Last Updated on November 26, 2025 by Bilal Hasdemir

Colorectal cancer is a major cause of death, but catching it early can save lives. Learn when to have a colonoscopy based on age, family history, and medical guidelines for early detection.
New guidelines say adults at low risk should have their first colonoscopy at 45. The US Preventive Services Task Force also suggests screening for those between 45 and 75. This early check can stop colorectal cancer or find it when it’s easier to treat.
Key Takeaways
- Adults at average risk should get their first colonoscopy at age 45.
- The US Preventive Services Task Force recommends screening for adults between 45 and 75 years old.
- Early detection of colorectal cancer significantly improves survival rates.
- Colonoscopy is a key tool in preventing and detecting colorectal cancer.
- Liv Hospital is committed to quality and patient-focused care.
The Critical Role of Colorectal Cancer Screening
Colorectal cancer cases are rising, hitting younger adults hard. Screening is key for early detection and prevention. It finds polyps in the colon or rectum before they become cancer.
New guidelines show more cases in adults under 50. This change highlights the need for early screening. The American Cancer Society and others now recommend starting screening earlier.
Colorectal Cancer Statistics in the United States
Colorectal cancer is a big problem in the U.S. There are about 150,000 new cases each year. It’s a major cause of cancer deaths, but many could be saved by finding and removing polyps early.
Younger adults are getting colorectal cancer more often. Those born around 1990 face twice the risk of colon cancer and quadruple the risk of rectal cancer compared to those born in 1950. This has led to new screening guidelines.
How Early Detection Impacts Survival Rates
Screening can greatly improve survival chances for colorectal cancer. Early detection means a five-year survival rate that’s much higher. Screening helps find polyps early, preventing cancer.
Screening can cut colorectal cancer deaths by up to 30%. Early detection is key. It’s vital to follow screening guidelines, even more so for those at higher risk.
When to Have a Colonoscopy: Updated Guidelines
New guidelines say people at average risk should start colonoscopy screenings at 45. This is a big change from what we used to think.
The American Cancer Society now says adults at average risk should start colon cancer screenings at 45. This change is based on new evidence. It shows that screening earlier can really help lower the risk of colorectal cancer.
The Recent Shift from Age 50 to Age 45
Experts lowered the age for colonoscopy screening because of a rise in colorectal cancer in younger adults. This change is a response to new data.
The American Cancer Society made this change to 45 because of more cases of colorectal cancer in people under 50. This aims to catch cancer early, when it’s easier to treat.
Research Evidence Supporting Earlier Screening
Studies show that starting colonoscopy screening at 45 can greatly reduce colorectal cancer cases and deaths.
| Study | Findings | Implications |
| American Cancer Society Study | Screening at 45 reduces colorectal cancer incidence by 15% | Earlier screening can lead to better outcomes |
| Journal of the National Cancer Institute | Lowering screening age to 45 saves lives | Supports guideline changes to age 45 |
People with a higher risk, like those with a family history of colorectal cancer, might need to start screening even earlier than 45. It’s key for them to talk to their doctor about when to start.
Knowing the new guidelines and the research behind them helps people make better health choices. This can lower their risk of colorectal cancer.
At What Age Should You Get a Colonoscopy?
Guidelines for colonoscopies have changed, and knowing when to start is key for staying healthy. The American Cancer Society and other experts have updated their advice. This is based on new research and data on colorectal cancer screening.
Most health groups agree that people at average risk should start screening at 45. This advice comes from studies showing early screening can lower the risk of colorectal cancer.
Standard Recommendations for Average-Risk Adults
For those at average risk, starting screening at 45 is recommended. This advice is for people without a history of colorectal cancer or a high family risk. It also applies to those without certain genetic syndromes.
Average-risk adults should talk to their doctor about screening options. These might include colonoscopy, stool tests, or other methods. The choice depends on personal preference, medical history, and what’s available.
