Last Updated on November 27, 2025 by Bilal Hasdemir

Choosing the right treatment for LAD blockage is key for heart health. At Liv Hospital, we help our patients decide between bypass surgery and stents. We focus on our patients and follow international standards.
For those with coronary artery disease, stents and CABG are proven treatments. We’ve seen success with patients like Mr. Bambang Budianto, thanks to good cardiac care.
It’s important to know the differences between these treatments. We’ll talk about the benefits and things to consider for each. Our aim is to give a fair view, using medical knowledge and patient stories to help make choices.
Key Takeaways
- Both stents and CABG are viable options for treating LAD blockage.
- The choice between bypass surgery and stents depends on individual patient needs.
- Liv Hospital offers a patient-centered approach to cardiac care.
- Understanding the differences between treatments is vital for informed decision-making.
- Proper cardiac care and treatment can lead to successful management of heart conditions.
Understanding LAD Blockage and Its Significance

The Left Anterior Descending Artery (LAD) is known as the “widowmaker” because of its severe blockage effects. It’s a key artery that supplies blood to the heart. Knowing its role is key to understanding how coronary artery disease affects the heart.
What is the Left Anterior Descending Artery?
The Left Anterior Descending Artery is a major branch of the left coronary artery. It runs down the heart’s anterior wall towards the apex. It supplies blood to a big part of the heart muscle, including the anterior wall, apex, and parts of the lateral wall. Its blockage is dangerous because it affects a large area of the heart.
How LAD Blockages Develop
LAD blockages happen when plaque builds up inside the artery. This plaque is made of fat, cholesterol, and other substances. Atherosclerosis, the buildup of plaque, can narrow or block the LAD. High blood pressure, high cholesterol, smoking, and diabetes can all contribute to this.
Symptoms and Diagnosis of LAD Blockage
Symptoms of LAD blockage include chest pain, shortness of breath, and heart attack in severe cases. Tests like electrocardiograms (ECG), stress tests, and coronary angiography help diagnose it. Knowing these symptoms and how to diagnose them is key for timely treatment.
| Diagnostic Method | Description | Use in LAD Blockage |
|---|---|---|
| Electrocardiogram (ECG) | Measures the electrical activity of the heart | Initial assessment of heart function and detection of ischemia or infarction |
| Stress Test | Evaluates heart function under stress, typically through exercise | Assesses the presence and severity of coronary artery disease |
| Coronary Angiography | Involves injecting a contrast agent into the coronary arteries to visualize them on an X-ray | Provides detailed images of the LAD and other coronary arteries, helping to identify blockages |
Understanding the LAD’s anatomy and function, how blockages develop, and how to diagnose them is vital. It helps both patients and healthcare providers deal with coronary artery disease better. This knowledge leads to better treatment decisions.
Common LAD Blockage Treatment Options

There are several ways to treat LAD blockage, each with its own benefits and drawbacks. The right treatment depends on the blockage’s severity, the patient’s health, and their medical history.
Coronary Artery Bypass Grafting (CABG)
CABG is a surgery that bypasses the blocked LAD with a graft. This method is known for its long-term success in treating complex LAD disease. It has been shown to reduce the need for more surgeries compared to other treatments.
