Understanding haematopoiesis is key for diagnosing and treating blood disorders. At Liv Hospital, we offer top-notch, ethical care. We use the latest knowledge in hematopoietic processes.
Haematopoiesis is how hematopoietic stem cells turn into different blood cells. This complex process mainly happens in the bone marrow. There, stem cells grow into various blood cells, each with its own role.
We know how vital it is to understand blood cell lineage. This knowledge helps us create effective treatments for blood-related issues.
Key Takeaways
- Haematopoiesis is the process of blood cell formation.
- It mainly happens in the bone marrow.
- Hematopoietic stem cells turn into different blood cell types.
- Knowing blood cell lineage is key for treating blood disorders.
- Liv Hospital offers advanced care based on the latest hematopoiesis research.
Understanding Haematopoiesis: Definition and Terminology
Haematopoiesis, or hematopoiesis, is how blood cells are made. It’s a key process for keeping blood cells flowing. These cells carry oxygen, fight off infections, and help blood clot.
Various Spellings: Hematopoyesis, Hemopoiesis, Haemopoesis
In different places, haematopoiesis is spelled differently. In the U.S., it’s “hematopoiesis.” In the U.K., it’s “haemopoiesis.” You might also see “hematopoyesis” and “hemopoiesis.” But they all mean the same thing: making blood cells.
“The multiple spellings of haematopoiesis can be confusing, but they all refer to the same fundamental biological process.” It’s important to know these different spellings are just variations. They don’t show different processes but different ways of writing the same term.
The Fundamental Process of Blood Cell Formation
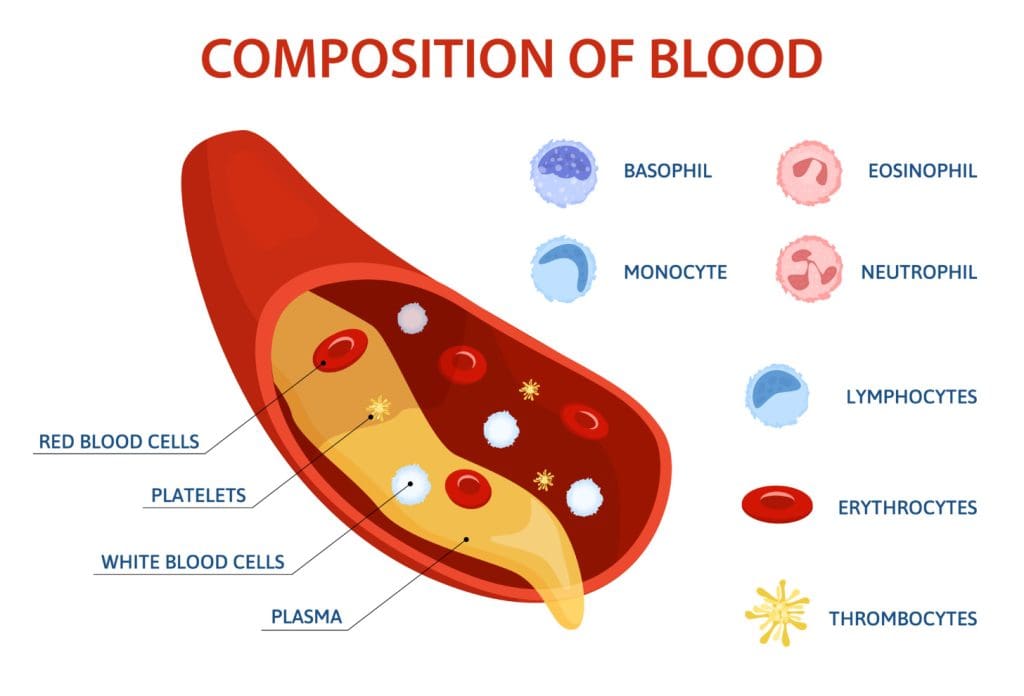
Haematopoiesis turns hematopoietic stem cells into all blood cell types. This includes red, white blood cells, and platelets. It happens mainly in the bone marrow. It’s controlled by growth factors, cytokines, and other signals.
Experts say,
“Haematopoiesis is a highly regulated process that ensures the production of blood cells according to the body’s needs.”
This control is key for staying healthy and fighting off diseases or injuries.
In short, knowing about haematopoiesis means understanding its different names and how blood cells are made. This knowledge helps us see the importance of blood cell production in health and disease.
The Biological Significance of Blood Cell Production
Haematopoiesis is key to our health. It makes blood cells needed for many body functions. This process keeps our body fighting off infections, carrying oxygen, and healing wounds.
