Last Updated on December 1, 2025 by Bilal Hasdemir
Embryonic stem cells come from embryonic development stages. They are taken from embryos that are a few days old. These cells can turn into different types of cells. This makes them important for stem cell research and possible treatments.
To get embryonic stem cells, scientists take cells from the inner cell mass of a blastocyst. This is a key stage in embryonic development. It shows why knowing where embryonic stem cells come from is so important.
Key Takeaways
- Embryonic stem cells are derived from embryos several days old.
- These cells are pluripotent, able to become any cell type.
- Derivation involves extracting cells from a blastocyst’s inner cell mass.
- Embryonic stem cells are valuable for medical research and therapy.
- Understanding their origin is key for their use.
The Fundamental Nature of Embryonic Stem Cells
Embryonic stem cells can turn into any cell in the body. This makes them key in regenerative medicine and tissue engineering.
Definition and Biological Significance
These cells come from early embryos. They can grow and change into almost any cell. This is why they are called pluripotent stem cells.
They are important for studying human development and for regenerative medicine. Their ability to become different cells helps in human embryo stem cell research and understanding how we grow.
Key Characteristics of Embryonic Stem Cells
The main traits of embryonic stem cells are:
- Pluripotency: They can become every type of body cell.
- Self-renewal: They can grow without changing into different cells.
- Ability to differentiate into cells from all three germ layers: ectoderm, endoderm, and mesoderm.
These traits make embryonic cell sources very useful for research and treatments.
Comparison with Other Stem Cell Types
Embryonic stem cells differ from adult stem cells. Adult stem cells can only turn into a few cell types. But embryonic stem cells can become many different types of cells.
Compared to induced pluripotent stem cells (iPSCs), embryonic stem cells come from embryos. iPSCs are made from adult cells that are changed to be like embryonic stem cells. Both are important for regenerative medicine but in different ways.
Early-Stage Embryo Cells: Development and Origin
The early stages of an embryo’s growth are key to understanding stem cells. This time is filled with fast cell growth and changes. It sets the stage for a complex life form.
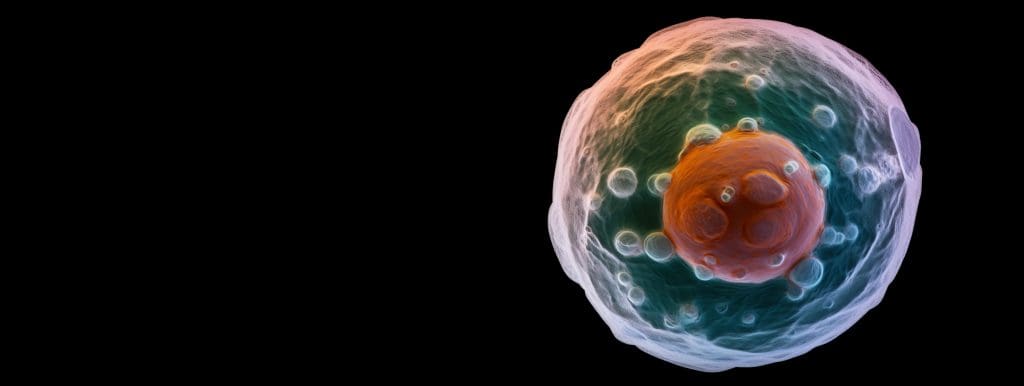
From Fertilization to Blastocyst Formation
From the start, the embryo goes through many stages. First, it’s the cleavage stage, where cells divide without growing. Then, it becomes a morula, a tight cluster of cells.
Next, the morula turns into a blastocyst through cavitation. This is when a fluid-filled space forms. The blastocyst has two main parts: the inner cell mass (ICM) and the trophectoderm. The ICM is where stem cells come from, while the trophectoderm helps make placental tissues.
Cellular Differentiation Timeline
Cell changes happen in a set order early on. At first, cells can become any cell type. Later, they can only become a few types but not a whole organism.
This order is important. It shows when cells can become stem cells.
Developmental Potentia of Early Embryonic Cells
Early embryo cells are very flexible. They can turn into many different cell types. The inner cell mass of the blastocyst is special. It’s where stem cells come from, which can grow into many cell types.
Using these cells’ abilities is important for medicine and learning about human development.
The Blastocyst Inner Cell Mass as a Primary Source
The inner cell mass in the blastocyst is a key source of embryonic stem cells. It has the ability to become any cell type. The blastocyst forms about 5-6 days after fertilization, marking a vital stage in early development.