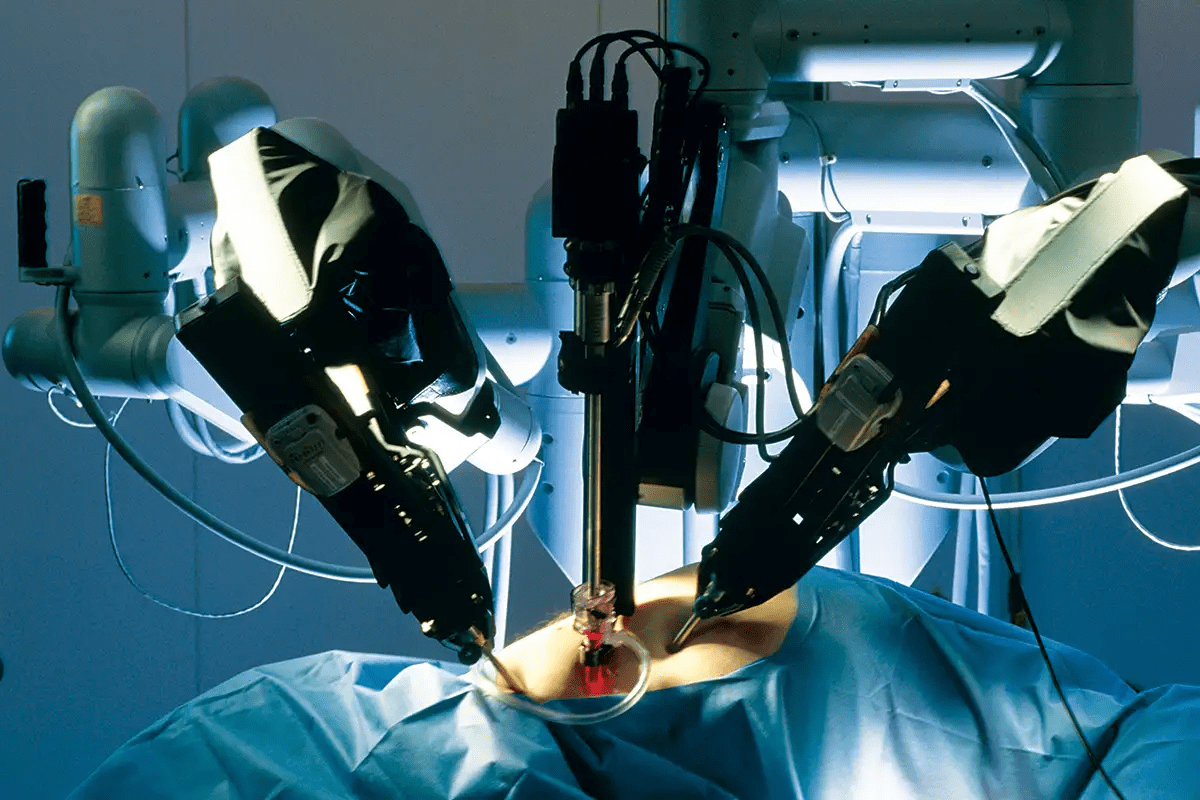
Percutaneous Coronary Intervention (PCI) with Stents
PCI with stents is a less invasive method. It uses a catheter to place a stent in the blocked artery. Drug-eluting stents are very effective in preventing the artery from getting blocked again. PCI is known for quicker recovery times, but there’s a higher chance of needing more surgeries.
Medical Management Approaches
For some, medical management is the first choice. It involves using medicines to manage symptoms and slow the disease. This can include antiplatelet therapy, beta-blockers, and statins. Medical management is key but is often used alongside surgeries like CABG or PCI for full care.
Studies show CABG and PCI with stents have similar death rates. But CABG is linked to fewer repeat surgeries. Knowing these options is key to making the best choice for LAD blockage care.
Coronary Artery Bypass Grafting Explained
Coronary artery bypass grafting (CABG) is a key surgery for heart disease. It’s mainly used for blockages in the left anterior descending artery (LAD). This surgery makes a new path for blood to reach the heart muscle.
The CABG Procedure
The CABG surgery is done under general anesthesia. It starts with opening the breastbone to reach the heart. A heart-lung machine keeps blood flowing while the heart stops.
The surgeon then takes a graft from the leg or chest. This graft goes around the blocked artery. It helps blood flow to the heart muscle.
Types of Bypass Grafts
There are different grafts used in CABG, each with its own benefits. The most common ones are:
- Saphenous Vein Grafts: These are taken from the leg and used for many bypasses.