Haematopoiesis is vital for the continuous renewal of blood components. Our blood cells don’t live forever and need to be replaced. For example, red blood cells last about 120 days, and platelets only 8-12 days. This constant replacement is essential for our circulatory system’s health.
Continuous Renewal of Blood Components
Haematopoiesis ensures our blood cells are always fresh. This is critical for our body’s optimal function. Here are some important points:
- Red blood cells are made at a rate of about 2 million per second to replace old or damaged ones.
- Platelets are produced in large numbers to keep our blood vessels strong.
- White blood cells are made to fight infections and support our immune system.
Maintaining Homeostasis Through Haematopoiesis
Haematopoiesis is vital for homeostasis. It controls the production of different blood cells. This lets our body respond well to various demands and stressors. For instance, it can boost white blood cell production during infections.
Volume and Rate of Blood Cell Production
The amount and rate of blood cell production are carefully controlled. Normally, the bone marrow makes billions of blood cells every day. But, this can jump up during conditions like anemia or infection.
For example, during hard exercise or at high altitudes, the body makes more red blood cells. This shows how haematopoiesis can adapt to our needs.
Where Does Haematopoiesis Occur in the Human Body?
Haematopoiesis mainly happens in the bone marrow. But, the places involved change as we grow. From embryos to adults, the body’s needs change, so the sites for blood cell production adapt.
Primary Sites of Blood Cell Formation
In the human body, haematopoiesis takes place in various organs at different life stages. At first, the yolk sac is where blood cell formation begins in the fetus.
As the fetus grows, other organs like the liver take over. Later, the bone marrow becomes the main site for blood cell production.
Developmental Changes in Haematopoietic Locations
During embryonic development, haematopoiesis moves through different sites. It starts in the yolk sac, then moves to the liver, and eventually to the bone marrow.
This change is key for the body’s growing needs. It allows for the right production of blood cells.
The following table summarizes the primary sites of haematopoiesis at different developmental stages:
| Developmental Stage | Primary Site of Haematopoiesis |
|---|---|
| Embryonic | Yolk Sac |
| Fetal | Liver |
| Adult | Bone Marrow |
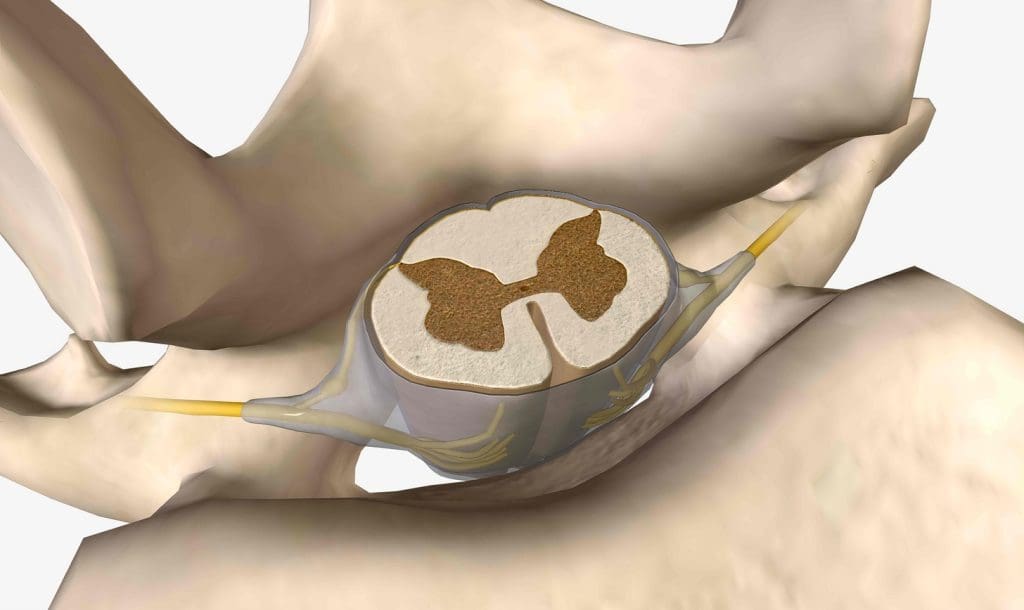
The Bone Marrow as the Central Hub
In adults, the bone marrow is the primary site for haematopoiesis. It produces all blood cells, including red and white blood cells, and platelets.
The bone marrow’s structure and cells help hematopoietic stem cells become mature blood cells.
In conclusion, haematopoiesis happens in different places as we develop. The bone marrow is the main site in adults.