Anatomy of the Blastocyst Structure
The blastocyst has two main parts: the trophectoderm and the inner cell mass. The trophectoderm is the outer layer, important for implantation and the placenta. On the other hand, the inner cell mass is a group of cells inside that will become the fetus.
Inner Cell Mass Composition and Properties
The inner cell mass is made up of pluripotent cells. These cells can turn into any cell type in the body. They are key for growth and have the power to form all three germ layers: ectoderm, endoderm, and mesoderm. This makes them very valuable for research and treatments.
Trophectoderm vs. Inner Cell Mass Fate
The trophectoderm and the inner cell mass have different paths in development. The trophectoderm helps form extraembryonic tissues like the placenta. In contrast, the inner cell mass is set to develop into the embryo. Knowing how these cells develop helps us understand the power of stem cells from the inner cell mass.
| Characteristics | Trophectoderm | Inner Cell Mass |
| Cell Fate | Extraembryonic tissues (e.g., placenta) | Embryo formation |
| Developmental Potentia | Limited to extraembryonic tissues | Pluripotent, capable of forming all cell types |
Embryonic Development Stages and Stem Cell Accessibility
Embryonic development stages are key to getting embryonic stem cells. The early stages before implantation are very important. How easy it is to get stem cells depends a lot on the stage of development.
Pre-implantation Embryonic Development
The embryo goes through important stages before it implants. These include fertilization, cleavage, and forming a blastocyst. The blastocyst stage is very important because it has the inner cell mass. This is where most embryonic stem cells come from.
- Fertilization: The sperm and egg come together to make a zygote.
- Cleavage: The zygote divides many times without growing much.
- Blastocyst formation: The embryo develops a fluid-filled cavity and separates into two cell groups: the inner cell mass and the trophectoderm.
Post-implantation Changes in Cell Potency
After implantation, the embryo goes through gastrulation. This is when cells start to become different types. This is a key time for setting up the body’s structure and axes.
Cells’ abilities change a lot after implantation. As the embryo grows, cells become more specialized. They lose their ability to be many things and start to do specific jobs.
Window of Opportunity for Stem Cell Derivation
The best time to get embryonic stem cells is during the pre-implantation stage, like the blastocyst stage. Getting stem cells from this stage is good because the cells are very potent and can grow a lot.
- The blastocyst stage is the best time to get stem cells.
- Cells from this stage can grow and change into many types.
- Being able to get stem cells from early embryos is very important for medicine and research.
Laboratory Isolation and Extraction Techniques
Getting embryonic stem cells from blastocysts is a detailed process. It involves several key steps. These steps help get these cells ready for research or medical use.
Blastocyst Dissection Methods
The first step is to dissect the blastocyst. This means carefully removing the trophectoderm, the outer layer. This lets us get to the inner cell mass where the stem cells are.
There are different ways to do this dissection. We use mechanical and enzymatic methods. The choice depends on what we need for our research or treatment.
Enzymatic and Mechanical Isolation Procedures
Enzymatic isolation uses trypsin to break down the blastocyst cells. This helps separate the inner cell mass from the outer layer.
Mechanical isolation, by contrast, uses physical dissection. It’s a precise method to avoid harming the cells.
Quality Assessment of Extracted Cells
After we get the cells, we check their quality. We look at their viability, ability to become many cell types, and genetic health.
We use immunofluorescence staining to see if they have the right markers. We also do karyotyping to check their genes.
It’s very important to make sure the cells are of high quality. This is true for both research and medical use.
Human Embryonic Stem Cell Sources in Modern Research
Modern research has found several key sources for human embryonic stem cells. This has changed the field of regenerative medicine a lot. These sources help us study human development and disease modeling better.
Human embryonic stem cells come from different places. This includes leftover embryos from IVF procedures and embryos made just for research. These cells have opened up new ways to understand human biology and create new treatments.
IVF-Derived Surplus Embryos
One main source of human embryonic stem cells is leftover embryos from in vitro fertilization (IVF) procedures. IVF clinics often have more embryos than needed for one treatment. With donor consent, these extra embryos can be used for stem cell research.
Getting these stem cells involves thinking about ethics and getting consent from donors. The embryos are usually at the blastocyst stage, which is best for getting stem cells.
Purpose-Created Research Embryos
At times, embryos are made just for research using IVF techniques. This lets scientists make embryos in a controlled way. It helps them get stem cells better.
These research embryos are great for studying early human development. They also help get stem cells with certain traits.
