Last Updated on October 20, 2025 by
Hematopoiesis is how all blood cells are made. It’s a key function that starts before we’re born and keeps going all our lives. In adults, this mainly happens in the bone marrow. Here, hematopoietic stem cells turn into different types of blood cells.
The bone marrow is a complex place. It has many cell interactions and molecular signals that control hematopoiesis. Knowing about this process is very important for treating blood diseases. It offers deep insights into the molecular steps of this process. At Liv Hospital, we know how serious this condition is. We offer top-notch care through our advanced hematology services.

Hematopoiesis is how our bodies make the different blood cells we need to live. It’s a vital process for keeping our blood cell counts healthy. Knowing about hematopoiesis helps us understand how our bodies work.
The term hematopoiesis comes from Greek words: “Haîma” for blood and “PoiĞ“sis” for making. It’s about creating all blood cell types, like red and white blood cells, and platelets. This complex process starts with hematopoietic stem cells turning into different blood cell types. For more on what starts hematopoiesis, check out this resource.
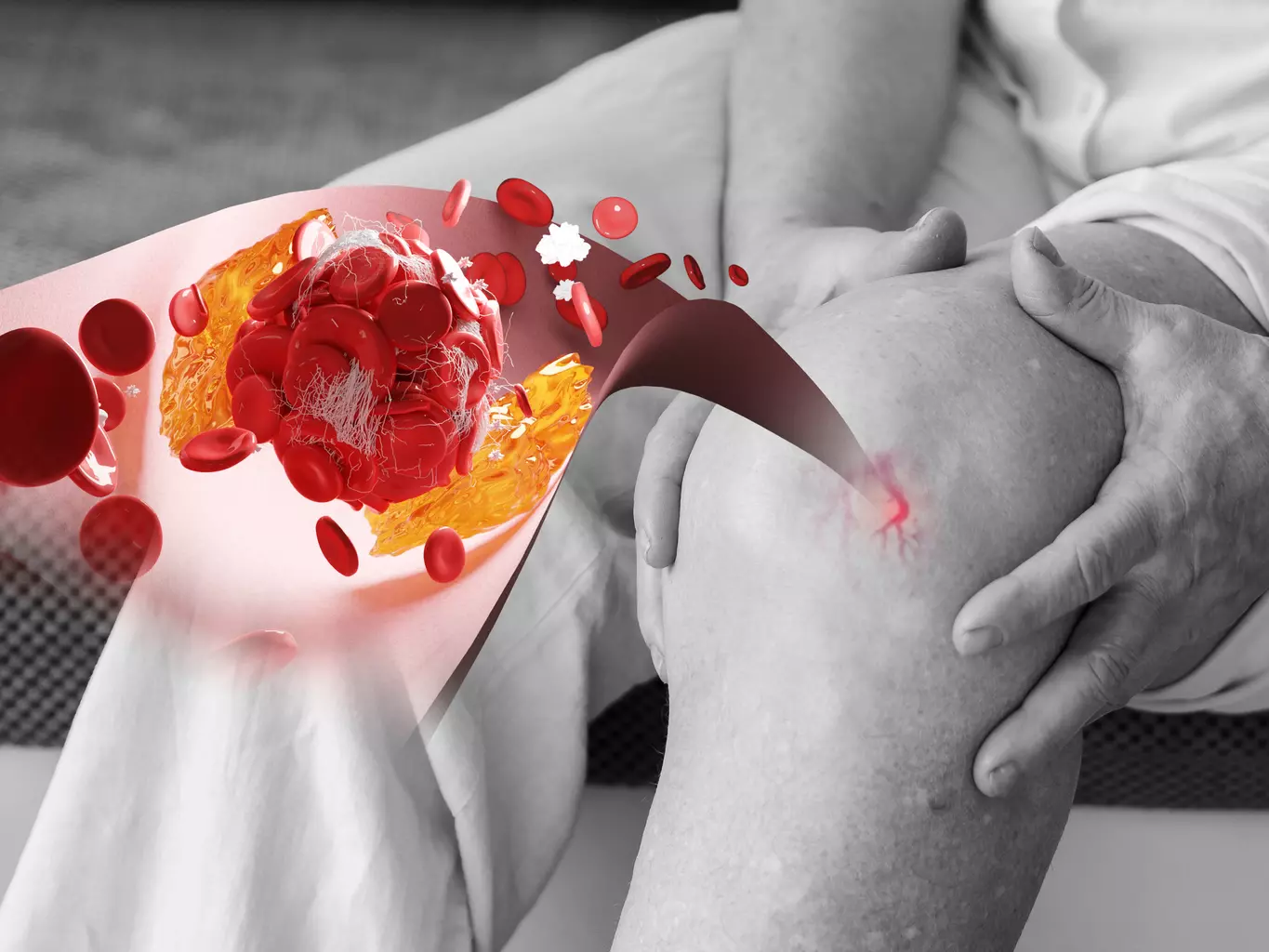
Hematopoiesis is very important for adults’ health. It helps replace old or damaged blood cells. This is key for carrying oxygen, fighting infections, and healing wounds. Problems with hematopoiesis can cause issues like anemia, infections, and bleeding disorders.
