Last Updated on December 3, 2025 by
How long for platelets to increase after chemo? Find out what level of platelets is dangerous and the timeline for a crucial, powerful recovery.
Chemotherapy is a common treatment for many cancers. It often causes a drop in platelet count. Knowing how long it takes for platelet recovery is key to good patient care.
About 2 to 3 weeks after chemo, platelets start to go up. But how fast they recover can change a lot. It depends on the cancer type, the patient’s age, and the chemo used.
It’s important to know the signs of low platelet cancer symptoms and low platelet count cancer symptoms. Patients should watch for these signs to get help quickly.
Key Takeaways
- Platelet count usually starts to recover 2 to 3 weeks after chemo.
- The recovery speed can change based on cancer type, patient age, and chemo.
- Knowing low pplateletcancer sysymptomsnd low platelet count cancer symptoms is key ftopatient care.
- Keeping an eye on chemo and low blood platelets is vital for managing patient outcomes.
- Recovery times can vary a lot among patients getting chemo.
Understanding Platelets and Their Function
Platelets, also known as thrombocytes, are vital for blood clotting. They help keep us from bleeding too much. These cells are made in the bone marrow and are always ready to help when needed.
What Are Platelets?
Platelets are small, irregularly shaped blood cells. They are key to stopping bleeding. When we get hurt, platelets form a plug to seal the wound. Then, a coagulation cascade makes the clot stronger.

Normal Platelet Count Range
A normal platelet count is between 150,000 and 450,000 per microliter of blood. If this range is not met, it could mean health problems. For example, too few platelets can lead to easy bleeding. Too many might cause clots to form more easily.
The Role of Platelets in the Body
Platelets stop us from bleeding too much when a blood vessel gis damaged They stick to the injury, gather together, and send out signals. These signals bring more platelets and start the clotting process. Platelets also help with inflammation and healing.
In cancer patients, like those with leukemia, platelet counts can be greatly affected. This is due to the disease itself and treatments like chemotherapy. Knowing about platelet function and counts is key to their care.
How Chemotherapy Affects Blood Cells
Chemotherapy targets fast-growing cancer cells. But it also affects other fast-growing cells, like those in the bone marrow. This is where blood cells are made.
Impact on Bone Marrow
The bone marrow is inside some bones, like hthe ips and the thighbones. It makes blood cells. Chemotherapy can make it hard for the bone marrow to make these cells.
This leads to myelosuppression. It affects platelets, white blood cells, and red blood cells. Patients then face more infections, anemia, and bleeding.
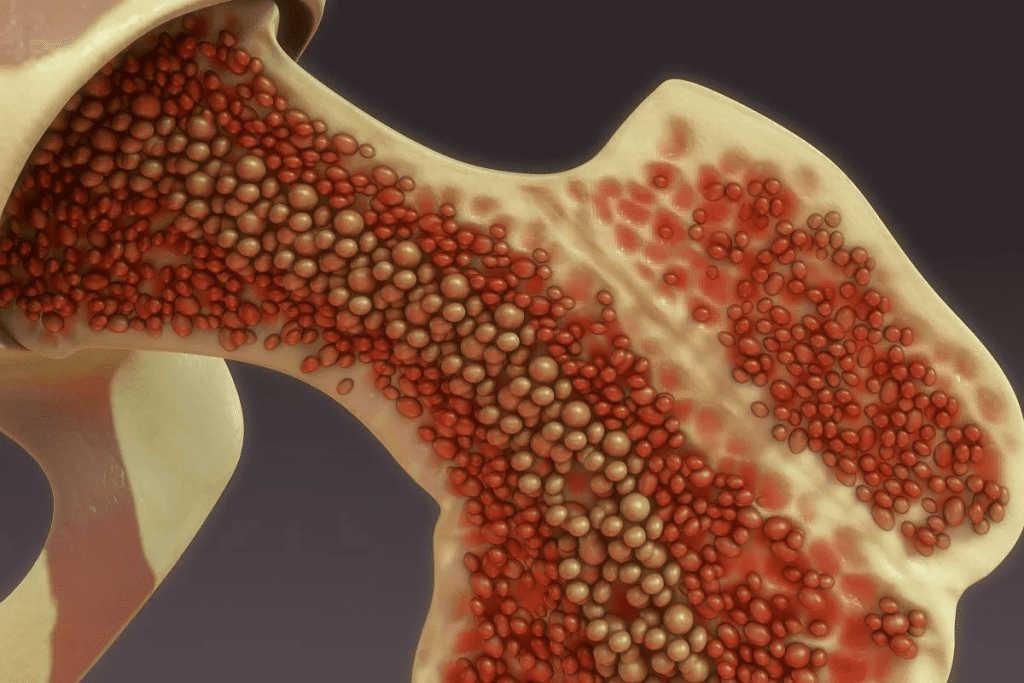
Myelosuppression Explained
Myelosuppression is a common side effect of chemotherapy. It means the bone marrow makes fewer blood cells. This can cause thrombocytopenia, or low platelet count, which raises the risk of bleeding.
