Blog
Liv Hospital aspires to lead the way in providing reliable and high-quality healthcare by combining a patient-centered approach, an experienced team of physicians, and the strength of multidisciplinary collaboration. With our commitment to applying advanced diagnostic and treatment methods in step with global standards, our ultimate focus remains clear: your health.
Sort By Letter
 Pediatrics
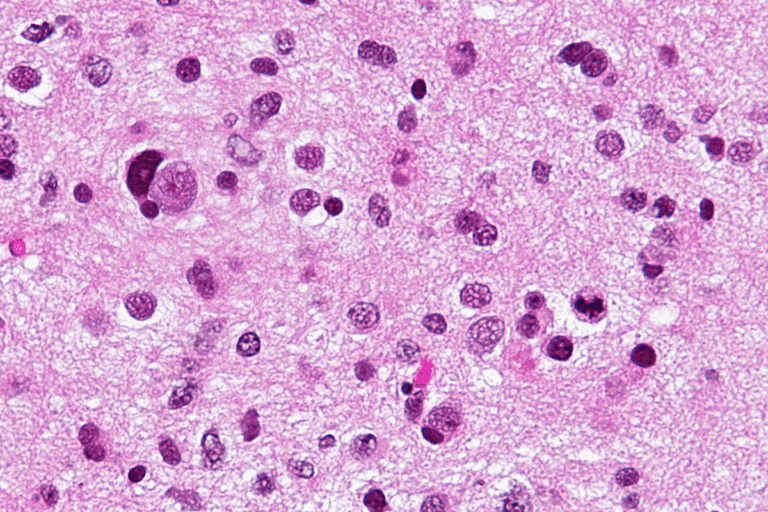
PediatricsMost Challenging Incurable Tumors: A Sobering Look
Recent statistics show that some cancers are hard to treat. This creates big medical oncology challenges. It’s ...
 Adhd
AdhdHow Does Adderall Work in the Brain and Affect Dopamine?
Learn about the science behind Adderall's ability to enhance focus and motivation by regulating dopamine.
 Gastroenterology
GastroenterologyBathroom Use After Hernia Surgery: An Easy Guide
Nearly 800,000 hernia repair surgeries are performed annually in the United States, with a significant number of pati...
 Orthopedics
OrthopedicsComplete Week 2 Hip Replacement: 5 Key Recovery Milestones
After hip replacement surgery, the second week is a big step. At Liv Hospital, we help our patients a lot during this...
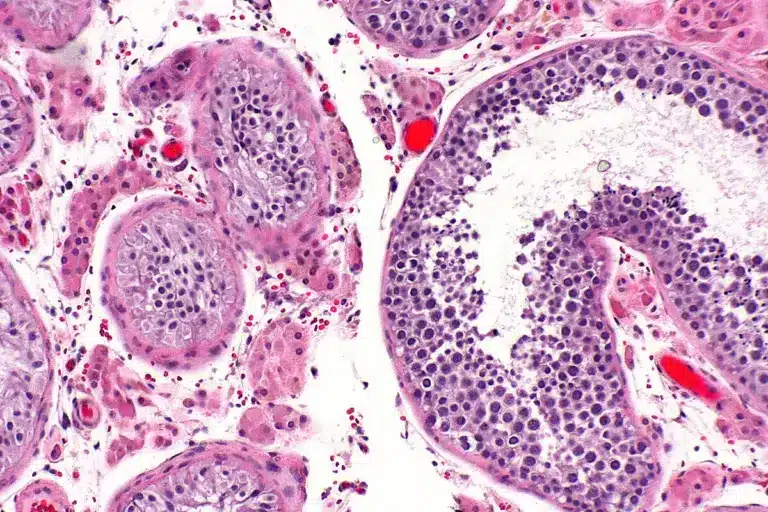 Testicular Cancer
Testicular CancerTesticular Cancer Symptoms: Feeling Sick?
Testicular cancer often hits young men, making it a big concern. Knowing the symptoms early is key to treating it wel...
 General Surgery
General SurgeryHigh Fiber Foods: Best List For Gut Health
high fiber foods Eating foods high in fiber is key for good health. It helps with digestion, heart health, and keepin...
 Kidney Disease
Kidney Disease7 Skin Signs of Kidney Disease: Rashes, Color Changes & Symptoms
Explore the visible skin manifestations of kidney disease, from rashes and color changes to intense itching. Understa...
 Dentistry
DentistryHow to Get a Single Tooth Bridge: Complete Guide
Losing a tooth can really upset you, affecting your confidence and health. Luckily, a single tooth bridge is a good f...
 Ear Nose Throat
Ear Nose ThroatBasal Cell Carcinoma Stages Pictures and Melanoma Photos
Skin cancer is the most common cancer worldwide. Basal cell carcinoma makes up about eight out of ten cases, says the...
No posts found
Try different filters



