The link between white blood cell count and cancer is complex. At Liv Hospital, we focus on this connection to give our patients the best care.
Changes in WBC count show how the body reacts to cancer and its treatment. We watch these changes to understand the disease’s progress and treatment success. Understanding the link between white blood cells and cancer helps doctors track how the immune system responds during therapy.
Our team is committed to personalized care. We use the latest research on white blood cell count and cancer. This approach helps us improve patient outcomes and support them during treatment.
Key Takeaways
- Changes in WBC count can be related to cancer and its treatment.
- Monitoring WBC count changes can provide valuable insights into cancer progression.
- Liv Hospital delivers expert, patient-focused care incorporating the latest research.
- Understanding the relationship between WBC count and cancer can improve treatment outcomes.
- Personalized care is essential for supporting patients throughout their treatment journey.
The Critical Role of White Blood Cells in Immune Defense
White blood cells are at the front line of our immune system. They fight off pathogens and protect us from infections and diseases. This makes them very important for our health.
Types of White Blood Cells and Their Functions
White blood cells, or leukocytes, are not all the same. They have different jobs to keep us safe. The main types are neutrophils, eosinophils, lymphocytes, monocytes, and basophils.
Neutrophils are the most common and help fight bacteria. Eosinophils deal with parasites and allergies. Lymphocytes, like B cells and T cells, are key in specific immune responses.
Monocytes turn into macrophages, which clean up debris and pathogens. Basophils help with inflammation and allergies.
Normal White Blood Cell Count Ranges
A healthy adult usually has 4,000 to 11,000 WBCs per microliter of blood. This number can vary slightly by lab. Knowing these ranges helps doctors diagnose and monitor health issues.
An abnormal WBC count can mean different things. Too many WBCs, or leukocytosis, might show infection, inflammation, or cancer. Too few, or leukopenia, can make us more prone to infections and might point to bone marrow problems or medication side effects.
White Blood Cells and Cancer: The Complex Relationship
It’s key to understand how white blood cells and cancer interact. This knowledge helps in creating better ways to diagnose and treat cancer. Cancer changes the immune system a lot, affecting white blood cell counts and how they work.
How Cancer Affects the Immune System
Cancer can change the immune system in many ways. It can lower or raise white blood cell counts. Here are some main effects:
- Immune Suppression: Some cancers weaken the immune system, causing fewer white blood cells.
- Inflammation: Cancer can cause long-lasting inflammation, leading to more white blood cells.
- Immune Evasion: Cancer cells can hide from the immune system, affecting white blood cell function.
The Significance of WBC Count in Cancer Diagnosis
White blood cell count is very important in finding cancer. Changes in WBC counts can show if cancer is present or how the body is fighting it. For example:
- Elevated WBC Counts: High counts might mean leukemia or lymphoma.
- Low WBC Counts: Low counts can mean the bone marrow is being affected by cancer.
Watching WBC counts over time helps doctors see how cancer is growing and if treatments are working.
Fact 1: Elevated WBC Counts Can Indicate Certain Types of Cancer
Elevated white blood cell (WBC) counts can signal certain cancers. This shows how the immune system and cancer are connected. We’ll look at how inflammation, which raises WBC counts, is tied to cancer. We’ll also see which cancers are linked to high WBC counts.
The Link Between Inflammation and Cancer
Chronic inflammation is a major risk for cancer. Inflammation can increase WBC counts as the body fights off threats. In cancer, this inflammation can both cause and result from tumor growth. For example, some cancers make substances that boost white blood cell production.
The connection between inflammation and cancer is complex. It involves many cell types and signals. Knowing this helps us understand why some cancers raise WBC counts.
Cancer Types Associated with High White Blood Cell Counts
Several cancers are linked to high WBC counts. These include:
- Leukemia: A blood or bone marrow cancer with abnormal white blood cells.
- Lymphoma: A cancer of the lymphatic system, causing more WBCs due to lymphocyte growth.
- Certain solid tumors: Tumors that cause long-term inflammation or make substances that increase WBCs.
Knowing which cancers raise WBC counts helps in early detection and tracking disease.