The severity of myelosuppression depends on the chemotherapy type and dose.
Why Platelets Are Particularly Vulnerable
Platelets are short-lived in the blood, lasting about 7 to 10 days. Chemotherapy can quickly lower their count. This is because it reduces new platelet production.
Most patients see their platelet nadir (lowest level) 7-14 days after treatment. This is a critical time for monitoring and managing bleeding risks.
Knowing how chemotherapy affects platelet counts is key. It helps manage the risks of low platelet counts, or thrombocytopenia. Recognizing signs and knowing when to seek medical help is important for patients going through cancer treatment.
Recognizing Low Platelet Count Symptoms
Low platelet count, or thrombocytopenia, can show in many ways. It’s key to watch platelet levels during cancer treatment, like chemotherapy. This is because treatments can weaken the bone marrow.
Low Platelets Cancer Symptoms
Cancer patients with low platelets might see different symptoms. Easy bruising and petechiae (small red or purple spots on the skin) happen because the body can’t clot blood well. They might also notice prolonged bleeding from small cuts or injuries.
Early Warning Signs
Spotting low platelet count symptoms early is important. Some early signs include:
- Nosebleeds or bleeding gums
- Fatigue or weakness
- Blood in urine or stool
- Heavy menstrual periods
These signs mean platelet counts might be low. It’s important to tell doctors right away.
Severe Manifestations
Thrombocytopenia can get worse and cause serious problems. Severe bleeding is a big risk and can be deadly if not treated quickly. Signs of severe bleeding include:
- Large bruises or hematomas
- Severe headache or confusion (indicating possible intracranial bleeding)
- Abdominal pain or vomiting blood
Patients should get help right away if they see these serious signs.
What Level of Platelets is Dangerous?
Understanding what level of platelets is dangerous is critical. Low platelet counts are very dangerous, even more so for those getting chemotherapy. Platelets help blood clot, and without enough, serious bleeding can happen.
Critical Platelet Level Thresholds
Platelet counts are measured in units per microliter of blood. A count under 150,000/μL is low (thrombocytopenia). But the risk of bleeding grows as the count goes lower.
Critical thresholds include:
- Below 50,000/μL: Moderate risk of bleeding, mainly with trauma or surgery.
- Below 20,000/μL: High risk of spontaneous bleeding.
- Below 10,000/μL: Very high risk of severe, life-threatening bleeding.
Is 70 a Low Platelet Count?
A platelet count of 70,000/μL is low. It’s not extremely low, but it’s risky, mainly for those on chemotherapy or with health issues.
Bleeding Risk Assessment
Assessing bleeding risk involves more than just platelet count. It also looks at overall health, other medical conditions, and the chemotherapy used.
Bleeding risk factors include:
- Low platelet count.
- Recent trauma or surgery.
- Use of anticoagulant medications.
When Medical Intervention Becomes Necessary
Medical help is needed when platelet counts are too low or when there’s significant bleeding. This might include platelet transfusions, adjusting chemotherapy, or other care.
Signs that medical intervention is necessary:
- Visible bleeding that doesn’t stop.
- Severe bruising or petechiae.
- Bleeding gums or nosebleeds.
The Timeline of Platelet Decrease After Chemotherapy
Knowing when platelet counts drop after chemo is key to patient care. Chemo hits not just cancer cells but also fast-growing cells in the bone marrow. These cells help make platelets.
The drop in platelet count after chemo follows a pattern. This pattern can be divided into different stages.
Initial Impact Phase (Days 1-7)
In the first days after chemo, the bone marrow’s platelet-making ability starts to slow down. Patients may see their platelet count drop just a few days after treatment.
Nadir Period (Days 7-14)
The nadir period is when platelet counts hit their lowest, usually between 7 to 14 days after chemo. Most patients see their platelet nadir around this time. It’s a key time for watching for bleeding risks.
Monitoring Protocols During Treatment
Keeping an eye on platelet counts during chemo is vital. Regular blood tests help doctors spot low platelet counts early. This helps them decide if a patient needs platelet transfusions or changes to their chemo plan.
Understanding when platelet counts drop after chemo helps doctors manage patient care better. This reduces the risks of low platelet counts.
