We depend on cranial nerves III, IV, and VI for our eye movements and vision. These nerves, or the oculomotor, trochlear, and abducens nerves, are key. They help control the muscles that move our eyes.what true about cranial nerves iii iv and viIPS Induced: What is the True Success Rate?
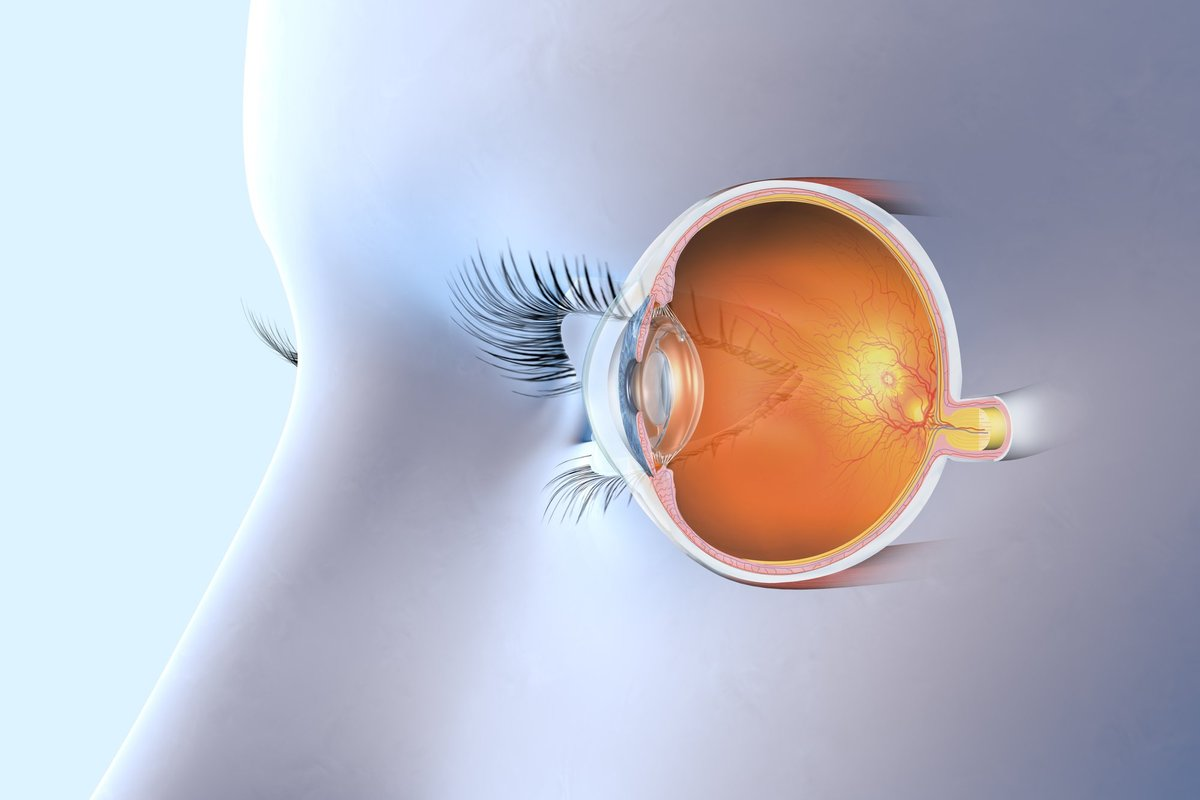
The oculomotor, trochlear, and abducens nerves are special nerves. They start in the brainstem and go through the skull. They then enter the eye area through a special opening.
Key Takeaways
- Cranial nerves III, IV, and VI control eye movements and vision.
- The oculomotor, trochlear, and abducens nerves innervate the extraocular muscles.
- Damage to these nerves can cause significant vision problems.
- Understanding the anatomy and functions of these nerves is essential for diagnosing and treating related disorders.
- These nerves are general somatic efferent nerves that travel through the calvarium and enter the orbit via the superior orbital fissure.