- Left Internal Mammary Artery (LIMA): This graft is best for LAD blockages because it works well over time.
- Radial Artery Grafts: These are from the forearm and used as an option to saphenous vein grafts.
The choice of graft depends on the patient’s health and the disease’s extent. The surgeon also plays a role in this decision.
The Role of Left Internal Mammary Artery (LIMA)
The Left Internal Mammary Artery (LIMA) is very important in CABG, mainly for LAD blockages. Studies show it leads to fewer repeat surgeries and heart problems. It’s the best choice for LAD bypass because it lasts longer.
“The use of the left internal mammary artery for grafting the LAD has been shown to improve long-term survival and reduce the need for repeat revascularization procedures.”
We often use LIMA with other grafts for better results. LIMA grafting improves long-term outcomes and lowers the risk of serious heart events.
| Graft Type | Long-term Patency Rate | Preferred Use |
|---|---|---|
| LIMA | High | LAD blockages |
| Saphenous Vein | Moderate | Multiple bypasses |
| Radial Artery | Moderate | Alternative to saphenous vein |
Stent Placement Procedures for LAD Blockage
Stent placement is key in treating LAD blockages. It’s a less invasive method than bypass surgery. We’ll look at the latest in coronary stents and the stent placement process.
The Evolution of Coronary Stents
Coronary stents have changed a lot over time. At first, bare-metal stents were used but they had problems like a high risk of restenosis. Then, drug-eluting stents came along. They release medicine that stops cells from growing back, lowering restenosis rates.
Bare-Metal vs. Drug-Eluting Stents
Choosing between bare-metal and drug-eluting stents depends on several things. These include the patient’s risk of restenosis, bleeding risks, and how well they can follow antiplatelet therapy. Drug-eluting stents are better at preventing repeat procedures than bare-metal stents. But, they might not be as effective as bypass surgery in some cases.
| Stent Type | Restenosis Rate | Bleeding Risk |
|---|---|---|
| Bare-Metal Stents | Higher | Lower |
| Drug-Eluting Stents | Lower | Higher |
The Stent Placement Procedure
The stent placement process starts with local anesthesia. Then, a leg or arm artery is accessed. A catheter is guided to the coronary artery under X-ray.
After finding the blockage, a balloon angioplasty opens the artery. Then, the stent is placed. Advancements in stent technology and technique have made stent placement a good option for many. But, the choice between stent placement and bypass surgery depends on the patient’s needs and should be discussed with a healthcare provider.
Comparing Recovery and Hospital Stay
Knowing the differences in recovery and hospital stay between bypass surgery and stent placement helps patients choose the best treatment. This knowledge is key to making informed decisions.
Typical Recovery Timeline for Bypass Surgery
Bypass surgery, or Coronary Artery Bypass Grafting (CABG), is a big surgery needing a long recovery. Patients usually stay in the hospital for 5 to 7 days after surgery. The whole recovery can take 6 to 12 weeks, during which they should avoid heavy lifting and bending.
The first part of recovery is managing pain and swelling at the incision site. Patients also need to follow a rehab program. This includes physical therapy to get back strength and mobility.
Recovery After Stent Placement
Stent placement, or Percutaneous Coronary Intervention (PCI), is a less invasive procedure. Patients usually stay in the hospital for 1 to 3 days after the procedure. The recovery is much quicker, with most back to normal in 1 to 2 weeks.
After stent placement, patients are watched for a few hours to check for any immediate problems. They are then told about lifestyle changes and medication to prevent clotting around the stent.
Rehabilitation Requirements for Each Procedure
Rehabilitation is important for both procedures. For bypass surgery, a detailed rehab program is needed to regain strength and prevent complications.
For stent placement, the rehab is less intense. But, patients must make big lifestyle changes. This includes eating right, exercising regularly, and quitting smoking if they smoke.
