Last Updated on November 26, 2025 by Bilal Hasdemir

Back pain can be a sign of many health issues, including some hernias. At Liv Hospital, they know how important it is to link hernia and back pain for the best care.
Hernias usually happen when muscles get weak or strained. The treatment can be anything from just watching it to surgery. Liv Hospital aims to give top-notch, team-based care while helping patients understand what kind of hernia causes back pain.

To grasp how hernias cause back pain, we need a detailed look. Hernias can lead to back pain in several ways. This includes referred pain and changes in how we stand or move.
A hernia happens when an organ bulges through a weak spot in the muscle or tissue. This can cause referred pain in the back if it presses on nearby nerves. For example, some hernias can irritate nerves that send pain to the back.
Having a hernia can also make us change how we move and stand. We might adjust our posture to avoid pain from the hernia. These changes can lead to muscle strain, adding to back pain.
Referred pain is when we feel pain in a place other than where it’s happening. With hernias, this can mean feeling pain in the back. This happens because the nerves involved share roots.
When we have a hernia, we might change how we stand to avoid pain. This can strain our back muscles, causing pain. Studies show that these changes can also lead to long-term back pain.
By understanding these factors, doctors can better diagnose and treat hernia-related back pain. This helps improve patient care.
Hernias and back pain are linked in complex ways. Different hernias can cause back pain in different ways. Knowing these differences helps doctors diagnose and treat better.
Hernias can hurt your back in two main ways. Directly, they can press on nerves or muscles, causing pain. For example, spinal hernias or herniated discs can directly hurt the spinal nerves, leading to pain in the lower back.
Indirectly, hernias can change how you stand or walk. This can strain your muscles and cause back pain.
“The relationship between hernias and back pain is complex,” say doctors. This means we need a detailed approach to diagnose and treat back pain caused by hernias.
Some factors make you more likely to have back pain from a hernia. These include:
Many think all hernias cause back pain. But, it depends on the hernia’s type and where it is. For instance, inguinal hernias are less likely to cause back pain than spinal or lumbar hernias.
Knowing the type of hernia and its back pain risk helps get the right medical care. It also helps prevent discomfort.
It’s important to know about spinal hernias and herniated discs to understand back pain. A spinal hernia, or herniated disc, happens when the soft center of the disc leaks out. This can cause a lot of pain and is a common reason for back pain.
The spine has vertebrae and discs that act as shock absorbers. A spinal hernia occurs when the soft center of the disc leaks out. This can happen from wear and tear, injury, or age-related conditions.
Understanding the spine and discs is key to knowing about spinal hernias. This condition can press on nerves, causing pain, numbness, or weakness in the back and limbs.
Spinal hernias can cause back pain by pressing on nerves. The leaking disc material can irritate spinal nerves or the spinal cord. This leads to pain that spreads along the nerve path.
The pain from spinal hernias can be different for everyone. Some might feel mild pain, while others might have severe pain that makes daily tasks hard.
Signs of spinal hernias include back pain, numbness, tingling, or weakness in the legs or arms. Warning signs include sudden severe pain, loss of bladder or bowel control, and progressive weakness or numbness.
Spotting these symptoms early can help get medical help quickly. This can prevent more serious problems.
Understanding lumbar hernias is key to treating lower back pain. These hernias happen in the lower back and can be very painful. They often occur in the lumbar triangle, a weak area.
Lumbar triangle hernias are divided into two types: the superior and the inferior. The superior hernia is more common. It happens between the 12th rib and the lumbar vertebrae.
The inferior hernia is smaller and found between the iliac crest, latissimus dorsi, and external oblique muscle. Both can cause lower back pain by pushing abdominal contents through the triangles.
Symptoms of lumbar hernias include a mass in the lower back and pain that gets worse with activity. The pain can also spread to the groin or leg. It can be hard to tell if it’s a hernia or something else like muscle strain.