Overview of the Ocular Motor Nerves
The ocular motor nerves, including cranial nerves III, IV, and VI, are key to eye movement control. They work together to help us track objects, read, and do daily tasks smoothly.
Common Functions and Characteristics
The oculomotor (cranial nerve III), trochlear (cranial nerve IV), and abducens (cranial nerve VI) nerves control eye movement. Cranial nerve III controls the medial, superior, inferior rectus, and inferior oblique muscles. Cranial nerve IV controls the superior oblique muscle, and cranial nerve VI controls the lateral rectus muscle.
These nerves have unique roles. For example, cranial nerve III controls eye muscles and also helps with pupil size and lens focus. Their complex interaction ensures precise eye movement control.
Cranial Nerve | Primary Function | Muscle Innervated |
III (Oculomotor) | Somatic Motor and Parasympathetic | Medial Rectus, Superior Rectus, Inferior Rectus, Inferior Oblique |
IV (Trochlear) | Somatic Motor | Superior Oblique |
VI (Abducens) | Somatic Motor | Lateral Rectus |
Anatomical Pathway Through the Cavernous Sinus
Cranial nerves III, IV, and VI pass through the cavernous sinus. This is a key area near the brain’s base. Damage here can cause various clinical syndromes.
“The cavernous sinus is a critical area for nerve pathology, leading to disorders like cavernous sinus syndrome.”
Knowing the nerves’ pathway is vital for diagnosing and treating related disorders. The nerves’ close location in the cavernous sinus means damage can affect one or more nerves. This leads to complex symptoms.
What Is True About Cranial Nerves III, IV, and VI in Eye Movement Control

Cranial nerves III, IV, and VI are key in eye movement. They work together to help us move our eyes and keep our vision clear. This teamwork is what lets us look where we want and see the world in 3D.
Coordinated Actions for Gaze Direction
These nerves control the muscles that move our eyes. The oculomotor nerve (III) helps four muscles move the eye. The trochlear nerve (IV) controls the superior oblique muscle. The abducens nerve (VI) works with the lateral rectus muscle.
When we look to the right, these nerves work together. The right lateral rectus and the left medial rectus muscles contract. This ensures both eyes move together, keeping our vision stable.
“The precise coordination of cranial nerves III, IV, and VI is fundamental to our ability to navigate and interact with our environment.”
Extraocular Muscle Innervation Map
Knowing how these nerves connect to eye muscles is important. The table below shows which nerves control which muscles:
Extraocular Muscle | Cranial Nerve Innervation |
Superior Rectus | Oculomotor (III) |
Medial Rectus | Oculomotor (III) |
Inferior Rectus | Oculomotor (III) |
Inferior Oblique | Oculomotor (III) |
Superior Oblique | Trochlear (IV) |
Lateral Rectus | Abducens (VI) |
The way these nerves and muscles work together shows how complex and precise our vision is.
Cranial Nerve III: The Oculomotor Nerve
The oculomotor nerve, also known as cranial nerve III, is key in controlling eye movements and pupillary functions. It works with cranial nerves IV and VI to control the eye’s motor functions.
Nuclei and Origin in the Midbrain
The oculomotor nerve starts in the midbrain, a vital part of the brainstem. Its nuclei are at the level of the superior colliculus. The oculomotor nucleus is complex, with both somatic motor and parasympathetic components.
We’ll look at the oculomotor nerve nuclei’s structure. The somatic motor nuclei control the extraocular muscles. The parasympathetic Edinger-Westphal nucleus helps in pupillary constriction.
Somatic Motor Functions and Extraocular Muscles
The oculomotor nerve controls several extraocular muscles. These include the superior rectus, medial rectus, inferior rectus, and inferior oblique muscles. These muscles work together for precise eye movements in different directions.
Extraocular Muscle | Primary Action |
Superior Rectus | Elevation |
Medial Rectus | Adduction |
Inferior Rectus | Depression |
Inferior Oblique | Extorsion |
Parasympathetic Functions for Pupillary Control
The oculomotor nerve also has parasympathetic fibers for pupillary control. The Edinger-Westphal nucleus sends signals to the ciliary ganglion. This leads to the sphincter pupillae muscle’s action, causing the pupil to constrict.