Defining “Average Risk” vs. “High Risk”
Knowing your risk level is important for when to start screening. People at average risk don’t have:
- A history of colorectal cancer or certain polyps
- A first-degree relative (parent, sibling, or child) with colorectal cancer before 60
- A genetic syndrome linked to colorectal cancer, like Lynch syndrome
- Inflammatory bowel disease (Crohn’s or ulcerative colitis)
Those at higher risk due to family history, medical history, or genetics might need to start screening earlier. The exact timing depends on individual risk factors.
| Risk Category | Recommended Starting Age for Screening | Screening Interval |
| Average Risk | 45 | 10 years for colonoscopy |
| High Risk (Family History) | 40 or 10 years before the age of the earliest diagnosis in the family | Varies based on initial findings and family history |
| High Risk (Genetic Syndrome) | Varies by syndrome; often starts in late teens or early twenties | Annual or as recommended by genetic guidelines |
It’s vital to talk to your doctor to figure out your risk and the best screening plan. By understanding your risk and following guidelines, you can help keep your colorectal health in check.
High-Risk Individuals: When to Start Screening Earlier
For people at high risk of colorectal cancer, the first colonoscopy timing is key. Certain factors raise your risk, making early screening vital.
Family History Considerations
A family history of colorectal cancer is a big risk factor. If a first-degree relative (like a parent or sibling) got cancer early, your risk goes up. Those with a family history should start screenings early.
The screening start age depends on when your relative was diagnosed. For example, if a first-degree relative got cancer before 60, start screening 10 years before that.
Personal Medical History Factors
Your medical history also affects when to start colonoscopy screening. Conditions like inflammatory bowel disease (IBD) raise your cancer risk.
If you have IBD, your doctor might suggest starting screening 8-10 years after diagnosis. Regular checks are key to catch problems early.
Genetic Syndromes Requiring Earlier Screening
Some genetic syndromes greatly increase colorectal cancer risk. These include Familial Adenomatous Polyposis (FAP) and Lynch Syndrome. If you have one, your doctor will push for more frequent screenings.
For FAP, annual screenings start at 10-12 years old. Lynch Syndrome screenings begin between 20 and 25 years old.
| Risk Factor | Recommended Screening Age | Screening Interval |
| First-degree relative with CRC diagnosed before 60 | 10 years before the relative’s diagnosis age | Every 5 years |
| Inflammatory Bowel Disease (IBD) | 8-10 years after IBD diagnosis | Every 1-3 years |
| Familial Adenomatous Polyposis (FAP) | 10-12 years old | Annually |
| Lynch Syndrome | 20-25 years old | Every 1-2 years |
Gender-Specific Considerations for Colonoscopy Timing
Men and women both need colonoscopy screenings, but timing can vary. This depends on individual risk factors. Knowing these factors helps determine the best screening time.
At What Age Should a Man Have a Colonoscopy?
Men should start colonoscopy screenings at 45, following the general guideline. But, if there’s a family history of colorectal cancer, they might need to start earlier.
Key considerations for men include:
- A family history of colorectal cancer, if a first-degree relative was diagnosed before age 60.
- A personal history of colorectal polyps or cancer.
- Known or suspected genetic syndromes that increase colorectal cancer risk, like Lynch syndrome.
Recommendations for Women’s First Colonoscopy
Women should also start their first colonoscopy at 45 if they’re at average risk. Their risk factors, like family history or certain medical conditions, can affect when they should get screened.
Women should talk to their healthcare provider about their risk factors. Certain conditions, like radiation exposure or genetic syndromes, might mean they need to get screened earlier.
Lifestyle and Medical History Considerations
Lifestyle and medical history are key in deciding when to get a colonoscopy. Things like diet, exercise, smoking, and medical conditions can change a person’s risk of colorectal cancer.
“A thorough look at an individual’s risk factors, including lifestyle and medical history, is vital for personalized colonoscopy screening advice.” –
American Gastroenterological Association
Healthcare providers can give personalized advice on when to get a colonoscopy. This ensures men and women get care that fits their unique risk profiles.