Bone Marrow Architecture and Function
It’s important to know how bone marrow works to understand blood cell creation. Bone marrow is a special organ that makes all blood cells. It’s key to haematopoiesis, the process of making blood cells.
Structure and Composition of Bone Marrow
Bone marrow is inside bones and has blood vessels, stromal cells, and developing blood cells. The stromal cells help build the structure and support blood cell growth. “The bone marrow microenvironment is a critical regulator of haematopoiesis,” experts say.
Haematopoiesis is tightly regulated by the bone marrow microenvironment, which includes a complex interplay of cellular and molecular components.
The marrow also has many blood vessels. These vessels bring nutrients and oxygen for blood cell production.
Red vs. Yellow Marrow: Distribution and Roles
Bone marrow is divided into red and yellow types. Red marrow is in the pelvis, vertebrae, sternum, and skull in adults. It’s full of cells that make blood. Yellow marrow is mostly fat and less active in making blood. It’s in the long bones.
Vascular Network Supporting Haematopoiesis
The bone marrow’s blood vessels are key for making blood cells. The sinusoidal capillaries help exchange nutrients, waste, and blood cells. This network keeps blood cells healthy.
In short, bone marrow’s structure and function are vital for blood cell creation. Knowing about bone marrow’s parts and how they work helps us understand blood cell production.
Age-Dependent Haematopoietic Sites
As we grow, where blood cells are made changes a lot. This ensures blood cell production stays efficient at all ages.
Fetal Haematopoiesis: Liver and Spleen
In the womb, blood cells are mainly made in the liver and spleen. The liver is key in the second trimester, with the spleen helping too. This early blood cell production is vital for the fetus’s growth and oxygen supply.
Pediatric Haematopoiesis: Long Bones Like the Femur
After birth, blood cell making moves to the bone marrow. In kids, long bones like the femur are important for this. As kids grow, these bones’ marrow gets busier making blood cells.
Adult Haematopoiesis: Pelvis, Vertebrae, Sternum, and Cranium
In adults, blood cell making happens mainly in the pelvis, vertebrae, sternum, and cranium. The marrow in these areas makes all blood cell types. This setup helps keep blood cell production efficient and balanced.
The change in where blood cells are made from fetus to adult shows how complex and well-regulated blood cell production is. Knowing about these changes helps us understand the importance of haematopoiesis in keeping us healthy throughout our lives.
Hematopoietic Stem Cells: The Foundation of Blood Cell Development
Hematopoietic stem cells are at the core of blood cell creation. They are vital for keeping blood cells fresh and balanced throughout our lives.
Characteristics and Properties of HSCs
HSCs have key traits that help them do their job. Self-renewal lets them keep their numbers steady while making more specialized cells. They also have a quiescence mode, which helps them avoid overgrowth and keeps them healthy.
- Ability to differentiate into all blood cell lineages
- Capacity for self-renewal to maintain stem cell populations
- Quiescence, or the ability to enter a dormant state
Self-Renewal and Quiescence Mechanisms
The ways HSCs renew themselves and stay dormant are complex. They involve both what’s inside the cell and signals from outside. Knowing how this works helps us understand blood cell issues.
Recent research shows how important certain signals and cell talks are. For example, Wnt/β-catenin and Notch help control HSC self-renewal.
Differentiation and Cellular Decisions
HSCs can turn into any blood cell type, including myeloid and lymphoid. What decides their path is a mix of what’s inside them and signals from outside.
Grasping these choices is key for new treatments. Knowing how HSCs are controlled can help us make more or less of certain blood cells.
The Organization of Blood Cell Lineages
It’s important to know how blood cell lineages are organized. This helps us understand how blood cells are made. The process is complex, with a structure that keeps producing different blood cells.
The Hematopoietic Hierarchy Explained
The hematopoietic hierarchy starts with hematopoietic stem cells (HSCs) at the top. These stem cells can make all blood cell types. They can also keep themselves going. The hierarchy looks like a tree, with HSCs branching into different cells, which then become mature blood cells.
Hematopoietic Hierarchy Structure:
| Cell Type | Description | Function |
|---|---|---|
| Hematopoietic Stem Cells (HSCs) | Self-renewing stem cells | Give rise to all blood cells |
| Multipotent Progenitor Cells | Cells with limited self-renewal | Differentiate into various blood cell lineages |
| Lineage-Restricted Progenitors | Cells committed to specific lineages | Produce specific types of blood cells |
| Mature Blood Cells | Fully differentiated cells | Perform specific functions in the body |
Interpreting Hematopoiesis Charts and Diagrams
Hematopoiesis charts and diagrams help us understand blood cell formation. They show the stages from HSCs to mature blood cells. These visual aids help researchers and doctors understand how blood cells are made.
