Last Updated on November 13, 2025 by
Chemotherapy is a common treatment for many cancers. It can harm blood cell production. This damage to the bone marrow can cause a low blood cell count. How does chemo affect blood count? Learn what type of cancer causes low hemoglobin and the terrible impact chemotherapy has on blood cell production.
It affects red blood cells, white blood cells, and platelets. What precautions might we take in a child? Get the crucial and powerful list of infection control precautions for young cancer patients during treatment.
At LIV Hospital, we know managing chemotherapy side effects is key. We look into how chemotherapy impacts blood counts. We also talk about the risks and ways to manage these side effects. Our goal is to provide complete care.
Key Takeaways
- Chemotherapy can suppress blood cell production by damaging bone marrow.
- Low blood cell counts can lead to increased risks of infection, anemia, and bleeding.
- Managing side effects is vital for patient well-being.
- Comprehensive care includes monitoring and addressing the impact of chemotherapy on blood counts.
- Effective strategies can help lessen the risks of low blood cell counts.
Understanding Blood Count Basics
A complete blood count (CBC) test is key in finding and tracking cancer. It shows the levels of white, red blood cells, and platelets. Knowing these levels helps cancer patients manage their treatment better.
Components of a Complete Blood Count
A CBC checks the levels of different blood cells. The main parts are:
- White Blood Cells (WBCs): These fight infections.
- Red Blood Cells (RBCs): They carry oxygen.
- Platelets: Important for blood clotting.
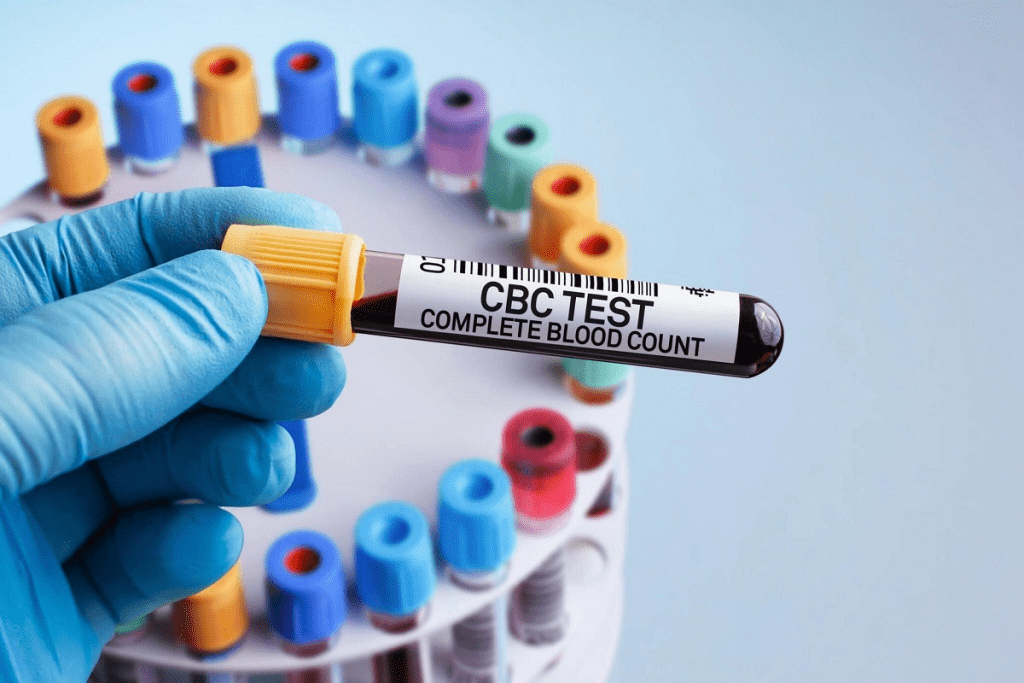
Normal Blood Count Ranges
Knowing the normal ranges for each blood cell is important. These can vary slightly by lab but usually are:
- WBC count: 4,500 to 11,000 cells per microliter
- RBC count: 4.32 to 5.72 million cells per microliter for men and 3.90 to 5.03 million cells per microliter for women
- Platelet count: 150,000 to 450,000 platelets per microliter
Importance of Blood Count in Cancer Care
Keeping an eye on blood counts is vital in cancer care, mainly during chemo. It helps in:
- Checking the risk of infection with low WBC counts.
