Last Updated on November 27, 2025 by Bilal Hasdemir

Understanding cancer diagnosis and treatment is key for patients and their families. At Liv Hospital, we make sure our patients have clear medical information. This helps them make better choices about their health.
When someone is diagnosed with cancer, they often hear about “remission” and “cure.” These terms are connected but mean different things. Remission means the cancer symptoms and signs are gone or very low. Thanks to new medical discoveries, we can now handle cancer care better.
At Liv Hospital, we aim to give top-notch healthcare to our international patients. We use the latest research, strict checks, and high ethics. This way, our patients get the best care possible.
Key Takeaways
- Cancer remission is a state where symptoms and detectable signs of the disease are reduced or absent.
- The opposite of remission is typically considered to be relapse or progression.
- Understanding the difference between remission and cure is key for patients.
- Remission does not always mean a patient is cured.
- Cancer treatment outcomes can vary a lot from one patient to another.
Understanding Cancer Remission
Remission in cancer means the disease is controlled, and symptoms are greatly reduced or gone. This is key in fighting cancer. It shows if treatment is working and gives patients hope.
Definition of Remission in Oncology
In oncology, remission means the cancer is controlled, and symptoms are less or gone. Remission can be partial or complete, based on how much the disease is reduced.
Partial remission means the cancer has shrunk or symptoms are less. But, some cancer signs are left.
Partial vs. Complete Remission
Complete remission means no cancer is found in tests. But, it’s important to remember. Even with no signs, tiny cancer cells could be there.
Here’s a table to show the difference:
| Remission Type | Description | Diagnostic Outcome |
|---|---|---|
| Partial Remission | Significant reduction in tumor size or symptoms | Some evidence of disease remains |
| Complete Remission | Cancer is no longer detectable | No evidence of disease |
Measuring Treatment Response
Testing how well treatment works includes many tests. These include CT scans, MRIs, and blood tests. New tech makes these tests better, helping doctors see if treatment is working.
Tumor markers are substances from cancer cells. Blood tests track these markers. They show if treatment is effective.
It’s important for both patients and doctors to understand cancer remission. By knowing how well treatment is working, we can make plans to get the best results.
The Opposite of Remission in Cancer
Cancer remission is a hopeful milestone, but it’s also important to know what happens when cancer returns or worsens. For many patients, the journey doesn’t end with remission. The possibility of relapse or progression is a significant concern.
Relapse: When Cancer Returns
A relapse occurs when cancer comes back after a period of remission. This can happen months or even years later. The cancer typically returns in the same area as the original tumor, but sometimes it can appear in a different part of the body.
Relapse is a significant concern because it indicates that the cancer was not completely eradicated by the initial treatment. Understanding the likelihood of relapse and the factors that contribute to it can help patients and healthcare providers make informed decisions about follow-up care.
Progression: When Cancer Worsens
Progression refers to the situation where cancer continues to grow or spread during treatment. This means that the disease is not responding to the current therapy, and the cancer is getting worse.
Progression is a critical issue because it necessitates a change in the treatment plan. Healthcare providers may need to switch to a different therapy or combination of therapies to try to control the cancer’s growth.
Distinguishing Between Relapse and Progression
While both relapse and progression indicate a problem with cancer control, they represent different scenarios. Relapse is about the return of cancer, whereas progression is about the ongoing growth or spread of the disease.
Distinguishing between the two is critical for determining the next steps in treatment. For relapse, the focus might be on re-treating the cancer with therapies that were not used initially or were not effective enough. For progression, the approach might involve changing the treatment regimen entirely.
Research has shown that early detection and treatment can improve outcomes in cases of relapse or progression. Regular follow-up and monitoring are key components of cancer care.