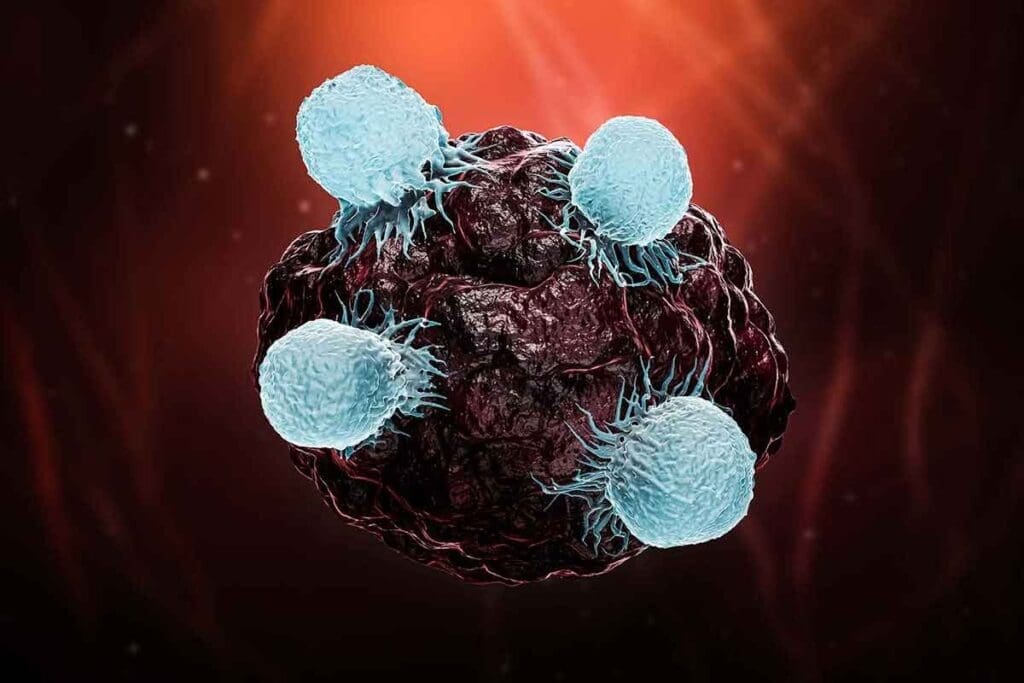
Fact 2: High Neutrophil Counts and Cancer Progression
Neutrophils are a key part of the immune system and play a big role in cancer. They help tumors grow and spread. This is because they are involved in many processes that affect tumor growth.
How Neutrophils Contribute to Metastasis
Neutrophils help cancer grow in several ways. They release factors that help tumors grow and spread. For example, they release matrix metalloproteinases (MMPs) that break down the tissue around cells, making it easier for cancer to spread.
They also interact with cancer cells, making them more aggressive. This interaction can lead to the formation of NETs. NETs are involved in cancer growth and spread.
Neutrophil-to-Lymphocyte Ratio as a Prognostic Marker
The neutrophil-to-lymphocyte ratio (NLR) is important in cancer. It’s the number of neutrophils divided by the number of lymphocytes in the blood. A high NLR means more neutrophils than lymphocytes, which is linked to a worse prognosis in many cancers.
NLR shows the balance between inflammation that helps tumors grow and the immune system fighting cancer. A high NLR means the inflammation is winning, which helps cancer grow.
| Cancer Type | NLR Cut-off Value | Prognostic Significance |
| Colorectal Cancer | 5 | High NLR associated with poor overall survival |
| Lung Cancer | 3.5 | Elevated NLR correlates with advanced disease and poor prognosis |
| Breast Cancer | 2.5 | High NLR linked to increased risk of recurrence and metastasis |
Knowing how neutrophils affect cancer and the importance of NLR helps doctors treat cancer better. This can lead to better outcomes for patients.
Fact 3: How Tumor Cells Hijack White Blood Cells
Tumor cells are smart at fooling the immune system, including white blood cells. They use these cells to grow and spread. This trickery involves many types of white blood cells and affects cancer growth.
Mechanisms of WBC Manipulation by Cancer Cells
Cancer cells trick white blood cells in different ways. They send out signals that draw certain WBCs to the tumor. For example, they release chemokines that attract myeloid-derived suppressor cells (MDSCs) and tumor-associated macrophages. These cells help keep the immune system from fighting the tumor.