Here is a comparative table summarizing the key differences in recovery and hospital stay between bypass surgery and stent placement:
| Procedure | Hospital Stay | Recovery Timeline | Rehabilitation Intensity |
|---|---|---|---|
| Bypass Surgery | 5-7 days | 6-12 weeks | High |
| Stent Placement | 1-3 days | 1-2 weeks | Low to Moderate |
Understanding these differences helps patients prepare for recovery. It also helps them make better choices about their treatment.
Short-term Outcomes: Bypass vs. Stents
When looking at treatments for LAD blockage, knowing the short-term results of bypass surgery and stent placement is key. We dive into the immediate effects of these treatments to shed light on their success and safety.
Procedural Success Rates
Success rates in procedures are a major sign of how well bypass surgery and stent placement work. Research shows both methods are very effective when done by experts. For example, a study in the Journal of the American College of Cardiology found CABG’s success rate to be over 95%. Stent placement had a success rate of about 98% for certain patients.
Success depends on many things like the patient’s health, the blockage’s complexity, and the medical team’s skill. Every patient is different, so what works for one might not for another.
Immediate Complications
Both bypass surgery and stent placement can have immediate complications. CABG might lead to bleeding, infection, or reactions to anesthesia. Stent placement could cause bleeding, allergic reactions, or injury to the coronary artery.
While these complications are possible, they are rare with skilled professionals in the right settings. Knowing these risks helps patients prepare and make informed choices.
In-hospital Mortality Rates
In-hospital death rates are a key measure of short-term safety. Studies show both CABG and stent placement have low in-hospital death rates, mainly in high-volume centers.
The Society of Thoracic Surgeons Adult Cardiac Surgery Database reported a 1.4% in-hospital death rate for CABG. Stent placement also has low in-hospital death rates, often under 1% in studies.
These rates can change based on patient risk factors, comorbidities, and procedure urgency. Healthcare providers use this information to weigh risks and benefits for each patient.
Long-term Effectiveness and Durability
When looking at LAD blockage treatments, we must compare bypass surgery and stent placement. The long-term success of these treatments is key to choosing the best option for patients.
Restenosis and Repeat Procedures
Restenosis, or artery narrowing after treatment, is a major factor. Coronary artery bypass grafting (CABG) shows lower restenosis rates than percutaneous coronary intervention (PCI) with stents. This is true, even more so when the left internal mammary artery (LIMA) is used as a graft. CABG leads to fewer repeat procedures, making it a more lasting solution for LAD blockage.
On the other hand, PCI with stents is less invasive but has a higher restenosis rate. Drug-eluting stents have lowered this rate, but it’s a concern, mainly for patients with diabetes or complex coronary anatomy.
Major Adverse Cardiac Events
Major adverse cardiac events (MACE), like heart attacks, strokes, and cardiac deaths, are key in evaluating treatments. CABG is linked to lower MACE rates than PCI, which is true for patients with multi-vessel disease or complex anatomy. The use of LIMA grafts in CABG is also beneficial in reducing MACE.
Studies show CABG is a more lasting revascularization strategy, with fewer MACE over time. This is important for patients at high risk of cardiac events or with significant health issues.
Long-term Survival Rates
Long-term survival is a critical measure of treatment success. Both CABG and PCI can improve survival, but CABG offers a survival benefit in certain groups, like those with complex or multi-vessel disease. The durability of CABG, with LIMA grafts, helps improve long-term survival.
In summary, CABG is a highly effective and durable treatment for LAD blockage, best for patients with complex disease or high-risk profiles.
Patient Selection Factors
Choosing between bypass surgery and stent placement depends on several factors. These include the patient’s health, the severity of their condition, and other important considerations.
Anatomical Considerations
The shape and size of the coronary arteries are key. Complex or diffuse LAD disease often needs CABG. Simpler blockages might be treated with stents.
Patients with multi-vessel disease or big lesions in important areas might do better with bypass surgery. This is because it can handle many blockages at once.