How Doctors Identify and Confirm Relapse
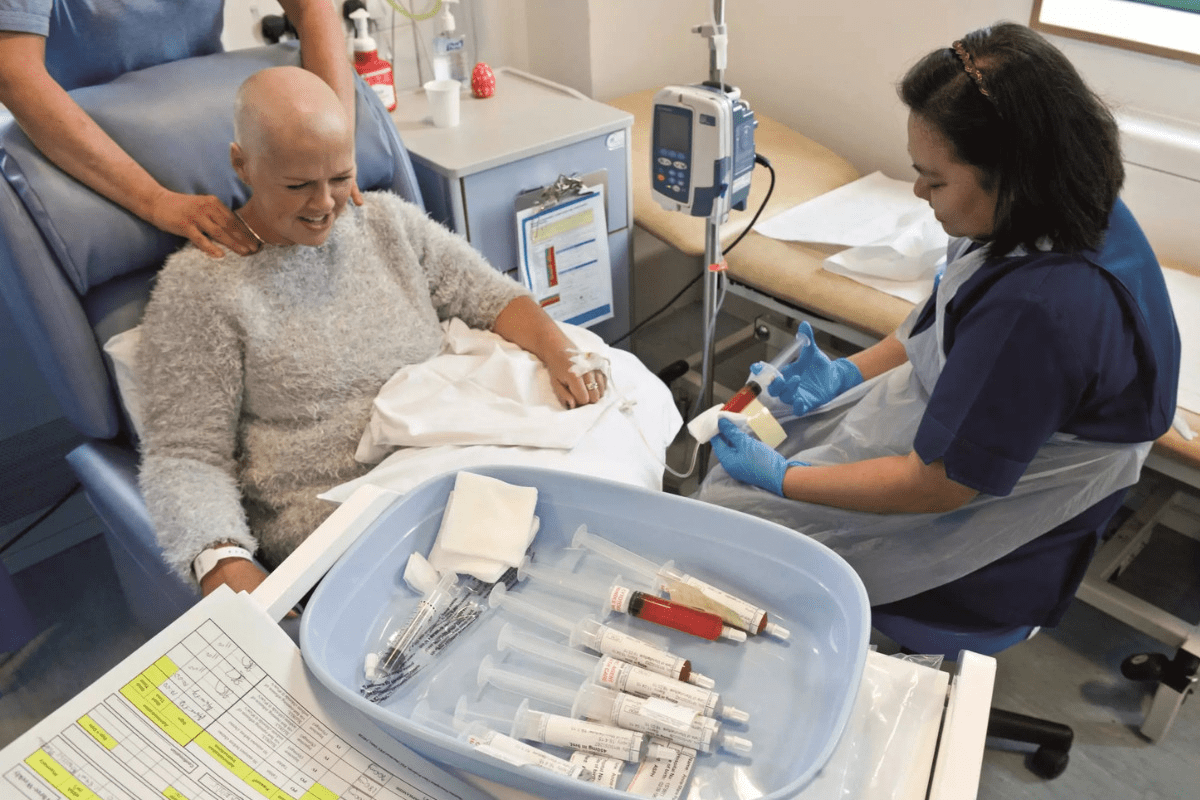
Doctors use tests and clinical checks to see if cancer has come back. Finding cancer relapse is complex. It needs a detailed approach with many diagnostic tools and checks.
Diagnostic Tests and Imaging
New imaging tech has made spotting cancer relapse easier. We use CT scans, PET scans, and MRI to find cancer again. These scans help us see even small changes in tumors.
Some important tests include:
- Computed Tomography (CT) scans
- Positron Emission Tomography (PET) scans
- Magnetic Resonance Imaging (MRI)
- Ultrasound
Clinical Signs and Symptoms
Clinical signs and symptoms are key in spotting relapse. We watch for new symptoms or worsening of old ones. What patients say is also very important.
Common signs of cancer relapse are:
- Persistent pain or discomfort
- Unexplained weight loss
- Changes in bowel or bladder habits
- New lumps or masses
Biopsy and Pathological Confirmation
Biopsy and pathological checks give clear proof of cancer coming back. We take biopsies to get tissue samples. Pathologists then check these samples to confirm cancer cells.
Timeframes and Statistics: When Relapses Typically Occur
Knowing when cancer relapses is key for patients and doctors. The time to relapse varies by cancer type and patient. We track relapse stats to guide treatment and care.
The Critical Five-Year Window
The first five years after diagnosis are vital for watching for relapse. Many cancers see their highest risk of coming back in this time. For example, breast cancer often relapses in the first two to three years.
Key statistics to consider:
- Most breast cancer relapses happen in the first five years.
- Colorectal cancer often sees its peak relapse between two to three years after surgery.
- Melanoma can have a high risk of recurrence even after five years.
Late Recurrences in Specific Cancer Types
Some cancers can come back much later than five years. Hormone-positive breast cancer and some lymphomas can recur a decade or more after treatment. We need to plan for long-term follow-up for these cancers.
Late recurrence shows the need for long-term watch for certain cancers. For example:
- Estrogen receptor-positive breast cancer can recur 15-20 years after diagnosis.
- Certain lymphomas may have a late peak in recurrence.
Risk Factors for Early Relapse
Finding out who’s at risk for early relapse helps tailor treatment. Risk factors include:
- Aggressive tumor biology.
- Incomplete surgical resection.