Somatic Cell Nuclear Transfer Approaches
Somatic cell nuclear transfer (SCNT) is another way to make embryonic stem cells. It involves putting an adult cell’s nucleus into an egg cell without a nucleus.
SCNT could make stem cells that match the donor’s genes. This could be good for treatments. But, this method is mostly experimental and has many technical issues.
| Source | Description | Potential Applications |
| IVF-Derived Surplus Embryos | Embryos leftover from IVF treatments | Research, disease modeling, regenerative medicine |
| Purpose-Created Research Embryos | Embryos created for research using IVF | Studying human development, deriving stem cells |
| Somatic Cell Nuclear Transfer | Nucleus transfer into an egg cell | Therapeutic applications, personalized medicine |
The variety of sources for human embryonic stem cells has greatly advanced research. It has opened up new possibilities for studying and treating diseases.
Pluripotency: The Defining Characteristic of Embryonic Stem Cells
Embryonic stem cells are special because they can become any type of body cell. This ability is key for their use in medicine and research.
Molecular Basis of Pluripotency
The molecular basis of pluripotency is complex. It involves many genetic and epigenetic factors. At the heart, it’s a network of transcription factors that keep the cell from becoming specialized.
These factors work together to stop the cell from differentiating. They also help the cell to keep dividing. This balance is essential for the cell’s pluripotent state.
Key Transcription Factors and Signaling Pathways
Important transcription factors help control pluripotency. OCT4, SOX2, and NANOG are key players. They form a network that keeps the cell in a pluripotent state.
- OCT4 is vital for keeping embryonic stem cells pluripotent.
- SOX2 works with OCT4 to control genes linked to pluripotency.
- NANOG is also essential, helping to keep the pluripotent state by regulating other genes.
Signaling pathways also play a big role. For example, the Wnt/β-catenin pathway helps keep embryonic stem cells pluripotent.
Measuring and Confirming Pluripotent Status
To check if embryonic stem cells are pluripotent, scientists use several methods. They look at the expression of specific markers like SSEA-1 or TRA-1-60. They also test if the cells can form teratomas or differentiate into different cell types.
They use techniques like quantitative PCR or RNA sequencing to check for key pluripotency genes. They also test the cells’ ability to turn into various cell types through differentiation protocols.
Establishing and Maintaining Embryonic Stem Cell Lines
Creating and keeping embryonic stem cell lines needs careful control of their culture. This is key to keep the cells in a pluripotent and stable genetic state.
Feeder Layers and Culture Requirements
Feeder layers are often used to help embryonic stem cells grow. These layers, made from mouse embryonic fibroblasts, give the cells the nutrients they need. They also help keep the cells from differentiating too early.
A study in Nature says feeder layers are vital for growing and keeping embryonic stem cells.
“The feeder layers provide a supportive environment that allows embryonic stem cells to self-renew and maintain their pluripotency.”
For embryonic stem cells to thrive, they need the right mix of growth factors, nutrients, and culture media. The exact mix can greatly affect how well the cells grow and stay stem-like.
| Culture Component | Function | Example |
| Feeder Layers | Support cell growth and maintain pluripotency | Mouse embryonic fibroblasts |
| Growth Factors | Regulate cell proliferation and differentiation | bFGF, LIF |
| Culture Media | Provide essential nutrients | DMEM/F12 |
Growth Factors and Signaling Molecules
Growth factors and signaling molecules are key in controlling embryonic stem cells. For example, basic fibroblast growth factor (bFGF) and leukemia inhibitory factor (LIF) help these cells stay in a state ready to differentiate into different cell types.
The signals from these factors keep the cells in a good state for differentiation. It’s important to understand how these signals work together to improve culture conditions for embryonic stem cell lines.
Genetic Stability Challenges in Long-term Culture
Keeping embryonic stem cell lines genetically stable over time is a big challenge. Long-term culture can cause genetic mutations. These mutations can change how the cells behave and their ability to differentiate.
Researchers have found that long-term culture can lead to genetic changes. This could make the cells less useful for treatments.
“Regular monitoring of genetic stability is critical to keep embryonic stem cell lines intact.”
To avoid these problems, it’s important to have strong quality control. This includes regular genetic checks to ensure the cells stay stable.
Alternative Sources to Traditional Embryonic Stem Cells
Traditional embryonic stem cells have their limits. This has led to the search for new stem cell sources. These alternatives are bringing fresh possibilities for treatments and research.
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells (iPSCs) are a big step forward. They turn regular cells into stem cells, like embryonic ones, without harming embryos. This breakthrough is opening doors for studying diseases, finding new drugs, and even regrowing tissues.