Typical Platelet Recovery Timeline After Chemotherapy
Chemotherapy can lower platelet counts. Knowing how long it takes to recover is important for patients and doctors. Platelets usually start to go up 2 to 3 weeks after treatment, taking about 25 days on average.
Early Recovery Phase (2-3 Weeks Post-Treatment)
In the first 2 to 3 weeks after chemotherapy, the body starts to make more platelets. This is a key time to see how well the bone marrow is working. It’s important to check platelet counts during this time to see if treatment is working and to catch any problems early.
Complete Recovery Period (Average 25 Days)
It usually takes about 25 days for platelets to fully recover after chemotherapy. But, this can change a lot depending on the cancer type, treatment, and overall health. Knowing these things can help plan treatment better and make decisions.
Variation in Recovery Times (12-52 Days)
Recovery times can vary a lot, from 12 to 52 days. This shows how important it is to get care that fits each person and to keep checking platelet counts. How fast someone recovers can depend on how strong the treatment was and how much bone marrow they have.
Chemo and Low Blood Platelets: Recovery Patterns
People with low blood platelets after chemotherapy can recover at different rates. Some might get better fast, while others might take longer. Figuring out why platelets are low and adjusting treatment can help speed up recovery.
Factors Affecting Platelet Recovery Rate
The speed of platelet recovery after chemotherapy depends on several key factors. Knowing these elements is vital for managing expectations and improving care during recovery.
Cancer Type and Stage
The type and stage of cancer greatly affect platelet recovery rates. Patients with advanced cancer or aggressive cancer types may face slower recovery. This is because they need more intense treatments ,and their disease is harder to fight.
Patient Age and Overall Health
Patient age and overall health are key in determining platelet recovery speed. Older patients or those with health issues may recover smore slowly This is because their bone marrow is less strong and their body are less resilient.
Chemotherapy Regimen and Dosage
The chemotherapy regimen and dosage are very important for platelet recovery. More intense chemotherapy can cause longer periods of low platelets. This means doctors need to watch patients closely and might need to change treatment plans.
Previous Treatments and Cumulative Effects
Previous treatments, like chemotherapy and radiation, can harm the bone marrow. This affects platelet production. Patients who have had many treatments may recover more slowly because their bone marrow is weaker.
In summary, platelet recovery after chemotherapy is influenced by many factors. These include cancer type, patient age, chemotherapy, and previous treatments. Understanding these can help doctors tailor care to each patient. This can lead to better outcomes.
Clinical Significance of Platelet Recovery Timing
The timing of platelet recovery after chemotherapy is key to patient outcomes. Studies show early platelet recovery links to better survival and treatment success in leukemia patients.
Early Recovery as a Positive Prognostic Indicator
Early platelet count recovery after chemotherapy is a good sign. Research shows patients with quicker recovery have better survival rates and treatment outcomes. This suggests the bone marrow is responding well to treatment.
“The rate of platelet recovery is a significant predictor of patient outcomes in leukemia treatment.” –
A renowned hematologist
Implications of Delayed Recovery (Beyond 26 Days)
Delayed platelet recovery, over 26 days, may signal complications or severe chemotherapy effects. Such delays raise the risk of bleeding and may require platelet transfusions. It’s vital to closely watch platelet counts during and after chemotherapy.
Correlation With Treatment Outcomes
The link between platelet recovery timing and treatment success is a major focus. Research indicates quicker platelet recovery is tied to better outcomes, like higher remission rates and longer survival. This shows platelet count’s role as a prognostic marker in leukemia and cancer treatment.
In summary, platelet recovery timing after chemotherapy is critical for patient prognosis and treatment outcomes. Early recovery is linked to better survival, while delayed recovery may signal complications. This highlights the need for careful monitoring and management of platelet counts during cancer treatment.
Interventions to Support Platelet Recovery
To help platelets recover after chemotherapy, several steps can be taken. These steps are key to managing low platelet counts and ensuring treatment success.
Growth Factors and Their Effectiveness
Growth factors, like thrombopoietin receptor agonists, boost platelet production. They help megakaryocytes, the bone marrow cells that make platelets, grow and mature. This can shorten the time of low platelet counts, lowering bleeding risks.
Platelet Transfusions: When They’re Needed
Platelet transfusions are vital for patients with very low platelet counts. They are usually given when counts drop below 10,000/ µL or if there’s active bleeding. The choice to give platelets depends on the patient’s health and bleeding risk.
What is the Minimum WBC Count for Chemotherapy?
The minimum white blood cell (WBC) count for chemotherapy varies. It depends on the treatment and the patient’s health. Generally, a WBC count of 1,500-3,000 cells/ µL is needed. But this can change based on the chemotherapy type and the patient’s health.