Another trick is changing WBCs to help the tumor grow. Tumor-associated macrophages can turn into an M2 type. This type helps with tissue remodeling, making new blood vessels, and keeping the immune system down. All these help the tumor grow.
The Role of Tumor-Associated Macrophages
Tumor-associated macrophages (TAMs) are key in how tumors fool the immune system. They help cancer grow in many ways, including:
- Helping make new blood vessels for the tumor.
- Keeping the immune system from fighting the tumor.
- Helping tumor cells move and spread by changing the tissue around them.
It’s important to understand how tumors trick white blood cells, like TAMs. This knowledge helps in making new treatments. Researchers aim to create better ways to fight cancer by targeting these tricks.
Fact 4: Blood Cancers and Their Impact on WBC Production
It’s important to know how blood cancers affect WBC production. Blood cancers like leukemia, lymphoma, and multiple myeloma can mess with normal WBC counts. This can make it hard for the body to fight off infections and stay healthy.
Leukemia: When White Blood Cells Become the Problem
Leukemia is a blood cancer that makes too many bad white blood cells in the bone marrow. This can cause a high WBC count, taking away from normal blood cells. We look at how different types of leukemia affect WBC counts.
Lymphoma and Multiple Myeloma Effects on WBC Counts
Lymphoma and multiple myeloma also impact WBC production. Lymphoma messes with the lymphatic system, while multiple myeloma affects plasma cells in the bone marrow. Both can cause abnormal WBC counts, either by making bad cells or by stopping normal cell production.
To show how these blood cancers affect WBC counts, let’s look at a table:
| Blood Cancer Type | Effect on WBC Count | Common Symptoms |
| Leukemia | High WBC count due to proliferation of malignant cells | Fatigue, frequent infections, easy bruising |
| Lymphoma | Variable; can be normal, high, or low depending on the stage and type | Swollen lymph nodes, fever, weight loss |
| Multiple Myeloma | Often low WBC count due to bone marrow suppression | Bone pain, anemia, recurrent infections |
These blood cancers show how complex the link between WBC production and cancer is. Knowing this is key for good diagnosis and treatment.
Fact 5: Chemotherapy and Low White Blood Cell Counts
Chemotherapy fights cancer but can harm white blood cell production. White blood cells help our body fight infections. When we get chemotherapy, it can hurt our bone marrow’s ability to make these cells.
It’s key to know how chemotherapy affects white blood cell counts. We’ll see why it causes neutropenia and how to lower the risk of infections.
Why Cancer Treatments Cause Neutropenia
Neutropenia is a common side effect of chemotherapy. It happens because chemotherapy stops bone marrow from working well. This affects the production of neutrophils, which fight infections.
The severity and how long neutropenia lasts can vary. Some people might only have mild cases, while others need more help.
Managing Infection Risk During Treatment
Keeping infection risk low during chemotherapy is very important. Here are some ways to do it:
- Monitoring white blood cell counts regularly
- Administering growth factors to stimulate white blood cell production
- Implementing preventive measures such as avoiding large crowds and maintaining good hygiene
- Using prophylactic antibiotics in some cases
Healthcare providers can make plans to manage these risks by understanding them.
Let’s look at how different chemotherapy regimens affect white blood cell counts:
| Chemotherapy Regimen | Risk of Neutropenia | Management Strategies |
| Regimen A | High | Growth factors, close monitoring |
| Regimen B | Moderate | Preventive antibiotics, hygiene practices |
| Regimen C | Low | Regular monitoring, patient education |
By making treatment plans for each patient and watching their condition closely, healthcare providers can reduce risks.
Fact 6: When Low WBC Count May Signal Undiagnosed Cancer
A low white blood cell (WBC) count, or leukopenia, can signal health issues, including undiagnosed cancer. It’s not a sure sign of cancer, but knowing the causes and signs is key for early treatment.
Distinguishing Between Cancer and Other Causes of Low WBC
Low WBC counts can come from many things, making it hard to find the cause. Some common reasons include:
- Viral infections
- Autoimmune disorders
- Bone marrow disorders
- Certain medications
- Nutritional deficiencies
Cancer, like blood cancers, can also cause low WBC counts. When cancer affects the bone marrow, it can stop normal blood cell production, leading to leukopenia.