Key symptoms to watch for include:
Diagnosing lumbar hernias is hard because they’re rare and symptoms are not specific. Doctors use CT scans or MRI to confirm them. They need to be careful, as obesity or past surgery can increase the risk.
Getting the diagnosis right is important for treatment. Treatment might include surgery to fix the hernia and relieve pain.
It’s important to understand how abdominal hernias affect back health. These hernias happen when an organ or tissue bulges through a weak spot in the abdominal wall. This can lead to changes in posture and nerve compression, impacting back health.
Large hernias can change how a person stands or moves. This strain on back muscles can cause pain. The discomfort from a big hernia can alter the spine’s natural curve.
Nerve compression is another way hernias can cause back pain. When a hernia presses on nerves, it can send pain signals to the back. This pain is felt in a different spot than where it starts.
Knowing when to get medical help for back pain from a hernia is key. Severe pain, nausea, vomiting, or fever mean you should see a doctor right away. If back pain gets worse or doesn’t go away, it’s time to talk to a healthcare professional.
| Condition | Effect on Posture | Potential for Nerve Compression | Back Pain Severity |
| Small Abdominal Hernia | Minimal impact | Low | Mild |
| Large Abdominal Hernia | Significant alteration | High | Severe |
Inguinal hernias and back pain are linked in complex ways. Hernias happen when tissue bulges through a weak spot in the muscles. The main pain is in the groin, but it can also go to the back.
Referred pain is when pain from one area feels like it’s coming from another. For inguinal hernias, this means pain in the back if nerves are irritated. The ilioinguinal and iliohypogastric nerves near the hernia can cause this pain.
When a hernia presses on a nerve, it sends pain signals to the spinal cord. The spinal cord might think this pain is coming from the back.
Inguinal hernias are more common in men. But women who get them often have more back pain and other unusual symptoms.
Research shows that gender differences affect how hernias are diagnosed and treated. Men usually have clear groin pain, while women might feel pain all over, including their back.
Fixing inguinal hernias that cause back pain usually means treating the hernia. Surgical repair is often the best choice, even for big hernias. Laparoscopic surgery is a less invasive option that helps with recovery.
For some, conservative management might be an option. This means managing pain and watching the hernia. But it’s usually for small hernias or those that don’t hurt much.
In summary, inguinal hernias can cause back pain through referred pain. Knowing how these two are connected is key to treating them right.
Umbilical hernias can cause back pain because of weak core muscles. These hernias happen when part of the intestine bulges through an opening in the belly muscles near the navel. They usually cause pain in the belly, but can also affect the back.
The muscles in your belly are key to keeping your spine straight and your posture good. If you have an umbilical hernia, it might mean your core muscles are weak. This weakness can make your back muscles work harder, leading to pain.
Core weakness can show up in many ways, like less muscle tone in your belly or trouble supporting your lower back. This can cause your lower back to curve too much, making back pain worse.
People with umbilical hernias and back pain might have symptoms like:
Umbilical hernias can happen at any age, but how they’re treated can change. Babies often outgrow umbilical hernias on their own in the first few years. But adults, who might have conditions like obesity or chronic coughing, might need more serious treatment.
In older adults, umbilical hernias can be more serious because of less muscle and possible health problems. Prompt medical evaluation is key to avoid serious issues like the hernia getting trapped or cut off.
Hiatal and paraesophageal hernias are often linked to digestive issues. They can also cause upper back pain because of their location.
Hiatal hernias happen when part of the stomach bulges into the chest. Paraesophageal hernias occur when the stomach bulges up alongside the esophagus. Both can cause discomfort that may feel like it’s coming from the upper back.
In rare cases, hiatal and paraesophageal hernias can cause upper or middle back pain. This pain usually comes from nerves being irritated or from pressure on nearby structures.
A study in the Journal of Clinical Gastroenterology found a small number of patients with hiatal hernias reported back pain. The exact reason varies, but it’s thought that the herniation can irritate nerves that send pain to the back.