Comorbidities and Risk Assessment
Conditions like diabetes, high blood pressure, and kidney disease affect treatment choices. A detailed risk assessment is vital to see if a patient is right for either procedure.
“The presence of comorbidities can complicate both the procedure and the recovery process, making a detailed risk assessment essential.”
Tools like the EuroSCORE or SYNTA score help predict surgical risks. They guide doctors in making the best choice for patients.
| Comorbidity | Impact on Treatment Choice |
|---|---|
| Diabetes | Increases risk with stents; CABG may offer better long-term outcomes |
| Chronic Kidney Disease | May complicate surgery; careful risk assessment needed |
| Hypertension | Requires careful management during and after procedure |
Age and Life Expectancy
A patient’s age and life expectancy are also important. Younger patients might get better long-term results from CABG. Older patients or those with short life expectancies might prefer the less invasive PCI with stents.
- Younger patients: CABG might be more beneficial for long-term outcomes.
- Older patients: PCI with stents may be preferred due to less invasiveness.
Complex and Extensive LAD Disease Management
Dealing with complex LAD disease is tough. It needs a detailed plan. We look at how far the disease has spread, the patient’s health, and the best treatments.
Multi-vessel Disease Approaches
For LAD disease that affects more than one area, a detailed plan is key. Coronary artery bypass grafting (CABG) is often the top choice. It’s strong and works well for tough cases.
- CABG is better for patients with diabetes or complex heart issues.
- Using the left internal mammary artery (LIMA) to LAD has great long-term success rates.
Some might choose a mix of CABG and PCI. This combines surgery with a less invasive method.
Diffuse LAD Disease Treatment
Diffuse LAD disease is a big challenge. Treatment options include:
- Long stents or multiple stents in PCI, but it might lead to more blockages.
- CABG with LIMA grafting is often the best choice for long-term results.
Choosing the right treatment is important. We consider the patient’s health, the disease’s details, and future needs.
Left Main Coronary Artery Involvement
When LAD disease also affects the left main artery, it gets even harder. Decisions are based on:
- The severity of the left main disease and its effect on the heart.
- The patient’s other health issues and how they might affect treatment choices.
Usually, CABG is best for serious left main disease. But, PCI might be an option for some with less severe cases.
In summary, managing complex LAD disease needs a personalized approach. We consider the patient’s health, the disease’s extent, and the best treatments.
Multidisciplinary Decision-Making Process
Treating LAD blockage well needs a team of experts. This team works together to understand the patient’s situation fully. This way, they make better choices for treatment.
Heart Team Approach
A team of doctors, including cardiologists and surgeons, come together. They talk about the best treatment for each patient. They look at how bad the blockage is, the patient’s health, and past treatments.
Key members of the heart team include:
- Interventional cardiologists
- Cardiac surgeons
- Imaging specialists
- Other relevant healthcare professionals
Risk Stratification Tools
Tools for risk assessment are very important. They help the team understand the risks of each treatment. This way, they can choose the safest option for the patient.
| Risk Stratification Tool | Description | Use in LAD Blockage |
|---|---|---|
| SYNTAX Score | Assesses complexity of coronary artery disease | Helps determine the most appropriate revascularization strategy |
| EuroSCORE | Predicts risk of mortality after cardiac surgery | Used to assess surgical risk in patients with LAD blockage |
Patient Preference Considerations
What the patient wants is also important. The team makes sure the treatment fits the patient’s needs and wishes.
By using the heart team, risk tools, and considering what the patient wants, we can treat LAD blockage in a detailed and personal way.
Quality of Life After LAD Blockage Treatment
It’s important to know how LAD blockage treatment affects life quality. This is true for both patients and their healthcare providers. The treatment’s effects on daily life can be big, and many factors play a role in well-being.