- Finding anemia through RBC count and hemoglobin levels.
- Seeing the risk of bleeding with low platelet counts.
By knowing about blood counts, cancer patients can handle their treatment and side effects better. This improves their life quality.
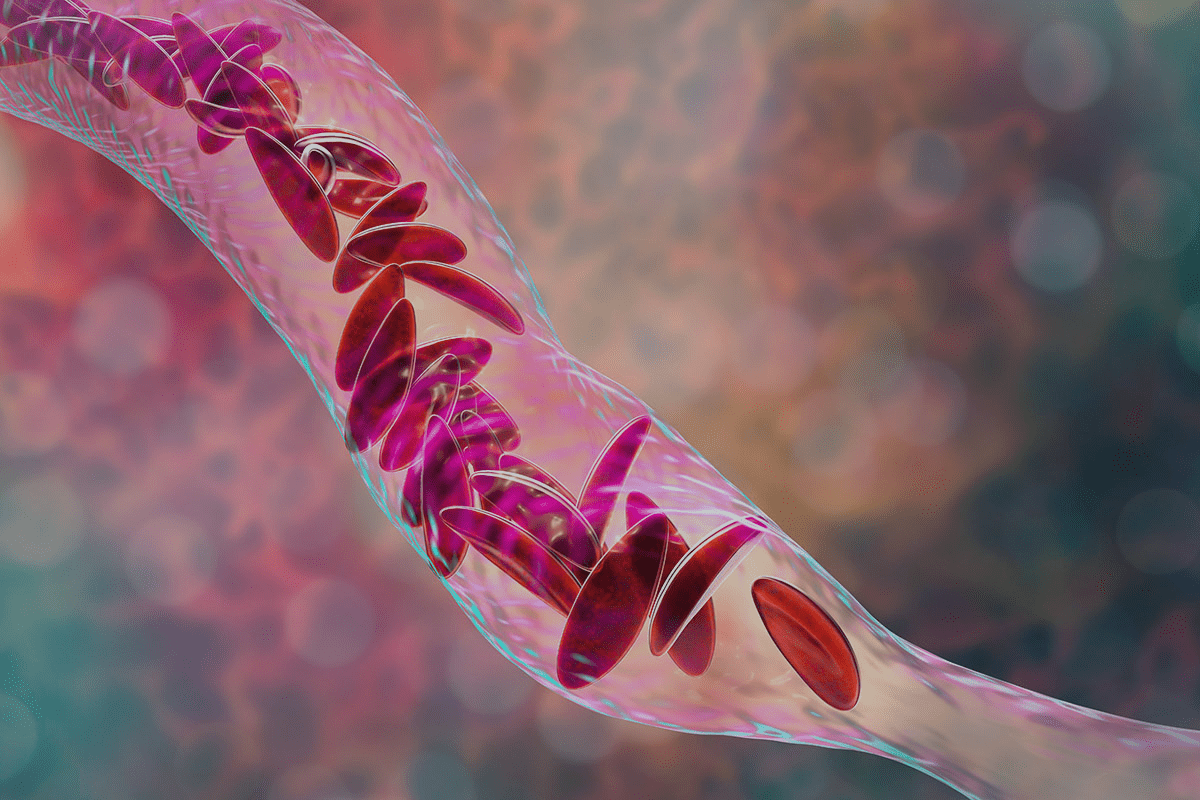
The Mechanism of Chemotherapy on Bone Marrow
Chemotherapy’s impact on bone marrow is complex. It suppresses blood cell production. This is because chemotherapy targets cells that divide quickly, like cancer cells.

How Chemotherapy Targets Rapidly Dividing Cells
Chemotherapy drugs aim at cells that divide fast, a trait of cancer. These drugs block cell division, slowing cancer growth. But, they also hit bone marrow cells, which produce blood cells.
“Chemotherapy’s effect on bone marrow can lower blood cell counts,” experts say. “This makes patients more likely to get infections, anemia, and bleeding problems.” Knowing this helps manage chemotherapy’s side effects.
Bone Marrow Suppression Process
Bone marrow suppression happens when chemotherapy hits bone marrow cells. This can cut down on red, white, and platelet blood cells. How much and for how long depends on the chemotherapy type and dose.
- Red blood cells carry oxygen and can drop, causing anemia.
- White blood cells fight infections and can fall, leading to neutropenia.