- Presence of metastasis at diagnosis.
- Genetic factors, such as specific mutations.
By knowing these risk factors and relapse patterns, we can make better follow-up plans. This can help improve patient outcomes.
Remission vs. Cure: Critical Distinctions
The difference between remission and cure in cancer treatment is key. It’s important for patients, families, and doctors to understand these terms. This knowledge helps in making the right treatment and care choices.
Why Doctors Rarely Use the Term “Cure”
Doctors rarely say “cure” because it’s hard to promise no return of cancer. Cancer can come back years later. This makes the term “cure” hard to use with certainty.
The idea of a “cure” is complex. Often, treatment aims to control or hide the disease. But, the chance of cancer coming back is always there. So, “remission” is used more often.
The Concept of Durable Remission
Durable remission means cancer is controlled or not found for a long time. Studies show some cancers can stay in remission for years. This gives patients a longer time without the disease getting worse.
Durable Remission: A long period where cancer is controlled.
Statistical vs. Individual Perspectives
When talking about remission and cure, both the big picture and personal experiences matter. Some cancers have higher remission rates. But, each person’s outcome depends on many things. These include the cancer type, stage, and overall health.
| Aspect | Remission | Cure |
|---|---|---|
| Definition | Cancer is under control or not detectable | Cancer will not return |
| Implication | Possibility of recurrence exists | No recurrence expected |
| Usage by Doctors | Commonly used | Rarely used due to uncertainty |
No Evidence of Disease (NED): What It Really Means
No Evidence of Disease (NED) means there’s no cancer found by today’s tests. Doctors use this term when a patient’s treatment seems to have worked.
NED as a Clinical Status
When a cancer patient reaches NED, it’s a big win. It means tests like scans and blood work show no cancer. But, it’s important to remember NED doesn’t mean the cancer is gone forever.
Patients often feel both happy and worried when they hear they’re NED. It’s a good sign, but cancer can come back. So, it’s key to keep up with check-ups and care.
“The term NED is not equivalent to being cured. It signifies that with current technology, we cannot detect cancer, but it doesn’t rule out the presence of microscopic disease.”
Limitations of Detection Methods
Today’s tests can find cancer better than before. But, they’re not perfect. Tiny cancer cells might not be caught, and cancer can come back.
| Detection Method | Limitations |
|---|---|
| Imaging Studies (CT, MRI, PET scans) | May not detect small tumors or microscopic disease |
| Blood Tests (Tumor Markers) | Can be influenced by various factors; not always specific to cancer |
| Biopsy | Invasive; sampling errors can occur |
Living with NED Status
Having NED means you need to stay active in your health care. Regular check-ups and tests are important to watch for any signs of cancer coming back.
Key aspects of living with NED include:
- Adhering to a scheduled follow-up plan
- Maintaining a healthy lifestyle
- Staying informed about the latest developments in cancer care
We help our patients make a plan for follow-ups. This way, they get the care and support they need.
Monitoring During Remission: Surveillance Protocols
Regular check-ups are key for those in remission to catch cancer signs early. This ongoing watch is vital in cancer care. It helps spot disease return quickly.
Follow-up Schedule and Tests
Having a personalized follow-up plan is essential. It includes:
- Regular physical exams
- Imaging tests like CT scans or MRIs
- Labor tests, including blood work
- Specific tests for the patient’s cancer type
How often tests are done depends on the cancer type, its stage, and treatment. For example, those with aggressive cancers might need more checks.
The Role of Tumor Markers
Tumor markers are substances found in higher amounts in some cancers. They help spot recurrence early. For example:
- Prostate-specific antigen (PSA) for prostate cancer
- Carcinoembryonic antigen (CEA) for colorectal cancer
- CA-125 for ovarian cancer
Though tumor markers are helpful, they’re not enough alone. They’re used with other tests for diagnosis.
Tailoring Surveillance to Cancer Type
Each cancer type needs its own surveillance plan. For example:
- Breast cancer might include mammograms and MRI
- Colorectal cancer could involve colonoscopies and CT scans
- Lymphoma might use PET scans and bone marrow biopsies
Customizing surveillance based on cancer type and patient needs improves care. Studies show this approach can lead to better results.
By focusing on regular checks and using various diagnostic tools, doctors can give better care to those in remission. This helps patients stay healthy for longer.
Cancer-Specific Patterns of Remission and Relapse
It’s key to understand how different cancers behave when they go into remission or come back. Each cancer type has its own way of acting, which affects how well it responds to treatment. We’ll look at these patterns in cancers like breast cancer, blood cancers, and cancers in kids.