Understanding the oculomotor nerve’s dual functions is key for diagnosing and managing eye and pupillary disorders. Its complex anatomy and functions highlight its importance in the ocular motor system.
Cranial Nerve IV: The Trochlear Nerve
Cranial nerve IV, or the trochlear nerve, is special because it exits the brainstem from the back. It controls the superior oblique muscle, making it interesting to study in eye movement.
Unique Dorsal Exit from the Brainstem
The trochlear nerve is the only one that exits the brainstem from the back. This unique dorsal exit sets it apart from other nerves. It comes from the midbrain, below the oculomotor nucleus, and then crosses over before leaving the brainstem.
This special exit is key for doctors to check for nerve problems. It helps them diagnose issues with the trochlear nerve.
Superior Oblique Muscle Innervation and Function
The trochlear nerve controls the superior oblique muscle. This muscle helps the eye move down and in, mainly when the eye is pulled towards the nose.
This nerve’s role in eye movement is vital for seeing things clearly with both eyes. If it doesn’t work right, it can cause double vision.
Longest Intracranial Course and Clinical Implications
The trochlear nerve travels the longest distance inside the skull. It goes around the brain, through the cavernous sinus, and into the eye socket. This long path makes it vulnerable to damage.
Its long journey can lead to nerve problems. These problems can cause the eye to move weakly, leading to double vision, which is worse when looking down.
Cranial Nerve VI: The Abducens Nerve
The sixth cranial nerve, also known as the abducens nerve, is key for moving our eyes outward. We’ll look at where it starts, its path, and what it does. We’ll also see why it’s important in medical terms.
Origin in the Pons and Anatomical Course
The abducens nerve begins in the pons, a part of the brainstem. It travels a long way inside the skull before it gets to the eye area. This makes it more likely to get hurt.
Lateral Rectus Muscle Function
The main job of the abducens nerve is to control the lateral rectus muscle. This muscle helps move the eye outward.
Vulnerable Intracranial Course and Compression Points
Because of its long path inside the skull, the abducens nerve is at risk of getting compressed or damaged. This can lead to abducens nerve palsy, causing double vision when looking sideways.
Here’s a quick summary of the abducens nerve:
Aspect | Description |
Origin | Pons |
Primary Function | Innervation of the lateral rectus muscle |
Clinical Significance | Vulnerable to compression or injury due to its long intracranial course |
Clinical Disorders and Palsies
Palsies of the oculomotor, trochlear, and abducens nerves can really affect a person’s life. These conditions cause symptoms like double vision, eyelid drooping, and unusual head positions.
Oculomotor Nerve Palsy and Pupil-Involving vs. Pupil-Sparing
Oculomotor nerve palsy, or third nerve palsy, can happen for many reasons. It might be due to lack of blood flow, aneurysms, or injuries. There are two main types: pupil-involving and pupil-sparing palsies. Pupil-involving palsies are often linked to serious issues like aneurysms. On the other hand, pupil-sparing palsies are more common in people with diabetes.
Key Features of Oculomotor Nerve Palsy:
- Ptosis
- Dilated pupil (in pupil-involving palsy)
- Downward and outward deviation of the eye
- Impaired extraocular muscle function
Trochlear Nerve Palsy and Head Tilt
Trochlear nerve palsy affects the superior oblique muscle. This leads to weakness in moving the eye up, down, and outward. People often tilt their head to help, which can reduce double vision.
Clinical findings may include:
Symptom | Description |
Head tilt | Compensatory mechanism to reduce diplopia |
Vertical diplopia | Worsens on looking down |
Trochlear nerve dysfunction | Impaired superior oblique muscle function |
Abducens Nerve Palsy and Horizontal Diplopia
Abducens nerve palsy weakens or paralyzes the lateral rectus muscle. This muscle is needed for eye movement outward. The result is double vision that gets worse when looking to the side.