Supportive Care Strategies
Supportive care is important for managing chemotherapy side effects, like low platelets. It includes eating foods high in antioxidants and fiber and making lifestyle changes to lower bleeding risks. Doctors may also prescribe medications to help with platelet production or bleeding control.
By using these interventions, healthcare providers can help platelet recovery in chemotherapy patients. This makes cancer treatment safer and more effective.
Managing Low Platelet Counts During Cancer Treatment
Managing low platelet counts is key for cancer patients. Low platelet counts, or thrombocytopenia, raise the risk of bleeding and bruising. It’s vital to manage this to keep patients safe and well.
Lifestyle Adjustments to Reduce Bleeding Risk
Patients with low platelet counts need to make lifestyle changes. They should avoid activities that might cause injury, like contact sports or heavy lifting. Using a soft-bristled toothbrush and avoiding dental procedures without a doctor’s okay can also help.
They should also be careful with sharp objects and avoid cutting themselves. Using electric razors instead of razors with blades can reduce the risk of cuts.
Dietary Considerations
Eating a balanced diet rich in nutrients can help platelet production. Foods high in vitamin K, like leafy greens, help with blood clotting. Increasing foods rich in antioxidants, such as berries and nuts, is also good.
Drinking plenty of fluids is important. Avoiding alcohol and caffeine, which can act as diuretics, is recommended.
Activity Modifications and Precautions
Changing daily activities can prevent injuries and bleeding. Patients should avoid heavy lifting, bending, or strenuous exercises. Engaging in gentle exercises, such as yoga or short walks, is safer.
LIV Hospital’s Evidence-Based Protocols
LIV Hospital follows global standards in patient care, using evidence-based protocols. For managing low platelet counts, they use a team approach with hematologists, oncologists, and nutritionists. Their protocols are tailored to each patient’s needs and treatment plan.
By using these protocols, patients at LIV Hospital get care that meets their unique needs. This helps minimize the risks of low platelet counts.
Conclusion
It’s important for cancer patients and doctors to understand how chemotherapy affects platelet counts. Platelet recovery is key in cancer treatment. It helps prevent bleeding and improves treatment success.
The time it takes for platelets to recover after chemotherapy varies. This depends on the cancer type, stage, patient’s age, and the chemotherapy used. Using growth factors and supportive care helps manage platelet issues and aids in recovery.
Healthcare providers can improve treatment results by focusing on platelet recovery. They can use the right strategies to manage low platelet counts. This ensures the best outcomes for patients going through chemotherapy and cancer treatment.
FAQ
What is a normal platelet count range?
A normal platelet count is between 150,000 to 450,000 platelets per microliter of blood.
Is 70 a low platelet count?
Yes, a platelet count of 70 is low. Normal counts are 150,000 to 450,000 per microliter.
What is the minimum WBC count for chemotherapy?
The minimum WBC count for chemotherapy varies. It depends on the treatment and the patient’s health. Usually, it’s 1,500 to 3,000 cells per microliter.
How long does it take for platelets to recover after chemotherapy?
Platelets start to increase 2 to 3 weeks after chemotherapy. Recovery takes about 25 days, but it can range from 12 to 52 days.
What are the symptoms of low platelet count during cancer treatment?
Symptoms include easy bruising and petechiae. Other signs are nosebleeds, bleeding gums, and heavy periods.
What level of platelets is considered dangerous?
A count below 20,000 to 50,000 platelets per microliter is dangerous. It raises the risk of severe bleeding.
Can certain therapies accelerate platelet recovery?
Yes, growth factors can help speed up platelet recovery after chemotherapy.
When are platelet transfusions needed?
Transfusions are needed when the count is very low (usually below 10,000 to 20,000). They are also needed for significant bleeding.
How does chemotherapy affect platelet count?
Chemotherapy lowers platelet count by affecting bone marrow. The lowest count (nadir) happens around 7-14 days after treatment.
What factors influence platelet recovery after chemotherapy?
Recovery is influenced by cancer type and stage, age, health, chemotherapy, and previous treatments
Reference
Çiftçiler, R., et al. (2020). The impact of early versus late platelet and neutrophil recovery after induction chemotherapy on survival outcomes of acute myeloid leukemia patients. Annals of Hematology, 99(5), 987-995. https://pmc.ncbi.nlm.nih.gov/articles/PMC7236414/
Ramesh, R., et al. (2024). Peripheral blood neutrophil nadir and time to platelet recovery in patients undergoing chemotherapy. World Journal of Oncology, 15(1), 50-58. https://journal.waocp.org/article_91314_1387c831437bb8a20d9eb0f5be25fb7a.pdf