Breast Cancer: Hormone Receptor Considerations
Breast cancer’s behavior changes based on hormone receptors. Hormone-positive breast cancer acts differently than hormone-negative. Hormone therapy is very important for hormone-positive breast cancer, helping to prevent it from coming back.
Having estrogen and progesterone receptors on cancer cells matters a lot. Studies show hormone-positive breast cancer patients live longer without the disease. But, even after a long time without cancer, it can come back. So, it’s important to keep watching for it.
Hematologic Malignancies vs. Solid Tumors
Blood cancers like leukemia and lymphoma behave differently than solid tumors. This is because of their unique biology and how they react to treatment. Chemotherapy and targeted therapies are often used, and some patients can stay in remission for a long time.
- Blood cancers can come back quickly.
- Solid tumors tend to follow a more predictable pattern of coming back.
- The treatments for blood and solid cancers are very different.
Knowing these differences helps us develop better ways to watch for cancer coming back and improve patient care.
Pediatric Cancers and Long-term Outcomes
Pediatric cancers, like leukemia and lymphoma, have their own patterns of remission and relapse. Thanks to better treatments, many kids with cancer now live longer. But, they often face health problems later in life because of their treatment.
| Cancer Type | 5-Year Survival Rate | Common Late Effects |
|---|---|---|
| Acute Lymphoblastic Leukemia | 90% | Cardiac issues, secondary cancers |
| Hodgkin Lymphoma | 85-90% | Infertility, secondary cancers |
| Neuroblastoma | 50-80% | Hearing loss, kidney damage |
It’s very important to keep up with these kids’ health long after their cancer treatment is over. This helps manage any late effects and ensures they stay healthy.
Psychological Impact of Living Between Remission and Relapse
After beating cancer, the uncertainty can deeply affect a person’s mental health. The fear of relapsing can cause a lot of stress and anxiety. This is common among many patients.
Managing Uncertainty and Scan Anxiety
Follow-up scans and check-ups can be very stressful. This stress, called “scan anxiety,” can be overwhelming for some. Healthcare providers should really help with this anxiety.
Studies show that support groups and communities can greatly help patients. They offer a sense of belonging and understanding. This can make a big difference in how patients feel.
“The fear of recurrence is a constant companion for many cancer survivors, affecting their quality of life and mental health.”
Coping Strategies for Patients and Families
It’s important for patients and their families to find ways to cope. This can include:
- Mindfulness and relaxation techniques
- Seeking support from family, friends, or support groups
- Doing things that bring joy and fulfillment
By using these strategies, patients can handle the uncertainty and anxiety better.
Support Resources and Communities
There are many resources to help cancer patients and their families. These include:
| Resource Type | Description | Benefits |
|---|---|---|
| Support Groups | Groups of people who have experienced similar challenges | Emotional support, sense of community |
| Counseling Services | Professional counseling to address mental health needs | Improved mental health, coping strategies |
| Online Communities | Online forums and social media groups for support | Accessibility, 24/7 support |
Using these resources, patients and their families can deal with the challenges of cancer remission better.
Treatment Approaches After Relapse
When cancer comes back after a break, treatment plans often change. The choice of treatment depends on many things. These include the cancer type, where it came back, past treatments, and the patient’s health.
Second-Line Therapies
Second-line therapies are used when the first treatment stops working. These can be chemotherapy, targeted therapy, immunotherapy, or hormone therapy. The choice depends on the cancer and what treatments were tried before.
Key considerations for second-line therapies include:
- The cancer’s genetic profile and any resistance to previous treatments
- The patient’s health and how well they can handle treatment
- New findings from clinical trials that might offer better options
Clinical Trial Opportunities
Clinical trials give patients access to new treatments. These trials are key for improving cancer care. They offer patients chances at treatments that might work better.
Clinical trials may involve:
- New drugs or drug combinations
- Immunotherapies that use the immune system to fight cancer
- Targeted therapies that target specific genetic mutations
Palliative Care Considerations
Palliative care helps with the symptoms and stress of serious illnesses like cancer. It’s very important, even when treatments can’t cure the cancer anymore. Palliative care teams work with oncologists to improve patients’ and families’ quality of life.
Palliative care can address:
- Pain and symptom management
- Emotional and psychological support
- Help with making decisions and planning for the future
By using second-line therapies, clinical trials, and palliative care, healthcare providers can give patients with cancer recurrence the best support.
Advances in Predicting and Preventing Relapse
Medical technology has made big strides in predicting and preventing cancer relapse. These breakthroughs are key in the fight against cancer. They bring new hope to patients and healthcare providers.