Diagnostic Features:
- Horizontal diplopia
- Esotropia (inward deviation of the eye)
- Impaired lateral rectus muscle function
It’s important to understand these conditions well. This helps doctors make the right diagnosis and treatment plan. The complex relationship between the oculomotor, trochlear, and abducens nerves is key to managing these issues.
Examination and Diagnostic Techniques
Managing ocular motor nerve disorders starts with precise exams and tests. We need a detailed clinical check-up and the right tests to see how cranial nerves III, IV, and VI work.
Clinical Assessment of Eye Movements and Alignment
Checking eye movements and alignment is key to diagnosing these disorders. We look at how far the eyes can move and if there are any issues. We also see if the patient can follow a target with their eyes and check for nystagmus or strabismus.
The cover test helps find strabismus by covering one eye and then the other. The Hirschberg test also helps by looking at the light reflection on the cornea to estimate strabismus.
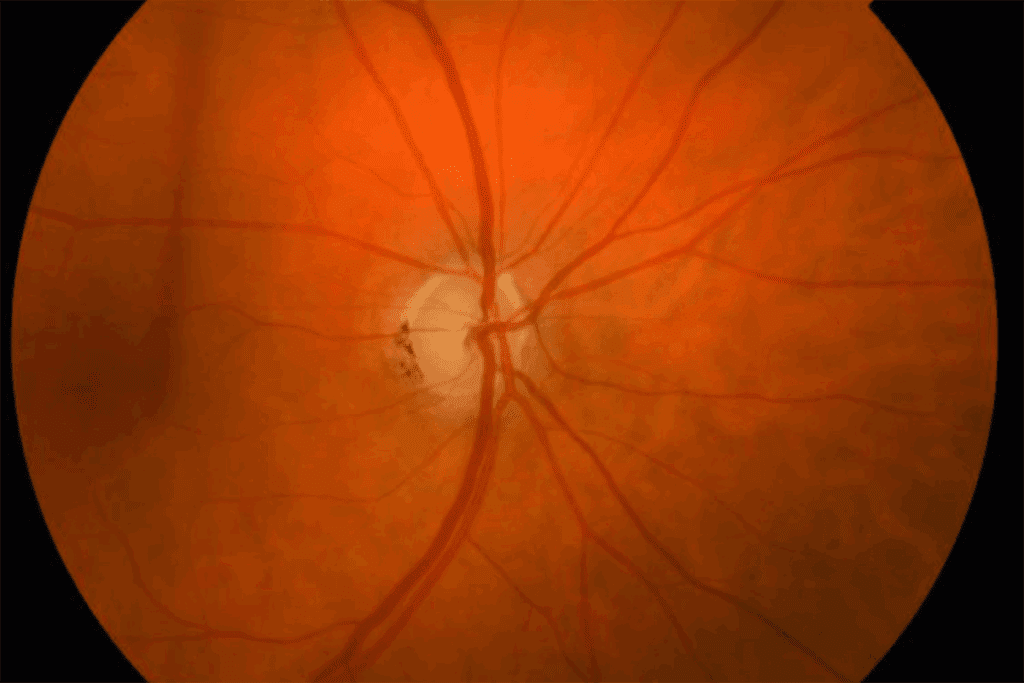
Pupillary Light Reflex and Accommodation Testing
Testing the pupillary light reflex is important for checking the oculomotor nerve’s parasympathetic function. We shine a light in the eye and watch the pupil’s reaction. A normal response means the nerve pathways are working right.
Accommodation testing checks how well the eyes focus on near objects. It looks at the convergence of the eyes and the constriction of the pupils. This test shows if the oculomotor nerve is working correctly.
Neuroimaging in Ocular Motor Nerve Disorders
Neuroimaging is vital for finding the cause of these disorders. We use MRI or CT scans to see the brainstem, cavernous sinus, and orbit. These scans can spot lesions, tumors, or vascular problems affecting the nerves.
Imaging Modality | Advantages | Clinical Use |
MRI | High soft tissue resolution, no radiation | Evaluating brainstem lesions, cavernous sinus pathology |
CT Scan | Quick, good for bony structures | Assessing orbital trauma, bony abnormalities |
By using clinical checks and advanced neuroimaging, we can accurately diagnose and manage ocular motor nerve disorders. This improves patient outcomes.