Key Features of iPSCs:
- Reprogrammed from somatic cells
- Pluripotent capabilities
- Potential for personalized medicine
Parthenogenetic and Androgenetic Stem Cells
Parthenogenetic stem cells come from unfertilized eggs. Androgenetic stem cells come from sperm. Both have benefits, like making stem cells that match well for transplants, reducing immune reactions.
| Stem Cell Type | Origin | Potential Applications |
| Parthenogenetic | Unfertilized eggs | Regenerative medicine, tissue engineering |
| Androgenetic | Sperm | Reproductive medicine, genetic research |
Extended PotentiaL Stem Cells
Extended potentiaL stem cells (EPSCs) have a wider range of uses than traditional stem cells. They can grow into many types of tissues. This makes them great for studying development and could lead to new treatments.
The search for new stem cell sources is changing stem cell research. These new options are helping to solve the problems of traditional stem cells. They bring new hope for medical breakthroughs and scientific discoveries.
Therapeutic Applications of Embryo-Derived Stem Cells
Embryo-derived stem cells have a wide range of uses in medicine. They can turn into many different cell types. This makes them very useful for treating various health issues.
Regenerative Medicine Approaches
Regenerative medicine aims to fix or replace damaged tissues and organs. These stem cells are being studied for their role in this field. They can become many types of cells.
Key Applications:
- Repairing damaged heart tissue
- Treating degenerative diseases such as Parkinson’s
- Replacing damaged skin
Disease Modeling and Drug Discovery
These stem cells can help model diseases in a lab. This lets researchers study how diseases progress and test new treatments. It could change how we find new medicines.
| Disease | Cell Type | Application |
| Parkinson’s | Dopaminergic neurons | Cell replacement therapy |
| Heart disease | Cardiomyocytes | Heart tissue repair |
| Diabetes | Pancreatic islet cells | Insulin production |
Tissue Engineering and Organoid Development
Tissue engineering uses stem cells to create new tissues. Organoid development makes tiny versions of organs in a lab. These areas are closely related.
Organoids could be used for many things, like studying diseases and testing drugs.
The field of organoids and tissue engineering is growing fast. It holds a lot of promise for helping people.
Ethical Considerations in Embryonic Stem Cell Research
Embryonic stem cell research raises many ethical questions. These questions involve the moral status of embryos, informed consent, and donor rights. They are complex and need careful thought.
Moral Status Debates
The moral status of embryos is a big issue. Philosophers and religious groups have different views on when life starts and what rights embryos have.
“The question of whether an embryo is a person with rights is a deeply philosophical and religious one, with different cultures and individuals holding diverse views.”
People debate if embryos can grow into humans and if it’s right to use them for research.
Informed Consent and Donor Rights
Donors must give informed consent. They need to know how their embryos will be used and the ethical issues involved.
| Key Elements of Informed Consent | Description |
| Understanding of Research Purpose | Donors should understand the goals and outcomes of the research. |
| Awareness of Risks and Benefits | Donors should know the risks and benefits of the research. |
| Voluntary Participation | Donors must feel free to choose without pressure. |
Religious and Cultural Perspectives
Religion and culture play big roles in this debate. Different beliefs on human life and embryo morality exist.
Alternatives like induced pluripotent stem cells (iPSCs) are being explored. They might solve some of the ethical problems.
Ethical alternatives like iPSCs are getting more attention. They could help avoid the ethical issues with embryonic stem cells.
The debate shows we need to keep talking about the ethics of embryonic stem cell research.
Regulatory Landscape for Embryonic Stem Cell Research
The rules for using embryonic stem cells in research are complex and change a lot from place to place. This shows how different people see the ethics, laws, and social views on using human embryos for science.
United States Federal and State Policies
In the U.S., the rules for stem cell research are mainly set by the federal government. But, state laws also have a big role. The Dickey-Wicker Amendment has been passed every year from 1996 on. It stops federal money from going to research that harms or destroys human embryos. Yet, it lets money go to research on stem cells from embryos that are no longer needed for making babies.
State laws are all over the map. Some places like California and New York support and fund this research. But, other states might have stricter rules.
| State | Policy on Embryonic Stem Cell Research | Funding Availability |
| California | Supportive | Available through state grants |
| New York | Supportive | Available through state grants |
| Other States | Varies | Limited or not available |
International Regulatory Frameworks
Across the world, countries have different rules for stem cell research. Some ban using human embryos for science, while others are more open to it.