Key Regulatory Checkpoints in Differentiation
The process of turning HSCs into mature blood cells is carefully controlled. Several key points ensure it happens right. These include controlling genes, signaling pathways, and the bone marrow environment.
- Transcription Factors: Proteins that control gene expression, determining cell fate.
- Signaling Pathways: Complex pathways that respond to external signals, influencing cell behavior.
- Bone Marrow Microenvironment: The niche that supports HSCs and progenitor cells, providing necessary signals for hematopoiesis.
Understanding these checkpoints is key to learning about hematopoiesis. It also helps in finding new treatments for blood disorders.
Myeloid and Lymphoid Pathways: From Stem Cells to Mature Blood Cells
Hematopoietic stem cells start their journey to become mature blood cells through the myeloid and lymphoid pathways. They split into two main groups: myeloid and lymphoid. These groups then grow into different types of blood cells. Knowing about these pathways helps us understand how blood cells are made and how they develop.
Myeloid Lineage: Erythrocytes, Granulocytes, Monocytes, and Platelets
The myeloid lineage creates important blood cells like red blood cells, neutrophils, eosinophils, basophils, monocytes, and platelets. These cells are key for carrying oxygen, fighting infections, and stopping bleeding.
The myeloid lineage is vital for keeping the body balanced and fighting off infections or injuries. Its development is controlled by special proteins and growth factors. This ensures the right amount of these cells is made.
Lymphoid Lineage: B Cells, T Cells, and NK Cells
The lymphoid lineage makes lymphocytes, which include B cells, T cells, and NK cells. These cells are essential for the immune system. B cells make antibodies, T cells fight infected cells, and NK cells quickly respond to viruses and tumors.
The growth of lymphoid cells involves many transcription factors and signaling pathways. This complex process guides their development and maturation. For more on what starts hematopoiesis, check out this link.
Transcription Factors Determining Cell Fate
Transcription factors are key in deciding the fate of hematopoietic stem cells and their offspring. They control the genes needed for stem cells to turn into different blood cell types.
Managing transcription factors is a complex task. It requires a fine balance to ensure blood cells develop and work correctly. Understanding these processes can help us find causes of blood disorders and new treatments.
Extramedullary Haematopoiesis: When Blood Cells Form Outside the Marrow
In some cases, the body makes blood cells outside the marrow. This can happen for good reasons or because of illness. It shows how the body can adapt to different situations.
Physiological vs. Pathological Extramedullary Haematopoiesis
There are two kinds of extramedullary haematopoiesis. The normal kind happens in babies, where the liver and spleen make blood cells. After birth, the bone marrow takes over this job. The other kind is linked to diseases, like myeloproliferative neoplasms, where the bone marrow can’t make enough blood cells.
It’s important to know the difference between these two kinds. The normal kind is part of growing up. But the disease kind means there’s something wrong that needs to be fixed.
Common Sites: Liver, Spleen, and Lymph Nodes
The liver, spleen, and lymph nodes are where blood cells can form outside the marrow. In babies, the liver is the main place for this. In adults, if it happens because of disease, the spleen and liver get bigger. Lymph nodes can also be involved, but it’s less common.
| Organ | Role in Extramedullary Haematopoiesis |
|---|---|
| Liver | Primary site during fetal development; can be involved in pathological extramedullary haematopoiesis |
| Spleen | Often involved in pathological extramedullary haematopoiesis, leading to splenomegaly |
| Lymph Nodes | Less common site, but can be involved in certain pathological conditions |
Clinical Implications and Detection Methods
The effects of extramedullary haematopoiesis depend on if it’s normal or caused by disease. Disease-related cases can harm organs by filling them with blood cells. Doctors use ultrasound, CT scans, and MRI to find it. They also take biopsies of affected organs.
To deal with extramedullary haematopoiesis, doctors use tests, imaging, and biopsies. Knowing why it happens helps figure out how to treat it.
The Bone Marrow Microenvironment: Orchestrating Blood Cell Production
Understanding the bone marrow microenvironment is key to knowing how blood cells are made. This area, also called the niche, supports hematopoietic stem cells (HSCs) to work right. It’s a complex mix of cells and molecules that help control blood cell creation.
Cellular Components of the Bone Marrow Niche
The bone marrow niche has several important cells, including:
- Osteoblasts and osteoclasts, vital for bone changes and HSC control.