Anatomical Relationships and Syndromes
It’s key to know how ocular motor nerves connect with other parts of the body. This knowledge helps doctors spot and treat related health issues. The nerves III, IV, and VI work together closely. Problems with these nerves can cause different syndromes.
We’ll look at three main syndromes. These are Cavernous Sinus Syndrome, Superior Orbital Fissure Syndrome, and how Brainstem Lesions affect these nerves.
Cavernous Sinus Syndrome and Multiple Cranial Nerve Involvement
The cavernous sinus is a key area where nerves III, IV, and VI meet. Cavernous Sinus Syndrome happens when something goes wrong in this area. It can cause problems with many nerves.
Signs include eye muscle weakness, eyelid drooping, and numbness in the face. This makes Cavernous Sinus Syndrome stand out from other nerve issues.
Superior Orbital Fissure Syndrome
Superior Orbital Fissure Syndrome is linked to the nerves and the area around them. It occurs when something goes wrong near the superior orbital fissure. This is a narrow spot where nerves III, IV, and VI enter the eye socket.
Its symptoms are similar to Cavernous Sinus Syndrome. But, it mainly affects nerves going through the fissure.
Brainstem Lesions Affecting Ocular Motor Nerves
Lesions in the brainstem can harm the nuclei or paths of nerves III, IV, and VI. These can be caused by strokes, tumors, or diseases that damage the protective covering of nerves.
The symptoms depend on where and how big the brainstem lesion is. For example, a problem with the oculomotor nucleus can cause eye weakness and eyelid drooping on one side.
It’s vital to understand the brainstem’s anatomy and its connection to ocular motor nerves. This knowledge helps doctors diagnose and treat these conditions well.
Conclusion
We’ve looked into the complex anatomy and functions of cranial nerves III, IV, and VI. These nerves are key in controlling eye movement and vision. They work together to help us move our eyes smoothly and see clearly.
These nerves are very important for our health. Problems with them can cause serious vision issues, like double vision. Knowing how these nerves work helps doctors diagnose and treat these problems better.
In summary, the connection between cranial nerves III, IV, and VI shows how complex our vision system is. As we learn more about these nerves, we can find better ways to treat related disorders. This will help improve the lives of those affected.
FAQ
What are the primary functions of cranial nerves III, IV, and VI?
These nerves control eye movements. They work with the extraocular muscles. This helps us move our eyes and see in 3D.
Which cranial nerves control eye movement?
The oculomotor (III), trochlear (IV), and abducens (VI) nerves control eye movements. They work together for precise eye actions.
What is the role of the oculomotor nerve in eye movement?
The oculomotor nerve controls many eye muscles. It also helps with pupil size. This is key for clear vision.
What is unique about the trochlear nerve’s anatomy?
The trochlear nerve exits the brainstem from the back. It has the longest path inside the skull. This makes it more likely to get damaged.
What is the function of the abducens nerve?
The abducens nerve controls the lateral rectus muscle. This muscle helps us look to the side. Its path makes it prone to damage.
What are the characteristic features of oculomotor nerve palsy?
Oculomotor nerve palsy can cause droopy eyelids and eyes that look down and out. It also makes pupils bigger. The effect on pupils can vary.
How is trochlear nerve palsy diagnosed?
Trochlear nerve palsy is often seen with a head tilt. This is to help the eye move better. Doctors check eye movements to diagnose it.
What diagnostic techniques are used to assess ocular motor nerve function?
Doctors use eye movement tests and check how eyes line up. They also test the light reflex and use scans to diagnose nerve problems.
What is cavernous sinus syndrome?
Cavernous sinus syndrome affects many nerves. It happens when there’s a problem in the cavernous sinus. This can harm eye nerves and others nearby.
How do brainstem lesions affect ocular motor nerves?
Brainstem lesions can harm the nuclei or paths of eye nerves. This leads to eye movement issues and other neurological problems.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK406/