Warning Signs That Warrant Further Investigation
If you have a low WBC count, watch for other symptoms that might mean a serious issue like cancer. Some signs to look out for are:
- Persistent fatigue or weakness
- Unexplained weight loss
- Frequent infections
- Easy bruising or bleeding
- Swollen lymph nodes or spleen
If you have several of these symptoms and a low WBC count, see your doctor. They might suggest tests like:
- Complete Blood Count (CBC) tests
- Bone marrow biopsy
- Imaging studies (e.g., CT scans)
Early detection and diagnosis are vital for effective treatment. A low WBC count alone doesn’t mean cancer, but knowing the signs and talking to your doctor can help if cancer is there.
Getting a cancer diagnosis can be scary, but knowing the signs and taking care of your health can help. If you’re worried about your WBC count or notice any warning signs, get medical advice right away.
Fact 7: How Cancer Directly Disrupts White Blood Cell Production
Cancer can mess with how our body makes white blood cells. These cells are key to fighting off infections and diseases. When cancer messes with white blood cell production, it can really hurt a patient’s health and how well they respond to treatment.
Bone Marrow Infiltration by Cancer Cells
Cancer can harm white blood cell production by getting into the bone marrow. The bone marrow is inside some bones, like the hips and thighbones. It’s where blood cells, including white blood cells, are made.
When cancer cells get into the bone marrow, they take over the space where healthy cells are made. This means fewer healthy white blood cells are made. Patients then get sick easier because their body can’t fight off infections well.
For example, leukemia is a cancer that affects the blood or bone marrow. It makes abnormal white blood cells that don’t work right.
Paraneoplastic Effects on WBC Production
Some cancers also cause paraneoplastic syndromes that mess with white blood cell production. These syndromes are rare and happen when the immune system reacts to a tumor in a weird way. They can make substances that either help or hurt the making of white blood cells.
For instance, some tumors make G-CSF. This is a substance that tells the bone marrow to make more white blood cells, like neutrophils. This can make the white blood cell count go up, leading to a condition called leukocytosis.
| Mechanism | Effect on WBC Production | Clinical Implication |
| Bone Marrow Infiltration | Decreased production of healthy WBCs | Increased risk of infections |
| Paraneoplastic Effects | Variable (increased or decreased WBC production) | Leukocytosis or leukopenia, depending on the substance produced |
In conclusion, cancer can mess with white blood cell production in a few ways. It can get into the bone marrow or cause paraneoplastic effects. Knowing how these happen is key to managing cancer’s effects on blood cells and helping patients get better.
Monitoring WBC Counts During Cancer Treatment
Keeping an eye on white blood cell (WBC) counts is key in cancer treatment. We know that fighting cancer well means watching WBC counts closely. This helps us manage the disease better.
WBC counts can change for many reasons during treatment. These include the cancer type, treatment methods, and how the patient reacts. Regular blood tests help us see these changes. Then, we can adjust treatment plans as needed.
Frequency of Blood Tests for Cancer Patients
How often cancer patients need blood tests depends on several things. These include the cancer type, treatment, and what the patient needs. Usually, we suggest blood tests:
- Before starting treatment to set a baseline WBC count
- During treatment to watch WBC counts and change plans if needed
- After treatment to make sure WBC counts go back to normal
Patients on chemotherapy might need blood tests more often. This is to catch side effects like neutropenia early.
Interpreting Changes in WBC Counts Over Time
Understanding WBC count changes is complex. We look at the patient’s history, current treatment, and health. This helps us spot issues and change treatment plans if needed.
| WBC Count Range | Interpretation | Potential Actions |
| Normal Range | Shows a healthy immune system | Keep following the current treatment plan |
| Low WBC Count | May mean a higher risk of infections | Change the treatment plan, think about using growth factors |
| High WBC Count | Could mean inflammation or cancer getting worse | Look into the cause, adjust treatment as needed |
By watching WBC counts and understanding changes, we can make cancer treatment better. It’s important for patients and doctors to talk often. This helps manage WBC count issues during treatment.
Innovative Approaches to Managing WBC Abnormalities in Cancer Care
Cancer treatment is always getting better, and managing white blood cell (WBC) issues is key. New ways to handle WBC problems in cancer patients are being found. These methods help improve treatment results and lower risks.