Physical Limitations and Capabilities
After treatment, patients might see changes in what they can do physically. Some might get back to doing things they did before, while others face new limits. Regular exercise and rehabilitation programs can help improve physical function and quality of life.
For example, Mr. Bambang Budianto was able to do his daily activities and even light exercise after a rehabilitation program. His story shows how important tailored rehabilitation is for improving physical abilities.
| Activity | Pre-Treatment | Post-Treatment |
|---|---|---|
| Walking | Limited due to chest pain | Able to walk short distances without discomfort |
| Exercise | Avoided due to symptoms | Participates in light aerobic exercises |
| Daily Tasks | Difficulty performing tasks | Able to perform tasks with ease |
Medication Requirements
Medicine is key in managing LAD blockage and preventing heart problems. Patients usually need to take antiplatelet therapy, beta-blockers, and statins. It’s important to know why they take these medicines and any possible side effects.
Working closely with healthcare providers to adjust medications is also key. This helps manage side effects and improves quality of life.
Long-term Lifestyle Adjustments
Changing lifestyle is a big part of managing LAD blockage long-term. Patients are often told to change their diet, exercise, and smoking habits. Adopting a heart-healthy lifestyle can greatly improve quality of life and lower heart risk.
For instance, eating a Mediterranean-style diet can help manage cholesterol and improve heart health.
Understanding the effects of LAD blockage treatment on life quality is key. Patients and healthcare providers can work together. They can focus on improving physical abilities, managing medications, and making long-term lifestyle changes.
Conclusion: Making an Informed Decision
When you face a Left Anterior Descending (LAD) artery blockage, knowing your options is key. At Liv Hospital, we offer top-notch healthcare and support for international patients. We’ve talked about the main differences between bypass surgery and stent placement for LAD blockage.
Deciding between bypass surgery and stents depends on several things. These include how bad the blockage is, your overall health, and what you prefer. We believe in a personalized approach. This means we consider your unique needs and situation to help you choose the best treatment for LAD blockage.
Understanding the good and bad sides of bypass surgery and stent placement helps you make a smart choice. Our team is here to support you every step of the way. We want to make sure you get the care that’s right for you.
FAQ
What is the main difference between bypass surgery and stent placement for LAD blockage?
Bypass surgery creates a new path around the blocked LAD. Stent placement keeps the artery open with a small mesh tube.
Which is better for LAD blockage treatment: CABG or PCI with stents?
Choosing between CABG and PCI with stents depends on the patient’s health and the blockage’s severity.
What are the benefits of using the Left Internal Mammary Artery (LIMA) in CABG?
Using LIMA in CABG improves long-term results. It’s durable and less prone to blockage.
How do bare-metal stents differ from drug-eluting stents?
Bare-metal stents are metal mesh. Drug-eluting stents release medicine to prevent blockage.
What is the typical recovery timeline for bypass surgery compared to stent placement?
Bypass surgery takes longer to recover from, often weeks. Stent placement recovery is quicker, usually days.
How do comorbidities and risk assessment impact patient selection for either bypass surgery or stent placement?
Health conditions and risk factors like age are key in choosing treatment. They help decide the best option.
What is the heart team approach, and how does it influence treatment decisions?
The heart team approach involves a team of experts. They work together to find the best treatment for each patient.
How do different treatments for LAD blockage impact quality of life?
Treatment choices affect daily life. They influence physical abilities, medication needs, and lifestyle changes.
What is the significance of restenosis rates in comparing bypass surgery and stent placement?
Lower restenosis rates mean better long-term results. It’s a key factor in comparing treatments.
How does CABG compare to PCI with stents in terms of long-term survival rates?
Survival rates vary based on patient factors. Some studies show similar outcomes for certain patients.
What is the role of patient preference in the decision-making process for LAD blockage treatment?
Patient preference is important. Patients should be informed and involved in choosing their treatment.
What is the difference between CABG and angioplasty?
CABG is a surgical bypass. Angioplasty is a minimally invasive procedure with a balloon and stent.
