best outcomes in their cancer treatment.
FAQ
What is the minimum white blood cell count required for chemotherapy?
For chemotherapy, a white blood cell count of at least 4,000 cells per microliter is safe. But, the Absolute Neutrophil Count (ANC) is also key. A count of 1,500 cells per microliter or higher is usually needed.
How does chemotherapy affect white blood cell counts?
Chemotherapy can lower white blood cell counts by affecting the bone marrow. The exact drop depends on the chemotherapy type and strength.
What is neutropenia, and how is it related to chemotherapy?
Neutropenia is when you have too few neutrophils, a type of white blood cell. Chemotherapy can cause this by reducing neutrophil production in the bone marrow. This makes you more likely to get infections.
How often should white blood cell counts be monitored during chemotherapy?
How often you get blood tests for white blood cell counts varies. It depends on your treatment and health. Usually, tests are done weekly or every two weeks to check counts and adjust treatment if needed.
What are the possible reasons for a high white blood cell count after chemotherapy?
A high white blood cell count after chemotherapy might mean your body is recovering. But, it could also mean you have an infection, inflammation, or another issue. Always talk to your doctor to find out why.
How can white blood cell counts be improved during chemotherapy?
To boost white blood cell counts during chemotherapy, growth factors like filgrastim and pegfilgrastim can help. Antibiotics and other treatments can also fight infections and support your care.
What precautions can be taken to prevent infections during periods of low white blood cell counts?
To avoid infections, practice good hygiene, eat well, and stay away from sick people. If you feel sick, see a doctor right away.
Can chemotherapy be delayed or adjusted based on white blood cell counts?
Yes, chemotherapy can be delayed or changed based on white blood cell counts. Doctors weigh the risks and benefits to decide if treatment should continue or if it needs to be adjusted.
What is the acceptable white blood cell count range for cancer patients?
For cancer patients, a white blood cell count between 4,000 and 11,000 cells per microliter is usually okay. But, this range can change based on your health and the type of cancer you have.
How are dose modifications made based on blood counts?
Dose changes are based on your white blood cell count, Absolute Neutrophil Count (ANC), and other health factors. Doctors adjust your treatment to balance its effectiveness and safety.