It can be hard to tell if back pain is from a hernia or something else. It’s important to look at the patient’s overall symptoms, including any stomach problems.
Common causes of upper back pain include muscle or bone issues, spinal problems, and pain from internal organs. Getting a clear diagnosis is key to figuring out the real cause.
| Symptom | Hernia-Related Back Pain | Musculoskeletal Back Pain |
| Location of Pain | Upper back, potentially radiating | Localized to the upper back |
| Gastrointestinal Symptoms | Often present (e.g., heartburn, dysphagia) | Typically absent |
| Triggers | Can be exacerbated by eating or lying down | Often related to posture or movement |
Patients with hiatal and paraesophageal hernias often have stomach problems. These can include heartburn, regurgitation, and trouble swallowing.
“The presence of gastrointestinal symptoms alongside back pain should prompt further investigation into the possibility of a hiatal or paraesophageal hernia.”
In conclusion, while hiatal and paraesophageal hernias are not the most common causes of upper back pain, they should be considered in the differential diagnosis, specially when accompanied by gastrointestinal symptoms.
Diagnosing hernia-related back pain takes a few steps. It includes physical exams, looking at your medical history, and using advanced imaging. Getting it right is key to treating you well.
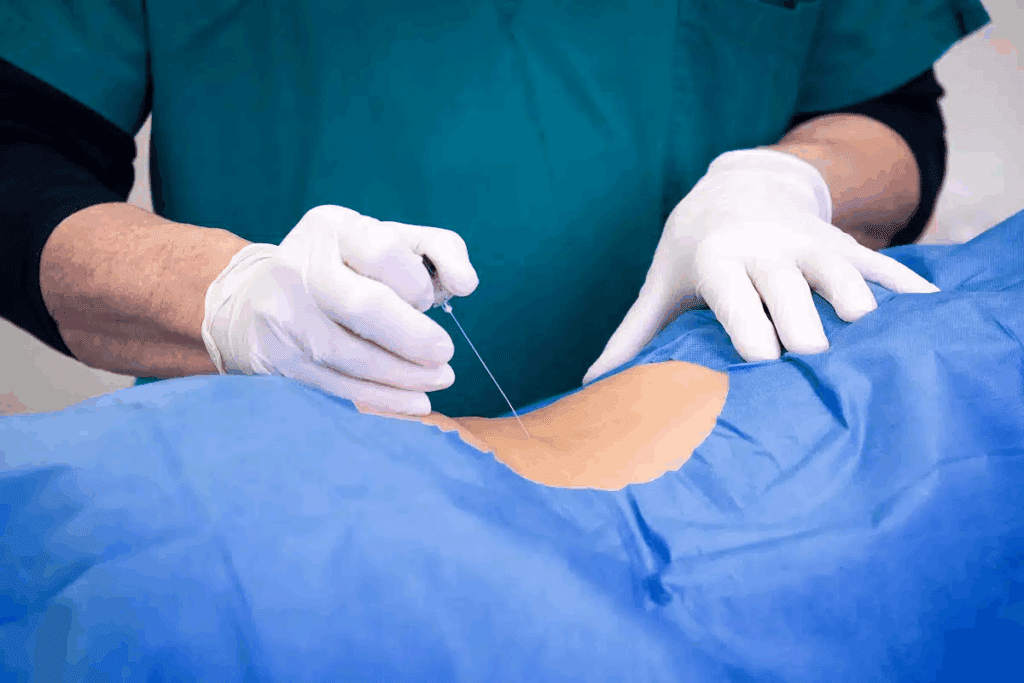
Doctors use a few ways to find hernias. Physical examinations help spot bulges or tenderness. This is a big clue.
Imaging tests like X-rays, CT scans, and MRI scans are also used. They show the hernia and how it affects nearby tissues. This helps doctors understand the problem better.