Which is worse: bypass surgery or stent placement?
Neither is inherently worse. The choice depends on the patient’s situation, with both treatments having risks and benefits.
What are the risks associated with stent placement?
Stent placement risks include bleeding, clotting, and restenosis.
How does multi-vessel disease impact treatment decisions for LAD blockage?
Multi-vessel disease requires a complex treatment plan. It involves careful consideration of each patient’s needs.
FAQ
What is the main difference between bypass surgery and stent placement for LAD blockage?
Bypass surgery creates a new path around the blocked LAD. Stent placement keeps the artery open with a small mesh tube.
Which is better for LAD blockage treatment: CABG or PCI with stents?
Choosing between CABG and PCI with stents depends on the patient’s health and the blockage’s severity.
What are the benefits of using the Left Internal Mammary Artery (LIMA) in CABG?
Using LIMA in CABG improves long-term results. It’s durable and less prone to blockage.
How do bare-metal stents differ from drug-eluting stents?
Bare-metal stents are metal mesh. Drug-eluting stents release medicine to prevent blockage.
What is the typical recovery timeline for bypass surgery compared to stent placement?
Bypass surgery takes longer to recover from, often weeks. Stent placement recovery is quicker, usually days.
How do comorbidities and risk assessment impact patient selection for either bypass surgery or stent placement?
Health conditions and risk factors like age are key in choosing treatment. They help decide the best option.
What is the heart team approach, and how does it influence treatment decisions?
The heart team approach involves a team of experts. They work together to find the best treatment for each patient.
How do different treatments for LAD blockage impact quality of life?
Treatment choices affect daily life. They influence physical abilities, medication needs, and lifestyle changes.
What is the significance of restenosis rates in comparing bypass surgery and stent placement?
Lower restenosis rates mean better long-term results. It’s a key factor in comparing treatments.
How does CABG compare to PCI with stents in terms of long-term survival rates?
Survival rates vary based on patient factors. Some studies show similar outcomes for certain patients.
What is the role of patient preference in the decision-making process for LAD blockage treatment?
Patient preference is important. Patients should be informed and involved in choosing their treatment.
What is the difference between CABG and angioplasty?
CABG is a surgical bypass. Angioplasty is a minimally invasive procedure with a balloon and stent.
Which is worse: bypass surgery or stent placement?
Neither is inherently worse. The choice depends on the patient’s situation, with both treatments having risks and benefits.
What are the risks associated with stent placement?
Stent placement risks include bleeding, clotting, and restenosis.
How does multi-vessel disease impact treatment decisions for LAD blockage?
Multi-vessel disease requires a complex treatment plan. It involves careful consideration of each patient’s needs.
References
- American Heart Association Journals. Isolated left anterior descending coronary artery disease: percutaneous transluminal coronary angioplasty versus stenting versus left internal mammary artery bypass grafting. doi:10.1161/01.CIR.0000136580.34604.B8. Retrieved from https://www.ahajournals.org/doi/circ.0000136580.34604.b8 (Ahajournals)
- Annals of Cardiothoracic Surgery. Percutaneous coronary intervention versus coronary artery bypass grafting in the management of TCAV. doi:10.21037/acs.2018.01.10. Retrieved from https://www.annalscts.com/article/view/1651316798 (annalscts.com)
- American Heart Association Journals. Ascending Aortic Replacement With Aortic Valve Reimplantation. Circulation: Suppl. 2. Retrieved from https://www.ahajournals.org/doi/circ.100.suppl_2.II‑114 (Ahajournals)
- PubMed. Article ID 8127094. Retrieved from https://pubmed.ncbi.nlm.nih.gov/8127094
- American Heart Association. Heart Procedures and Surgeries. Retrieved from https://www.heart.org/en/health‑topics/treatments-and-procedures/angioplasty-and‑stents‑vs‑bypass‑surgery (heart.org)