- Platelets help blood clot and can be reduced, causing thrombocytopenia.
Variability of Effects by Chemotherapy Type
Chemotherapy drugs affect bone marrow differently. Some cause more severe suppression, lasting longer. Knowing the chemotherapy type and its bone marrow effects is key to managing risks.
“The type and dose of chemotherapy are critical factors in determining the extent of bone marrow suppression,” says a leading oncologist. “Tailoring the treatment to the individual patient’s needs can help mitigate some of these effects.”
Understanding how chemotherapy impacts bone marrow and blood cell production helps doctors. They can then manage cancer treatment risks better. This improves patient outcomes and quality of life.
Impact on Red Blood Cells and Hemoglobin
Chemotherapy is a key treatment for many cancers. But, it affects the body’s blood cells, like red blood cells and hemoglobin, a lot. It can lead to anemia, a condition where the body doesn’t make enough red blood cells.
Chemotherapy-Induced Anemia Statistics
Anemia is a common side effect of cancer treatment. Up to 35% of patients get anemia after chemotherapy. This happens because chemotherapy kills not just cancer cells but also fast-dividing cells in the bone marrow that make red blood cells.
The chance of getting anemia depends on the type of chemotherapy, the dose, and the patient’s health. Knowing these facts helps doctors manage anemia better in patients getting chemotherapy.
Symptoms of Low Hemoglobin During Treatment
Low hemoglobin during chemotherapy can cause several symptoms. These include:
- Fatigue and weakness
- Shortness of breath
- Dizziness or lightheadedness
- Pale skin
- Headaches
These symptoms can really affect a patient’s life. It’s important for doctors to keep an eye on hemoglobin levels and fix any problems quickly.
How Anemia Affects Quality of Life
Anemia can really change a patient’s life. It can make it hard to do everyday things, feel emotionally well, and handle cancer treatment. Fatigue, a common symptom, can stop patients from doing things they love.
Also, anemia can make cancer treatment less effective. Patients with anemia might need to change their treatment plans. This could affect how well the treatment works. So, managing anemia well is key to a good quality of life and effective treatment.
What Type of Cancer Causes Low Hemoglobin
It’s important to know what type of cancers effect hemoglobin levels. Low hemoglobin, or anemia, is common in cancer patients. It can happen due to the disease itself or its treatment.
Blood Cancers and Their Effect on Hemoglobin
Blood cancers like leukemia, lymphoma, and multiple myeloma harm blood cell production. This includes red blood cells that carry hemoglobin. These cancers can lower healthy red blood cells, causing low hemoglobin levels.
- Leukemia: Affects the bone marrow, where red blood cells are made, leading to anemia.
- Lymphoma: Can cause anemia by affecting the bone marrow or the body’s immune response.
- Multiple Myeloma: Directly impacts plasma cells in the bone marrow, affecting normal blood cell production.
Solid Tumors That Impact Red Blood Cell Production
Solid tumors can also lower hemoglobin levels, often indirectly. They can cause chronic inflammation, nutritional deficiencies, or directly harm the bone marrow. This affects red blood cell production.
“Chronic diseases, including cancer, can lead to anemia of chronic disease, characterized by low hemoglobin levels due to the body’s inflammatory response.”
Source: Medical Oncology Journal
Examples of solid tumors that can impact hemoglobin include:
- Cancers of the gastrointestinal tract, which can lead to chronic blood loss or nutritional deficiencies.
- Tumors that metastasize to the bone, potentially affecting bone marrow function.
Does Low Blood Count Mean Cancer?
A low blood count, including low hemoglobin, can be a symptom of cancer. But it’s not only found in cancer. Many non-cancerous conditions can also cause low blood counts. In cancer cases, a low blood count can suggest the presence of a malignancy, mainly blood cancers.
If you’re experiencing symptoms like fatigue or shortness of breath, see your healthcare provider. Early diagnosis and treatment can greatly improve your health.
Effects on White Blood Cell Count
Chemotherapy can change white blood cell counts, making patients more likely to get infections. White blood cells are key to fighting infections and diseases. When chemotherapy hits these cells, it can cause neutropenia.
Understanding Neutropenia and Infection Risk
Neutropenia means having too few neutrophils, a type of white blood cell. It’s a common side effect of chemotherapy. This makes patients more at risk for infections.