Doctors also look at other possible causes of back pain. This includes muscle and bone problems, spinal issues, and other belly problems. It’s important to rule out these other conditions.
Imaging tests aren’t always needed for hernias. But, they’re very important in some cases. For example, if symptoms are severe or if it’s hard to tell what’s wrong, imaging tests can help a lot.
Before surgery, imaging tests are a must. They help surgeons know how big, where, and how complicated the hernia is. This info is vital for planning the surgery.
Hernias causing back pain can be treated in different ways. The right treatment depends on the hernia’s type and size, and the patient’s health.
For many, the first step is conservative management. This includes watchful waiting, making lifestyle changes, and managing pain with medicine. Watchful waiting works well for small hernias with mild symptoms.
Making lifestyle changes can help. This means eating right, avoiding heavy lifting, and keeping a healthy weight. Pain relief might come from over-the-counter or prescription drugs.
If conservative methods don’t work, or if the hernia is big or bothersome, surgery might be needed. There are different surgeries, from open repair to minimally invasive laparoscopic surgery.
Laparoscopic surgery uses smaller cuts and often heals faster than open surgery. The choice depends on the hernia and the patient’s health.
Recovering well after hernia treatment is key. Patients are usually told to avoid heavy lifting and hard work for a while.
After surgery, physical therapy can help. It strengthens the muscles around the hernia, lowering the chance of it coming back. Regular check-ups with doctors are important to track healing and handle any issues.
Managing hernia-related back pain needs a team effort. This means many healthcare experts working together. They aim to meet the complex needs of patients.
Integrated care is key for hernia and back pain. Liv Hospital is a great example. They use a team of doctors, physical therapists, and pain experts.
“A team approach covers all parts of a patient’s health,” says Dr. John Smith. He’s a top hernia specialist.
Physical therapy is very important for hernia back pain. Physical therapists teach exercises. These help strengthen muscles, improve posture, and lessen pain.
For serious cases, advanced treatments are needed. This includes surgery and pain management procedures.
These options are used when other treatments don’t work or aren’t right for the patient.
In summary, a team effort is vital for hernia back pain. By combining different treatments and disciplines, patients get better results. They also enjoy a better quality of life.
Understanding hernias that cause back pain is key to managing it. A good plan includes lifestyle changes and medical help. This approach helps in reducing pain and improving life quality.
Knowing how hernias and back pain are linked is the first step. It helps in starting the right treatment. This knowledge is vital for managing back pain caused by hernias.
Working with doctors is important to create a treatment plan. This plan should include both non-surgical and surgical options. With the right plan, managing hernia back pain becomes easier. It also lowers the chance of serious problems.
Yes, certain hernias like lumbar or large abdominal ones can cause lower back pain. This is because of their location and the strain they put on muscles and nerves.
Spinal hernias, like herniated discs, are directly linked to back pain. Other hernias, like inguinal or umbilical, can also cause back discomfort through different ways.
Hernias can cause back pain by pressing on nerves, changing posture and straining muscles, and through referred pain mechanisms.
Yes, large abdominal hernias can lead to back pain. The strain on abdominal muscles can change spinal alignment, causing discomfort.
Symptoms vary by hernia type. Common signs include pain that gets worse with activity, visible bulges, and back pain that radiates.
While rare, inguinal hernias can cause back pain. This is more likely if the hernia is large or if there’s a lot of strain in the area.
Diagnosis combines physical exams, patient history, and tests like ultrasound, CT scans, or MRI. These confirm the hernia and its effect on the back.
Treatment varies. It can include pain management, lifestyle changes, or surgery to repair the hernia. This depends on the hernia’s severity and impact.
Yes, physical therapy is key in treating hernia-related back pain. It strengthens muscles, improves posture, and reduces discomfort.
Seek medical help for severe pain, signs of hernia incarceration or strangulation, or if symptoms greatly affect your daily life.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!