In adults, hematopoiesis happens mainly in the bone marrow. This is the spongy tissue inside some bones. The bone marrow has stem cells that can become any blood cell type. Keeping hematopoiesis in check involves many growth factors and signals.
Knowing where and how hematopoiesis works is key for diagnosing and treating blood cell issues. By understanding hematopoiesis, we can tackle blood-related diseases better. It shows how important it is to keep our blood-making system healthy.
Hematopoiesis changes a lot from when we’re in the womb to when we’re grown up. As we grow, how our body makes blood cells changes too. This change is key to keeping our blood system healthy.
In the womb, blood cell making happens in different places. First, it’s in the yolk sac, then the liver, and lastly in the bone marrow. When we’re born, it mainly happens in the bone marrow of certain bones.
The way we make blood cells changes a lot from being a fetus to being an adult. Knowing these changes helps us understand how complex blood cell making is. As we grow up, where and how we make blood cells changes a lot, ending up in the pelvis, vertebrae, sternum, ribs, and skull.
In adults, blood cell making happens mainly in the pelvis, vertebrae, sternum, ribs, and skull. This change is key to keep making blood cells as adults. The bone marrow in these bones creates a special place for blood cells to grow. This ensures we always have enough blood cells.
Here’s a comparison of the key aspects of fetal and adult hematopoiesis:
| Aspect | Fetal Hematopoiesis | Adult Hematopoiesis |
|---|---|---|
| Primary Sites | Yolk sac, liver, bone marrow | Pelvis, vertebrae, sternum, ribs, skull |
| Main Location at Maturity | Bone marrow | Bone marrow |
| Cell Production Focus | Supports fetal development | Maintains adult blood cell needs |
Understanding how hematopoiesis changes from being a fetus to an adult shows us how complex making blood cells is.
In conclusion, hematopoiesis changes a lot from being a fetus to an adult. This complex process is vital for keeping our blood system healthy throughout our lives.
Hematopoiesis, or the making of blood cells, happens in certain bone marrow areas in adults. We’ll look at where this process mainly takes place. We’ll also see the difference between red and yellow marrow and the main and secondary sites.
Bone marrow is divided into red and yellow types. Red marrow is where blood cells are made, filled with blood vessels and many cells. On the other hand, yellow marrow is mostly fat and doesn’t make blood cells. In adults, red marrow is mostly in the pelvis, vertebrae, sternum, ribs, and skull.
The main places for making blood cells in adults are the pelvis, vertebrae, sternum, ribs, and skull. These bones have red marrow, which makes blood cells. The pelvis is very important because it has a lot of red marrow. The vertebrae also have a big role, with lots of surface area for making blood cells.
Other important places are the sternum and ribs, full of red marrow. The skull is also a key place, with hematopoiesis happening in the diploë, the space between the inner and outer tables of the cranial bones.
There are also secondary sites for making blood cells in adults. These sites can become active when the body needs more blood cells. The long bones of the arms and legs usually have yellow marrow but can turn to red marrow when needed.
For more on where hematopoietic stem cells are found, check out resources like this one.
In summary, in adults, making blood cells mainly happens in the red marrow of the pelvis, vertebrae, sternum, ribs, and skull. Knowing about red and yellow marrow and the main and secondary sites helps us understand how blood cells are made.