Key risks associated with neutropenia include:
- Increased susceptibility to infections
- Potential for severe infections due to a compromised immune system
- Possible delays in chemotherapy treatment due to low white blood cell counts
Low WBC Symptoms to Monitor
Patients on chemotherapy should watch for low white blood cell count symptoms. These include:
- Frequent or persistent infections
- Fever or chills
- Sore throat or mouth sores
- Cough or difficulty breathing
Keeping an eye on these symptoms and telling your healthcare provider is important. It helps manage neutropenia risks.
What Cancer Causes Low Neutrophils
Chemotherapy isn’t the only cause of low neutrophil counts. Some cancers, like leukemia or lymphoma, can also affect white blood cell production. Knowing why you have low neutrophils is key to finding the right treatment.
Understanding how chemotherapy affects white blood cells and the risks of neutropenia is important. Patients and healthcare providers can work together to manage these side effects. This helps reduce the risk of complications.
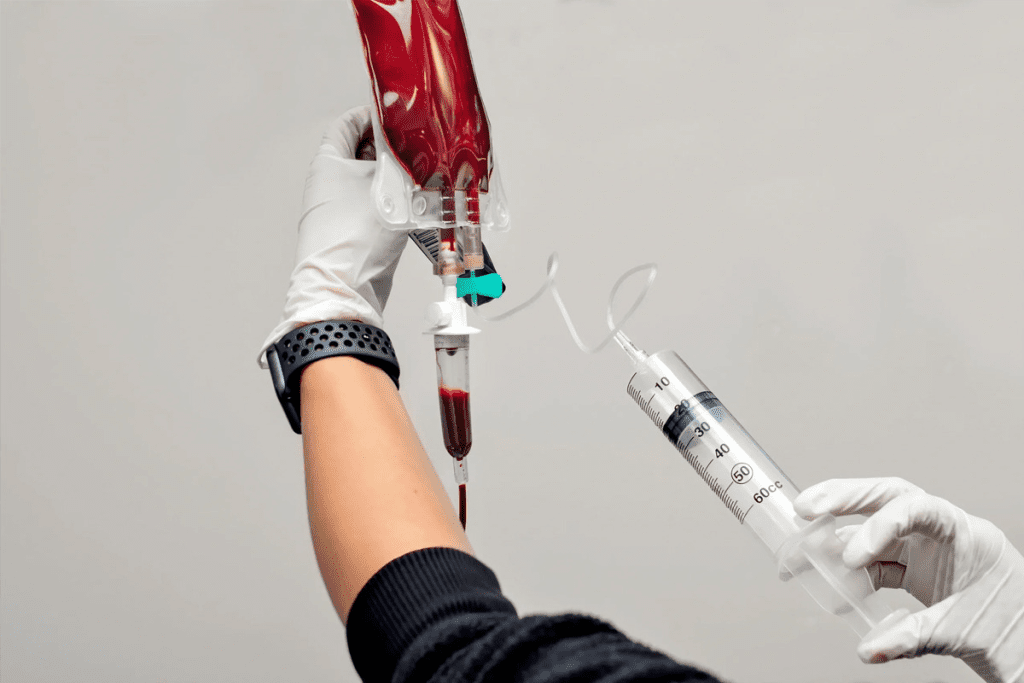
Platelet Suppression and Bleeding Complications
Chemotherapy can lower platelet counts, causing thrombocytopenia. This increases the risk of bleeding. We will look at why platelets drop and how to manage bleeding risks during treatment.
Low Platelets as a Cancer Symptom
Low platelet count, or thrombocytopenia, can be a sign of cancer. It’s common in diseases like leukemia that harm the bone marrow. Cancer cells can invade the bone marrow, making it hard to produce platelets. This can cause more bruising and bleeding.
Chemotherapy-Induced Thrombocytopenia
Chemotherapy can lower platelet counts because it targets fast-growing cells in the bone marrow. The severity and how long it lasts can depend on the type and dose of chemotherapy. Knowing the risks of your chemotherapy is key to managing this side effect.
Managing Bleeding Risks During Treatment
To manage bleeding risks during chemotherapy, a mix of medical care and lifestyle changes is needed. Regularly checking platelet counts helps doctors adjust treatment plans. Patients can also take steps to lower bleeding risks, like avoiding injuries, gentle oral care, and being careful with sharp objects.