Growth Factors and Other Supportive Treatments
Growth factors are proteins that help make more blood cells, like white blood cells. In cancer care, they are used to stop and treat low neutrophil levels, a type of WBC problem.
Other supportive treatments include:
- Antibiotics to prevent or treat infections
- Adjustments to chemotherapy regimens to minimize WBC toxicity
- Nutritional support to enhance overall health
Emerging Therapies Targeting the WBC-Cancer Relationship
Scientists are working on new treatments that focus on the link between WBCs and cancer. These new treatments aim to:
- Change the tumor environment to slow cancer growth
- Boost the body’s immune fight against tumors
- Lessen inflammation linked to cancer growth
The table below shows some new ways to manage WBC issues in cancer care:
| Therapy | Purpose | Benefits |
| Growth Factors (e.g., G-CSF) | Stimulate WBC production | Prevents neutropenia, reduces infection risk |
| Supportive Treatments (e.g., antibiotics, nutritional support) | Manage treatment side effects | Enhances patient health, reduces complications |
| Emerging Therapies (e.g., tumor microenvironment modulation) | Target WBC-cancer relationship | Potential to improve treatment outcomes, reduce cancer progression |
Conclusion: The Importance of WBC Monitoring in Cancer Management
Monitoring white blood cell counts is key in cancer care. It helps spot problems early and shapes treatment plans. We’ve learned how cancer changes white blood cells, showing if the disease is growing or responding to treatment.
The link between white blood cell counts and treatment results is complex. It involves factors like the neutrophil-to-lymphocyte ratio and tumor-associated macrophages. By watching white blood cells closely, doctors can tweak treatments to better help patients.
Managing white blood cells in cancer needs a full approach. This includes regular blood tests and new diagnostic tools. We think knowing how white blood cell counts relate to cancer helps both patients and doctors improve care.
As we learn more about white blood cells and cancer, we can create better treatments. This will help patients live better lives while they’re fighting cancer.
FAQ
What is the normal range for white blood cell counts, and how does cancer affect it?
White blood cell (WBC) counts usually fall between 4,500 to 11,000 cells per microliter of blood. Cancer and its treatment can change these numbers. This often leads to either too many or too few WBCs.
Can a high white blood cell count be a sign of cancer?
A high WBC count might be linked to some cancers, like those causing chronic inflammation or leukemia. But, it’s not a sure sign of cancer. Other issues like infections or inflammatory diseases can also raise WBC counts.
How does chemotherapy affect white blood cell counts?
Chemotherapy can lower WBC counts by slowing down the bone marrow. This is called neutropenia. It makes infections more likely and might need growth factors to help WBCs.
What is the neutrophil-to-lymphocyte ratio, and why is it important in cancer?
The neutrophil-to-lymphocyte ratio (NLR) compares neutrophils to lymphocytes in the blood. A high NLR is linked to a worse prognosis in many cancers. It suggests a strong inflammatory response that helps tumors grow.
Can cancer directly affect the production of white blood cells?
Yes, some cancers, like leukemia or lymphoma, can directly harm WBC production. They might invade the bone marrow or make substances that affect WBCs.
How often should white blood cell counts be monitored during cancer treatment?
Monitoring WBC counts during cancer treatment depends on the cancer type, treatment, and patient’s health. Blood tests are often done regularly, sometimes weekly or before each treatment. This helps check WBC counts and adjust treatment as needed.
Are there new treatments being developed to manage WBC abnormalities in cancer patients?
Yes, new therapies and supportive treatments are being developed. These include growth factors to boost WBC production. They aim to lower infection risks and help with cancer treatment.
What are tumor-associated macrophages, and how do they relate to cancer?
Tumor-associated macrophages are WBCs that cancer cells manipulate to help tumors grow. They play a big role in creating an environment that suppresses the immune system. This helps cancer develop and spread.
How can low white blood cell counts be managed during cancer treatment?
Low WBC counts during cancer treatment can be managed in several ways. This includes using growth factors, adjusting chemotherapy, and preventing infections. Measures like prophylactic antibiotics or isolation procedures can help.
Reference
- National Institutes of Health, MedlinePlus. Low White Blood Cell Count and Cancer. https://medlineplus.gov/ency/patientinstructions/000675.htm