Medical Organizations’ Official Guidelines
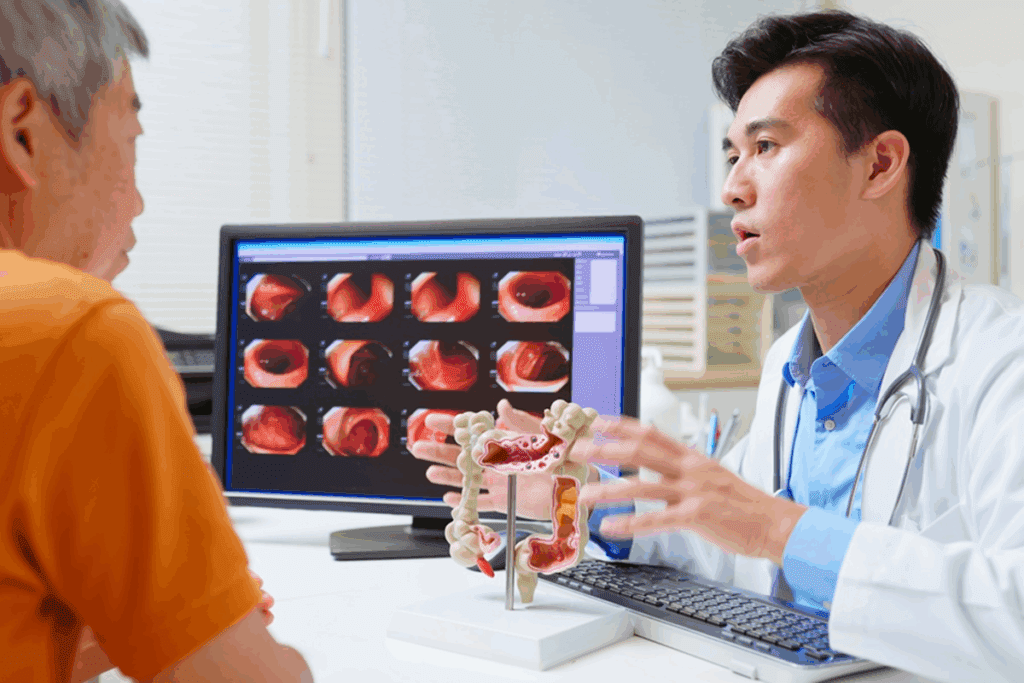
Expert groups like the American Cancer Society have set guidelines for colonoscopies. These rules help doctors and patients make smart choices about screening for colorectal cancer.
American Cancer Society Recommendations
The American Cancer Society says adults should start screening at 45 if they’re at average risk. They found that early screening can lower the risk of colorectal cancer.
They list several screening methods, with colonoscopy being a top choice. People with a family history or other risk factors might need to start screening earlier.
U.S. Preventive Services Task Force Guidelines
The U.S. Preventive Services Task Force also has guidelines. They say adults between 45 and 75 should get screened for colorectal cancer. The decision to start screening at 45 depends on your risk and what you prefer.
For those 76 to 85, the Task Force suggests making screening decisions based on your health, how long you might live, and any past screenings.
Gastroenterological Society Positions
Gastroenterological groups, like the American Gastroenterological Association, agree with the American Cancer Society and the U.S. Preventive Services Task Force. They highlight colonoscopy’s role in screening and offer advice on when to have follow-up tests.
These organizations keep updating their guidelines with new research. This ensures their recommendations are based on the best ways to fight colorectal cancer.
When Should Colonoscopies Stop? Upper Age Limits
Deciding when to stop colonoscopies is complex. As people get older, their risk for colorectal cancer goes up. But, their health can also become more complicated.
When it comes to older adults, doctors look at several things. They consider the patient’s health, how long they might live, and past screening results. Guidelines say to keep screening until age 75. After that, it depends on the person’s health and risk factors.
Guidelines for Ages 75-85
For those 76 to 85, the choice to keep screening is personal. Doctors look at the patient’s health and how long they might live. They decide if the benefits of screening are worth the risks and hassle.
Doctors consider many things, like other health issues and how well the patient can function. They also think about what the patient wants. Healthcare providers are key in helping patients make this choice. They help them see the good and bad sides based on their own situation.