- Use a soft-bristled toothbrush to prevent gum bleeding.
- Avoid contact sports and activities that could lead to injury.
- Be cautious when handling sharp objects, such as razors or knives.
Understanding the risks of chemotherapy-induced thrombocytopenia and taking action can help patients avoid bleeding complications. This way, they can safely go through their treatment.
Timeline of Blood Count Changes After Chemotherapy
Chemotherapy affects blood counts in a predictable way. Knowing this timeline helps manage side effects and improve patient outcomes.
Initial Impact on Blood Production
Chemotherapy targets fast-growing cells, including those in the bone marrow. This leads to blood count changes soon after treatment starts. The impact varies based on the chemotherapy type, dose, and patient factors.
“Chemotherapy-induced myelosuppression is a common side effect, affecting the production of blood cells,” as noted in various medical studies. This suppression can lead to a decrease in red blood cells, white blood cells, and platelets.
Peak Suppression Period (1-2 Weeks Post-Treatment)
The nadir or peak suppression period for blood counts is usually 1-2 weeks after chemotherapy. During this time, patients face a higher risk of infections, anemia, and bleeding. Close monitoring and supportive care are critical during this period.
- Red blood cell count decreases, potentially leading to anemia.
- White blood cell count drops, increasing the risk of infections.
- Platelet count decreases, potentially causing bleeding complications.
Recovery Patterns Before Next Cycle
Fortunately, blood counts usually start to recover after the nadir. Many patients return to baseline levels before the next chemotherapy cycle. Recovery patterns vary based on the chemotherapy regimen, patient health, and other factors.
“Understanding the recovery patterns of blood counts is essential for managing patient care and adjusting treatment plans as necessary,” according to clinical guidelines.
By understanding the timeline of blood count changes after chemotherapy, healthcare providers can better manage patient care. They can adjust treatment plans and supportive measures to minimize complications and optimize outcomes.
Long-Term Genomic Effects on Blood Cells
Chemotherapy’s effects on blood cells last long after treatment ends. It causes big changes in the genes of blood cells. Knowing these changes helps manage treatment results and lower long-term risks.
DNA Changes Following Chemotherapy
Chemotherapy can change the DNA in blood cells, leading to genetic mutations. These changes might make blood cells work differently and raise the chance of getting secondary cancers. Research shows some chemotherapy drugs are more likely to damage genes, so treatment plans need to be careful.
Accelerated Aging of Blood Cells
Studies show chemotherapy can make blood cells age faster. This can lead to early aging and health problems. It makes patients more likely to get sick and face other health issues.
Secondary Cancer Risk Factors
Chemotherapy is a big risk for getting secondary cancers. The risk depends on the type and amount of chemotherapy, and how a patient reacts.
Important factors for the long-term effects of chemotherapy include:
- Type and dosage of chemotherapy agents
- Individual patient genetic susceptibility
- Duration of chemotherapy treatment
Understanding how chemotherapy affects blood cells long-term helps doctors manage side effects. It also lowers the chance of long-term problems. This knowledge helps patients and doctors create care plans that treat cancer well while avoiding long-term risks.
How to Boost White Blood Cell Count During Treatment
Boosting white blood cells can lower the risk of infections during treatment. A healthy count is key for those on chemotherapy. It helps fight off infections and aids in recovery.
Medical Interventions
Medical help is vital for boosting white blood cells. Growth factors like granulocyte-colony stimulating factor (G-CSF) are used. They make the bone marrow produce more white blood cells. These are given by injection when the count is low.
A study on Medical News Today shows G-CSF’s success in raising counts in chemotherapy patients. Knowing about growth factors helps patients choose their treatments wisely.
Nutritional Approaches
Nutritional approaches also support white blood cell production. Eating fruits, vegetables, whole grains, and lean proteins is important. Foods like berries and leafy greens are full of antioxidants.
Supplements like vitamin C, vitamin D, and zinc can boost immunity. But, always talk to your doctor before taking them to avoid side effects.
Lifestyle Modifications
Making lifestyle changes is also key. Regular exercise boosts the immune system. Aim for 30 minutes of brisk walking daily.
Getting enough sleep and managing stress is also important. Try meditation or deep breathing to reduce stress. These changes can help avoid complications and improve treatment results.