Hematopoiesis happens in the bone marrow. It’s a place where blood cells are made. The bone marrow is full of life, helping blood cells grow from stem cells.
We’ll look at what makes up this special place. We’ll see how it helps blood cells grow.
The bone marrow has many parts that help it work. These parts include:
The bone marrow is full of different cells. These include stem cells and other cells that help blood cells grow.
| Cell Type | Function in Hematopoiesis |
|---|---|
| Hematopoietic Stem Cells | They can grow and become any blood cell type. |
| Mesenchymal Stem Cells | They help by giving out growth factors and cytokines. |
| Osteoblasts | They help control the niche through cell interactions. |
Understanding the bone marrow is key to seeing how blood cells are made. The mix of its parts and cells creates a special place for blood cell production.
Hematopoietic stem cells are at the core of blood cell creation. They have the power to renew themselves and turn into different types of blood cells. This process is vital for making all blood cells throughout our lives.
HSCs have special traits that help keep the blood system working. They can self-renew, keeping a steady supply of stem cells. They also differentiate into various blood cell types. This is key for blood cell production and keeping the system balanced.
The key features of HSCs include:
HSCs can renew themselves, keeping their numbers steady. They can also turn into all mature blood cell types. This balance is carefully managed to ensure proper blood cell creation.
Turning into different blood cells is a complex process. It’s guided by signals and rules. HSCs first become progenitor cells, then mature into specific blood cell types, like myeloid and lymphoid.
Blood cell development from HSCs follows a clear structure. HSCs are at the start, giving rise to multipotent progenitor cells. These cells then become more specific progenitors, eventually leading to mature blood cells.
| Cell Type | Description | Function |
|---|---|---|
| Hematopoietic Stem Cells (HSCs) | Self-renewing cells that give rise to all blood cell types | Maintain hematopoiesis |
| Multipotent Progenitor Cells | Cells that have lost self-renewal capacity but can differentiate into multiple lineages | Give rise to various blood cell types |
| Lineage-Restricted Progenitors | Cells committed to specific blood cell lineages | Produce mature blood cells of specific types |
| Mature Blood Cells | Fully differentiated cells performing specific functions | Carry out various physiological roles |
Understanding the hierarchy of hematopoietic cell development is key. It shows how blood cells are made and regulated. The complex relationship between HSCs, progenitor cells, and mature blood cells ensures a constant supply of blood cells for health.
Understanding hematopoiesis is key to grasping blood cell production. It’s a complex process where stem cells turn into different blood cells. These cells then move into the bloodstream.
Blood cell development has several stages. It starts with hematopoietic stem cells. These cells can renew themselves and turn into different blood cells.
Hematopoietic stem cells turn into two main types: myeloid and lymphoid. The myeloid lineage makes red blood cells, platelets, and more. The lymphoid lineage creates lymphocytes, like B cells and T cells.
Growth factors and cytokines guide these cells to develop. For example, erythropoietin helps make red blood cells. Granulocyte-colony stimulating factor (G-CSF) helps make granulocytes.
As blood cells mature, they change to do their jobs. Once mature, they enter the bloodstream. There, they help keep the body balanced, fight infections, and carry oxygen.
Hematopoiesis is carefully controlled to make the right blood cells. If it’s not, it can cause blood disorders. This shows how important this process is.
Hematopoiesis is the process of making blood cells. It’s a complex process that keeps our blood cells fresh throughout our lives.
Growth factors and cytokines are key players in hematopoiesis. They send signals that help blood cells grow, change, and stay alive. Some important ones are:
Transcription factors are proteins that control gene activity. In hematopoiesis, they guide stem cells to become different blood cell types. Important ones include:
These factors work together to decide the fate of blood cells.
Epigenetic changes, like DNA methylation and histone modifications, also play a big role. They affect gene activity without changing the DNA. For example:
These controls are vital for blood cells to function right.
In summary, hematopoiesis is a complex process. It involves growth factors, cytokines, transcription factors, and epigenetic changes. Knowing about these helps us understand how blood cell production works and what can go wrong.
Hematopoiesis happens in the hematopoietic niche, a place with many cell types working together. It’s not just a space; it helps control the growth, change, and survival of blood cells. This is done through complex cell talks and signals.