Considerations for Adults Over 85
For those over 85, the decision to keep screening is based on their health and how long they might live. Often, the risks of the procedure are too high, mainly if they have other serious health problems or don’t have much time left.
But, for healthy older adults who might live a long time, screening might be a good idea. The decision should be made based on the patient’s health and what they want. This way, screening helps those who can benefit the most, without harming those who can’t.
In short, while there are guidelines for stopping colonoscopies, each person’s situation is unique. Doctors must consider the patient’s health, life expectancy, and personal wishes. This ensures that screening is both effective and right for each person.
Colonoscopy Frequency: Timing Between Screenings
The time between colonoscopies varies based on several factors. These include the first test’s results and your personal risk level. Knowing these factors helps decide how often you should get screened.
Follow-up Intervals Based on Initial Results
If your first colonoscopy shows no issues, you might wait 10 years for the next one. But, if polyps are found, you’ll need to go back sooner. This could be every 3 to 5 years, depending on the polyps’ size and type.
| Initial Colonoscopy Results | Recommended Follow-up Interval |
| No polyps or abnormalities | 10 years |
| 1-2 small (<1 cm) tubular adenomas | 7-10 years |
| 3-10 adenomas or any adenoma ≥1 cm | 3 years |
| More than 10 adenomas | 1-3 years |
Adjusting Screening Intervals as You Age
As people get older, their health and risk levels can change. This might affect how often they need colonoscopies. For those over 75, the choice to keep screening depends on their health, life expectancy, and past results.
Alternative Screening Methods and Their Timing
There are many screening tests for polyps or colorectal cancer, aside from colonoscopy. These include stool-based tests and visual exams. They offer choices for those who may not want or can’t have a colonoscopy.
Stool-Based Tests
Stool-based tests are easy and don’t hurt. They look for hidden blood or DNA changes in stool. These signs can mean colorectal cancer or polyps that could become cancer.
There are a few types of these tests:
- Fecal Occult Blood Tests (FOBT): These tests find hidden blood in the stool.
- Fecal Immunochemical Tests (FIT): FIT is more precise than FOBT and finds antibodies to human hemoglobin.
- Stool DNA Tests: These tests look for DNA changes in the stool that might show colorectal cancer.
How often you need these tests varies. For example, FIT is suggested every year. Stool DNA tests like Cologuard are recommended every three years if the first test is negative.
| Stool-Based Test | Frequency | Description |
| FIT | Annually | Detects antibodies to human hemoglobin |
| Stool DNA Test (Cologuard) | Every 3 years | Detects DNA changes indicative of colorectal cancer |
| FOBT | Annually | Detects hidden blood in the stool |
Visual Exams Beyond Colonoscopy
Visual exams are another option instead of colonoscopy. They include:
- CT Colonography (Virtual Colonoscopy): Uses CT scans to make detailed images of the colon.
- Flexible Sigmoidoscopy: Looks at the lower part of the colon.
CT colonography is suggested every five years if the first test is negative. Flexible sigmoidoscopy is done every 5-10 years, often with FIT.
Knowing when and why to use these tests is key to good health. It’s important to talk to a doctor to find the right screening plan for you. This depends on your risk and health history.
Special Population Considerations for First Colonoscopy
Some groups face higher risks that affect when they should have their first colonoscopy. While most adults should start screenings at 45, some may need to start earlier. This is because of their higher risk.
African Americans and Earlier Screening Recommendations
African Americans are at a higher risk of colorectal cancer. They tend to get diagnosed younger and have a higher death rate. Because of this, some say they should start screenings around 40-45 years old.
The American Cancer Society advises African Americans to talk to their doctor. This helps figure out the best screening schedule for them.
Other Demographic Risk Factors
Other groups also face higher risks. For example, those with a family history of colorectal cancer or certain genetic syndromes are at higher risk. Family history is a big risk factor. Guidelines suggest starting screenings 10 years before the youngest family member was diagnosed.
Also, lifestyle and environment play a role. A diet full of red and processed meats, not enough exercise, and obesity increase risk.
“A healthy lifestyle, including a balanced diet and regular physical activity, can contribute to reducing the risk of colorectal cancer.”