Minimal Residual Disease Testing
Minimal Residual Disease (MRD) testing is a powerful tool. It finds tiny cancer cells left after treatment. This is very important for blood cancers like leukemia and lymphoma.
MRD testing looks at blood or bone marrow for cancer markers. Tools like PCR and NGS help find these markers very well.
| MRD Testing Method | Sensitivity | Common Applications |
|---|---|---|
| PCR | High | Leukemia, Lymphoma |
| NGS | Very High | Multiple Myeloma, Leukemia |
Emerging Biomarkers and Technologies
Researchers are looking at new biomarkers and technologies. One is circulating tumor DNA (ctDNA) analysis. It finds DNA from cancer cells in the blood. This can spot relapse early.
Artificial intelligence (AI) and machine learning are also being explored. They can look at lots of data to find patterns that might mean a higher risk of relapse. This could lead to better treatment plans.
Maintenance Therapies
Maintenance therapies are now common for some cancers. They use lower doses of drugs for a long time to keep cancer away. For example, in multiple myeloma, lenalidomide helps keep the cancer from coming back.
New maintenance therapies are being developed too. These include targeted and immunotherapies. They can be made just for the patient’s cancer type. You can learn more about this in our article on whether chemotherapy kills cancer stem cells.
By using MRD testing, new biomarkers, and maintenance therapies, we’re getting closer to stopping cancer relapse. This is a big step towards a better future in cancer treatment.
Conclusion: Navigating the Cancer Journey Beyond Remission
Navigating the cancer journey beyond remission needs ongoing care and support. Remission, relapse, and cure are complex ideas that affect patients and their families. It’s key to understand these concepts well.
Studies show that good care and support lead to better outcomes. We aim to offer top-notch healthcare and support. This helps patients deal with the ups and downs of their journey.
It’s vital for patients to stay informed and involved in their care. This way, they can manage their remission better and increase their chances of beating cancer long-term. We’re here to support patients every step of the way, providing the resources and care they need to thrive.
FAQ
What is the opposite of remission in cancer?
The opposite of remission in cancer is relapse or progression. This means the disease is coming back or getting worse.
What is the difference between partial and complete remission?
Partial remission means symptoms are greatly reduced. Complete remission means the disease is gone.
How is treatment response measured in cancer patients?
Treatment response is measured with tests like imaging studies and tumor marker assessments.
What is the difference between relapse and progression?
Relapse is when cancer comes back after a break. Progression is when the disease gets worse.
How is cancer relapse diagnosed?
Diagnosing relapse involves tests, clinical checks, and sometimes a biopsy.
What is No Evidence of Disease (NED) status?
NED status means tests show no cancer. But it doesn’t mean the cancer is cured for sure.
Is being in remission the same as being cured?
No, being in remission and being cured are different. Remission means symptoms are gone or reduced. Cure means the cancer won’t come back.
What is durable remission?
Durable remission means cancer control lasts a long time. It shows the disease is controlled for a long period.
How often should patients have follow-up care during remission?
Patients should have regular check-ups. This includes tests and assessments to watch for recurrence.
What is the role of tumor markers in detecting relapse?
Tumor markers are key in spotting relapse. They watch for changes in proteins or genes linked to cancer.
What are the psychological impacts of living with cancer remission and the risk of relapse?
Living with remission and the risk of relapse affects the mind. It can cause anxiety, uncertainty, and fear of recurrence.
What treatment approaches are available after cancer relapse?
After relapse, treatments include second-line therapies and clinical trials. Palliative care is also considered.
What advances are being made in predicting and preventing cancer relapse?
New tech like minimal residual disease testing and biomarkers are being explored. They aim to predict and prevent relapse.
References
- MyPathologyReport. What is negative for malignancy? https://www.mypathologyreport.ca/pathology-dictionary/negative-for-malignancy/
- Wikipedia. Malignancy https://en.wikipedia.org/wiki/Malignancy
- SEER Training. Introduction to the SEER Training Website https://www.training.seer.cancer.gov/help/
- MD Anderson. Remission, cancer‑free, no evidence of disease: What’s the difference? https://www.mdanderson.org/cancerwise/remission–cancer-free–no-evidence-of-disease–what-is-the-difference-when-talking-about-cancer-treatment-effectiveness-and-results.h00-159460845.html
- National Center for Biotechnology Information (NCBI). In the NCBI Bookshelf: NBK82165 https://www.ncbi.nlm.nih.gov/books/NBK82165/