- Endothelial cells, which line blood vessels and aid in HSC upkeep.
- Stromal cells, like CXCL12-abundant reticular (CAR) cells, key for HSC signals.
- Immune cells, such as macrophages and regulatory T cells, for immune balance.
These cells interact with HSCs and their descendants, shaping their actions and destiny.
Molecular Signals Regulating HSC Function
Signals in the bone marrow microenvironment are vital for HSC control. Important pathways include:
- The CXCL12/CXCR4 axis, key for HSC staying and finding their way.
- The Notch signaling pathway, affecting HSC self-renewal and change.
- The Wnt/β-catenin pathway, managing HSC growth and survival.
- The transforming growth factor-beta (TGF-β) signaling pathway, controlling HSC quietness and action.
These signals are carefully managed and work together to keep haematopoiesis in balance.
Recent Advances from Single-Cell and Imaging Studies
New single-cell analysis and imaging methods have greatly improved our understanding of the bone marrow microenvironment. Single-cell RNA sequencing has shown HSC and their descendants’ diversity. Advanced imaging lets us see HSC niches live.
These studies have given us new insights into the bone marrow’s complex interactions. They’ve shed light on how HSCs work and blood cell creation.
As we dive deeper into the bone marrow microenvironment, we’ll likely find new ways to treat blood disorders.
Conclusion: The Remarkable Journey of Blood Cell Formation
We’ve looked into haematopoiesis, a key process in the bone marrow. Here, hematopoietic stem cells turn into different blood cells. This is vital for keeping our blood cells fresh and balanced.
The path of blood cell creation is truly amazing. It starts with stem cells and ends with mature blood cells in our bodies. Haematopoiesis shows how complex and precise our biology is.
Knowing about haematopoiesis helps us understand blood disorders better. It also guides us in creating new treatments. As we learn more, we can improve care for patients with blood-related illnesses.
What is haematopoiesis?
Haematopoiesis is the process of making blood cells. It starts with hematopoietic stem cells turning into different types of blood cells. These include red blood cells, white blood cells, and platelets.
Where does haematopoiesis occur in adults?
In adults, haematopoiesis mainly happens in the bone marrow. This is found in the pelvis, vertebrae, sternum, and cranium.
What is the role of hematopoietic stem cells in haematopoiesis?
Hematopoietic stem cells (HSCs) are key in blood cell development. They can renew themselves and turn into all types of blood cells. This ensures blood cells keep being made.
How does haematopoiesis change during development?
Haematopoiesis changes location as we grow. In fetuses, it’s in the liver and spleen. In kids, it’s also in long bones. As we get older, it mainly happens in the bone marrow.
What is the difference between red and yellow marrow?
Red marrow makes blood cells, while yellow marrow stores fat. The amount of each changes with age.
What is extramedullary haematopoiesis?
Extramedullary haematopoiesis is when blood cells are made outside the bone marrow. It can happen in the liver, spleen, or lymph nodes. It’s a normal response or can be a sign of disease.
How is haematopoiesis regulated?
Haematopoiesis is controlled by many factors in the bone marrow. These include cells, signals, and genes. They work together to make the right amount of blood cells.
What is the significance of haematopoiesis?
Haematopoiesis is vital for keeping blood cells fresh. It helps with oxygen transport, fighting infections, and blood clotting. It keeps our body balanced.
How do hematopoiesis charts and diagrams illustrate blood cell development?
Charts and diagrams show how blood cells are made. They show the steps from hematopoietic stem cells to mature blood cells.
What are the myeloid and lymphoid pathways in haematopoiesis?
The myeloid pathway makes erythrocytes, granulocytes, monocytes, and platelets. The lymphoid pathway makes B cells, T cells, and NK cells. Both start from hematopoietic stem cells.
- PMC (National Center for Biotechnology Information). (n.d.). [Article title from PMC7769132]. PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7769132/
- Leukaemia Foundation. (n.d.). The bone marrow & blood formation. Leukaemia.org.au. Retrieved October 10, 2025, from https://www.leukaemia.org.au/blood-cancer/understanding-your-blood/bone-marrow-and-blood-formation/
- Wikipedia. (n.d.). Haematopoiesis. Wikipedia. Retrieved October 10, 2025, from https://en.wikipedia.org/wiki/Haematopoiesis
- Histology Guide. (n.d.). Hematopoiesis (Slidebox series). HistologyGuide.com. Retrieved October 10, 2025, from https://histologyguide.com/slidebox/08-hematopoiesis.html




