The European Union’s Stem Cell Charter sets guidelines for this research, focusing on ethics. Places like the U.K. and Singapore have rules that let stem cell research happen under certain rules.
Funding Mechanisms and Limitations
Getting money for stem cell research is key to how much and what kind of research happens. In the U.S., the government can fund research on existing stem cells. But, the Dickey-Wicker Amendment stops new stem cells from getting federal money.
Private and state money help fill the gap, but they have their own limits and ethics. Working with other countries can also bring in more money. But, it’s hard because of all the different rules.
Current Research Frontiers and Technological Advances
Embryonic stem cell research is leading the way in science, thanks to gene editing and synthetic embryology. These breakthroughs help us understand how embryos develop. They also open doors to new treatments.
Single-Cell Analysis of Early Embryos
Single-cell analysis has changed the game, letting us study early embryos in great detail. It helps us find out which cells are doing what and how. This knowledge is key to understanding how cells change during development.
Single-cell RNA sequencing has been a game-changer. It gives us a look at the genes active at different stages of development. This info is vital for grasping how stem cells work and how they turn into different cell types.
Synthetic Embryology Approaches
Synthetic embryology uses stem cells to build artificial embryo models. These models help us study early development and diseases. They’re like mini-labs for understanding how embryos grow and how diseases start.
Recent breakthroughs have made it possible to build embryo-like structures. These models help us learn about important developmental steps like the formation of organs. This field could lead to new ways to treat developmental disorders and help in regenerative medicine.
Gene Editing in Embryonic Stem Cells
Gene editing, like CRISPR/Cas9, has changed embryonic stem cell research. It lets scientists make precise changes to the genome. This helps them study how genes affect development.
Gene editing in embryonic stem cells is a big deal for research and developing treatments. It lets us create disease models and study gene function. It could also lead to new gene therapies.
Biobanking and Commercialization
Biobanks for embryonic stem cells are key for research and turning discoveries into treatments. Biobanks store and share high-quality stem cell lines. These are essential for scientists.
Companies are starting to make products from embryonic stem cells, like therapies. But, there are strict rules to follow. These rules vary by country, making it tricky to navigate ethics and laws.
Conclusion: The Enduring Significance of Embryonic Stem Cell Research
Embryonic stem cell research is key to understanding how we develop and fight diseases. These cells can be grown and studied, leading to new ways to heal and understand health issues. This research is a big step forward in medicine.
This field is important because it could lead to new treatments. As scientists learn more about these cells, they can find new ways to help people. This could change how we treat many diseases.
The future of this research looks bright. Scientists are working on new ways to use these cells. They hope to make big strides in understanding and treating diseases. This could be a game-changer for medicine.
FAQ
What are embryonic stem cells and where are they derived from?
Embryonic stem cells come from the inner cell mass of a blastocyst. This is an early stage in embryonic development. They can turn into any cell type in the body.
What is the significance of embryonic stem cells in medical research?
They are key in medical research. They help in regenerative medicine, disease modeling, drug discovery, and tissue engineering.
How are embryonic stem cells isolated and extracted?
Scientists use lab techniques to get them. This involves dissecting blastocysts and checking the quality of the cells.
What is the difference between embryonic stem cells and other types of stem cells?
They differ from adult stem cells and induced pluripotent stem cells. Embryonic stem cells are more versatile and can self-renew.
What are the sources of human embryonic stem cells used in research?
They come from IVF surplus embryos, embryos made for research, and somatic cell nuclear transfer.
What is pluripotency and how is it maintained in embryonic stem cells?
Pluripotency means a cell can become any cell type. In embryonic stem cells, it’s kept by complex factors and pathways.
What are the challenges in establishing and maintaining embryonic stem cell lines?
Challenges include needing feeder layers, growth factors, and keeping genetic stability over time.
What are the alternative sources to traditional embryonic stem cells?
Alternatives include induced pluripotent stem cells, parthenogenetic and androgenetic stem cells, and extended stem cells.
What are the therapeutic applications of embryo-derived stem cells?
They have many uses. These include regenerative medicine, disease modeling, drug discovery, and tissue engineering.
What are the ethical considerations surrounding embryonic stem cell research?
Ethical debates include moral status, informed consent, donor rights, and religious and cultural views.
What is the current regulatory landscape for embryonic stem cell research?
It includes federal and state policies in the U.S. and international rules. Funding and its limits also play a role.
What are the current frontiers in embryonic stem cell research?
Frontiers include single-cell analysis, synthetic embryology, gene editing, and biobanking and commercialization implications.