Managing Low WBC and RBC Simultaneously
Dealing with low white blood cell (WBC) and red blood cell (RBC) counts at the same time is tough. This is called pancytopenia. It happens when many blood cell types are low, needing a detailed plan to manage it.
Comprehensive Approaches to Pancytopenia
Pancytopenia is a serious issue that needs a detailed treatment plan. Managing it well involves several important steps:
- Regular checks on blood cell counts to see how bad pancytopenia is
- Changing chemotherapy plans to lessen harm to blood cells
- Using transfusions and growth factor therapy to boost blood cell counts
- Helping patients eat well to support blood cell making
With a detailed plan, doctors can reduce pancytopenia’s risks and help patients do better.
Treatment Adjustments When Multiple Cell Lines Are Affected
When many blood cell types are low, changing treatment is key. Changing chemotherapy plans can help less harm blood cells. This might mean:
- Slowing down or cutting back on chemotherapy to let blood cells recover
- Switching to chemotherapy that’s less hard on blood cells
- Starting supportive care like G-CSF to help make more white blood cells
Changing treatment plans needs careful thought and watching closely. It’s about finding the right balance between fighting cancer and keeping blood counts up.
Balancing Cancer Treatment with Blood Count Recovery
Finding the right balance between fighting cancer and helping blood counts recover is tricky. Doctors have to think carefully about keeping chemotherapy going while watching blood counts. Ways to do this include:
- Planning chemotherapy cycles with breaks in between for recovery
- Using supportive care to help blood cells
- Keeping a close eye on blood counts to make treatment choices
By using these methods, patients can get good cancer treatment without risking too much with low blood counts.
Conclusion
Chemotherapy can really affect blood counts, including red, white blood cells, and platelets. It’s important to understand these effects to manage side effects and improve health outcomes.
At LIV Hospital, we focus on top-notch healthcare and support for international patients. We help patients and doctors work together to lessen treatment side effects. This way, we can make treatment better for everyone.
Managing blood count changes from chemotherapy needs a team effort. This includes medical help, good nutrition, and changes in lifestyle. With these steps, patients can face chemotherapy’s challenges and get better health results.
FAQ
What are the symptoms of low white blood cell count?
Low white blood cell count, or leukopenia, can cause frequent infections and fever. You might also feel tired and unwell. In serious cases, it can lead to dangerous infections.
Is low platelet count a symptom of cancer?
Yes, low platelet count, or thrombocytopenia, can be a sign of cancer. This includes leukemia and lymphoma. It can also happen as a side effect of chemotherapy.
Does low blood count mean cancer?
Not always. Low blood count can be due to many reasons, like chemotherapy or bone marrow issues. While it might be linked to cancer, it’s not a sure sign.
What cancer causes low neutrophils?
Leukemia and lymphoma can cause low neutrophil count. Chemotherapy and radiation therapy can also lower neutrophils.
How to boost white blood cell count during chemotherapy?
To boost white blood cells during chemotherapy, try medical treatments and a healthy diet. Eat lots of fruits, vegetables, and whole grains. Also, rest well and manage stress.
What is the normal range for white blood cell count in leukemia?
In leukemia, white blood cell count can be too high or too low. A CBC test can show this and help diagnose leukemia.
How to raise white blood cell count after chemotherapy?
To raise white blood cells after chemotherapy, use medical treatments, eat well, and reduce stress. A balanced diet and stress reduction are key.
What are the risks of low red and white blood cell count?
Low red and white blood cell count, or pancytopenia, raises the risk of anemia and infections. It also increases the risk of bleeding. It needs careful management to balance treatment and recovery.
Is leukopenia a sign of cancer?
Leukopenia can be a sign of cancer, like leukemia. But it can also be caused by other things, like chemotherapy or bone marrow disorders.
How to manage low white blood cell and red blood cell counts simultaneously?
Managing low white and red blood cell counts together needs a detailed plan. This includes adjusting treatments, nutritional support, and lifestyle changes. It aims to balance treatment with recovery.
References
- Mitchell, E., et al. (2025). The long-term effects of chemotherapy on normal blood cells. Nature Genetics, 57, 1124-1131. https://www.nature.com/articles/s41588-025-02234-x
- Adeel, M., et al. (2024). Quantifying anticancer drug toxicity on white blood cell populations. Toxicology Reports, 11, 201-210. https://www.sciencedirect.com/science/article/pii/S101836472300486X