Mesenchymal stem cells (MSCs) are key in the hematopoietic niche. They make many growth factors and other important stuff that help blood cells. MSCs help keep HSCs in a state of rest and self-renewal, making sure we always have enough blood cells.
MSCs talk to HSCs in two ways: by touching each other and by sending out signals. For example, they make stromal cell-derived factor 1 (SDF-1), which helps HSCs stay in the niche as studies have found.
Endothelial cells line the blood vessels in the bone marrow. They play a big role in blood cell making. They make things like vascular endothelial growth factor (VEGF), which helps blood vessels grow and supports the niche.
Endothelial cells and HSCs talk to each other in both ways. Endothelial cells help HSCs, and HSCs can also change how endothelial cells work. This creates a reciprocal regulatory loop that keeps the niche balanced.
Osteoblasts and osteoclasts are important in bone remodeling, which is linked to blood cell making. Osteoblasts help make the niche for HSCs. They make things like osteopontin and angiopoietin-1, which help HSCs stick and survive.
Osteoclasts, on the other hand, break down bone. Their work can change the niche by releasing stored factors, affecting HSCs. The right balance between osteoblasts and osteoclasts is key for a healthy niche and blood cell making.
In summary, the hematopoietic niche is a complex place where many cells work together for blood cell production. Knowing how these cells interact is important for finding new treatments for blood-related diseases.
When hematopoiesis is disrupted, it can cause many blood and bone marrow disorders. Hematopoiesis is how blood cells are made. Problems in this process can lead to health issues, affecting blood cell production.
Bone marrow failure syndromes happen when the bone marrow can’t make enough blood cells. This results in anemia, infections, and bleeding disorders because of a lack of red and white blood cells and platelets.
Examples include aplastic anemia and myelodysplastic syndromes. These can be caused by toxins, certain drugs, and viruses.
Hematologic malignancies are cancers of the blood and bone marrow. These include leukemia, lymphoma, and multiple myeloma. Disrupted hematopoiesis can cause these cancers by letting abnormal blood cells grow too much.
The exact causes of these cancers are not fully known. They are thought to come from a mix of genetics and environment.
Diagnosing these disorders involves tests like blood counts, bone marrow biopsies, and genetic testing. Knowing the cause is key to finding the right treatment.
Treatment options depend on the condition. They can include medications, blood transfusions, and bone marrow transplantation. Sometimes, chemotherapy or radiation therapy is needed to fight cancer.
Hematopoiesis is a complex process that’s vital for making blood cells. We’ve learned it mainly happens in the bone marrow of the pelvis, vertebrae, sternum, ribs, and skull. Knowing where it happens helps us understand how blood cells are made and why it’s key for adult health.
The process of hematopoiesis is tightly controlled by growth factors, cytokines, and cell interactions. We’ve discovered that it takes place in specific areas. Problems with this process can cause disorders like bone marrow failure and blood cancers.
Understanding hematopoiesis and where it happens shows its importance for adult health. It’s a question that’s essential to answer. We’ve found that it mainly happens in the bone marrow.
Hematopoiesis is the process of making blood cells. In adults, it mainly happens in the bone marrow of certain bones. These include the pelvis, vertebrae, sternum, ribs, and skull.
It’s the process where stem cells turn into all blood cells. This includes red blood cells, white blood cells, and platelets.
It’s a complex process. Hematopoietic stem cells grow and change into different blood cells. This is all thanks to molecular signals, growth factors, and cytokines.
In the womb, it happens in different places. First, in the yolk sac, then in the liver, and later in the bone marrow.
In adults, red marrow is key for making blood cells. Yellow marrow, on the other hand, is full of fat and doesn’t make blood cells.
In adults, the main places for making blood cells are the pelvis, vertebrae, sternum, ribs, and skull. These areas have red marrow.
Knowing about hematopoiesis helps us deal with blood disorders. It’s important for finding new treatments and improving care.
It’s controlled by many molecular signals. These include growth factors, cytokines, and transcription factors. They help stem cells grow and change into blood cells.
These cells can make more of themselves and turn into all blood cells. They’re vital for keeping our blood healthy.
It’s the order in which blood cells develop. It starts with stem cells and goes through many stages to become mature blood cells.
If hematopoiesis goes wrong, it can cause blood disorders. This includes bone marrow failure and diseases like leukemia and lymphoma.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!