It’s important to understand these risk factors for the first colonoscopy. Doctors use these factors to advise on when and how often to have screenings.
Insurance Coverage and Colonoscopy Timing
Insurance coverage is key in setting when you’ll have your first colonoscopy. Knowing your insurance options is important for getting this important screening.
Health insurance plans often cover colonoscopies without a deductible or co-pay. This is thanks to the Affordable Care Act. It makes sure most plans cover screenings like colonoscopies without extra costs.
Medicare Coverage Guidelines
People 65 and older get colonoscopy coverage through Medicare. Medicare Part B pays for screenings for those at average risk every 10 years if they’re normal. Those at higher risk get screenings more often.
Even though Medicare covers a lot, you might have to pay for some extra services. This includes things like biopsies or removing polyps during the screening.
Private Insurance Policies and the Affordable Care Act
Private insurance policies can vary, but the Affordable Care Act helps. Most plans cover preventive colonoscopies without extra costs. This means you might not have to pay a deductible or co-pay for a colonoscopy, depending on your age and risk.
It’s important to check your insurance plan. This way, you’ll know about any costs for the procedure or care after it.
In summary, knowing your insurance is a big step in planning for a colonoscopy. Whether you’re on Medicare or a private plan, understanding your benefits helps you make smart health care choices.
Conclusion: Making an Informed Decision About Your First Colonoscopy
Deciding when to have a colonoscopy requires knowing the guidelines, risk factors, and insurance coverage. It’s important to talk to a healthcare provider. They can help figure out the best screening plan for you.
Looking at the latest guidelines from groups like the American Cancer Society and the U.S. Preventive Services Task Force is key. Knowing your personal risk factors, like family and medical history, is also important. These factors help guide your decision.
Choosing the right time for your first colonoscopy can greatly affect your health. It’s vital to discuss your situation with a healthcare provider. They can create a screening plan that fits your needs.
FAQ
At what age should I get my first colonoscopy if I’m at average risk?
Adults at average risk should get their first colonoscopy at 45. This is what major medical groups now suggest.
What does it mean to be at “average risk” for colorectal cancer?
Being at “average risk” means you don’t have a family history of colorectal cancer. It also means you don’t have certain genetic syndromes or other risk factors.
When should high-risk individuals start getting colonoscopies?
High-risk people, like those with a family history of colorectal cancer, should start screening early. They should do so 10 years before the relative’s diagnosis.
Are there different recommendations for men and women regarding colonoscopy timing?
Both men and women should start colonoscopies at 45, based on average risk. But, your personal risk factors and health history can change this timing.
What are the guidelines from major medical organizations regarding colonoscopy screenings?
Groups like the American Cancer Society and the U.S. Preventive Services Task Force say to start screenings at 45 for those at average risk.
At what age should colonoscopies stop?
Stopping colonoscopies depends on your health and how long you might live. Usually, they’re not needed after 75-85 years old.
How often should I get a colonoscopy?
How often you need a colonoscopy depends on the first results. If no polyps are found, you might wait 10 years. But, this can change based on your risk and past findings.
Are there alternative screening methods to colonoscopy?
Yes, there are other options like stool tests and CT colonography. These can be chosen based on your risk and what you prefer.
Do insurance plans cover colonoscopies, and are there any specific guidelines?
Most insurance, including Medicare, covers colonoscopies as recommended by major groups. But, the details can vary.
Are there special considerations for certain demographic groups regarding colonoscopy timing?
Yes, groups like African Americans might have different risk factors. This could affect when they should have their first colonoscopy.
What factors influence the decision to continue or stop colonoscopy screenings?
Decisions are based on your health, how long you might live, past results, and risk factors. Comorbid conditions also play a role.
How do I know if I’m at high risk for colorectal cancer?
High risk includes a family history of colorectal cancer, certain genetic syndromes, and other medical conditions. Talking to your doctor can help figure out your risk.
References
Dahmiwal, T., et al. (2024). Dietary considerations in cholecystectomy. Journal of Gastrointestinal Surgery, 28(5), 345-350. Retrieved from