Last Updated on November 26, 2025 by Bilal Hasdemir
Nearly 1.9 million people are diagnosed with cancer each year in the United States. Many of them undergo chemotherapy as part of their treatment. After chemotherapy, patients need careful monitoring to check their recovery and spot any issues early.
Crucial to this monitoring are various blood tests. These tests help healthcare providers understand the patient’s overall health.
One of the main tests done is the Complete Blood Count (CBC) test. It measures different components, like red cells and platelets. It’s important to understand these test results to manage side effects and keep patients safe.
Key Takeaways
- Chemotherapy patients require regular monitoring through blood tests.
- The Complete Blood Count (CBC) test is a key diagnostic tool.
- CBC tests measure various components, including red cells and platelets.
- Understanding test results is vital for managing side effects.
- Blood tests help healthcare providers assess patient recovery.
Understanding Blood Tests in Cancer Treatment
Blood tests are key in managing cancer. They help check if treatment is working and spot side effects early. It’s important for both patients and doctors to understand their role.
The Role of Blood Tests in Monitoring Treatment Response
Blood tests track how the body reacts to cancer treatment. They look at white blood cells, red blood cells, and platelets. These cells can change with chemotherapy. Doctors use these tests to see if treatment is on track or if changes are needed.
Why Regular Blood Testing is Essential
Getting blood tests regularly is vital during and after chemo. They help doctors find problems early and fix side effects fast. This keeps treatment effective and reduces risks.
Complete Blood Count (CBC): A Crucial Diagnostic Tool

The CBC is a detailed test that checks different parts of the blood. It gives important information about a patient’s health during cancer treatment. This test is key in seeing how chemotherapy affects the body and tracking the patient’s healing.
Components of a CBC Test
A CBC test looks at several important parts of the blood. These include white blood cells, red blood cells, and platelets. White blood cells help fight infections. Red blood cells carry oxygen. Platelets help the blood to clot.
- White Blood Cell (WBC) count
- Red Blood Cell (RBC) count
- Platelet count
How often CBC tests are done depends on the patient’s health and treatment plan.
Frequency of CBC Tests
Usually, CBC tests are done often to check how well the treatment is working. They also help find any problems early.
- Before each chemotherapy cycle
- During chemotherapy treatment
- After completing chemotherapy to monitor recovery
White Blood Cells Less: A Common Chemotherapy Side Effect
Chemotherapy often lowers white blood cell counts. This makes patients more likely to get infections. It’s a common side effect that needs careful watching and management to avoid problems.
Normal White Blood Cell Range vs. Post-Chemotherapy Levels
A normal white blood cell count is between 4,500 and 11,000 cells per microliter of blood. But, after chemotherapy, this number often drops below normal. A low WBC count, or leukopenia, raises the risk of getting sick.
After chemotherapy, how much WBC counts drop can vary. The type of chemotherapy, the dose, and the person’s health all play a part.
Types of White Blood Cells Affected by Chemotherapy
Chemotherapy can lower different types of white blood cells. These include neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Neutrophils, the most common, are key in fighting off infections. A drop in neutrophils, or neutropenia, is a common side effect.
Lymphocytes, another important WBC, help the immune system. Chemotherapy can lower lymphocytes, making patients more prone to infections.
What a WBC Count of 3.1 or Lower Means
A WBC count of 3.1 or lower is considered low. It means a higher risk of getting sick. In these cases, patients might need close monitoring and treatments like growth factor therapy to boost white blood cell production.
It’s important to understand what a low WBC count means. Regular blood tests are key to keep an eye on WBC counts and adjust treatment plans as needed.
Neutrophil Count: The Critical Marker After Chemotherapy
Healthcare providers closely watch the neutrophil count after chemotherapy. This count shows how well a patient can fight off infections. Neutrophils, a key type of white blood cell, often decrease after chemotherapy.
Understanding Absolute Neutrophil Count (ANC)
The Absolute Neutrophil Count (ANC) measures the number of neutrophils in the blood. It’s found by multiplying the total white blood cell count by the percentage of neutrophils. ANC is a vital indicator of a patient’s risk of infection. An ANC below 500 cells per microliter raises the risk of severe infections.
When Low Neutrophils Become Dangerous
A low neutrophil count, or neutropenia, can be dangerous if it falls below certain levels. Patients with an ANC below 1000 cells per microliter face a higher risk of infection. Prompt medical attention is necessary if symptoms of infection occur, such as fever, chills, or sore throat.
What Cancer Types Cause Low Neutrophils
Certain cancers and their treatments can lower neutrophil counts. For example, cancers like leukemia affect bone marrow and neutrophil production. Also, intensive chemotherapy can lead to lower ANC levels. Knowing the risks of different cancers and treatments helps manage neutropenia well.
- Leukemia
- Lymphoma
- Chemotherapy-intensive regimens
Red Blood Cell and Hemoglobin Testing Post-Chemotherapy
Chemotherapy can harm the body’s ability to make red blood cells, causing anemia. It’s key to understand how chemotherapy affects red blood cell production to manage side effects.
Chemotherapy can stop the bone marrow from making red blood cells. When there are fewer red blood cells, the body’s tissues and organs don’t get enough oxygen. This can lead to fatigue, weakness, and other symptoms.
Effects of Chemotherapy on Red Blood Cell Production
Chemotherapy can lower red blood cell production, causing low hemoglobin levels. Low hemoglobin can make you feel tired, weak, and experience other symptoms.
Interpreting Low Hemoglobin Levels
Hemoglobin levels are a key sign of anemia. Low hemoglobin levels mean you might need medical help.
Consequences of Low Red Blood Cell and White Blood Cell Count
Low counts of both red and white blood cells show a strong bone marrow suppression. This raises the risk of infections and other serious problems.
Platelet Count Monitoring After Cancer Treatment
Monitoring platelet counts is key in managing cancer treatment risks. Platelets help blood clot, and treatments can lower their count.
Knowing the normal platelet range is vital. It’s between 150,000 to 450,000 per microliter of blood. Counts below this can mean thrombocytopenia, raising bleeding risks.
Normal vs. Low Platelet Counts
Thrombocytopenia, or low platelet count, can happen due to cancer treatment. It makes it hard for blood to clot. This can cause easy bruising, long bleeding from cuts, and serious internal bleeding.
| Platelet Count Range | Status | Risks |
| 150,000 – 450,000 | Normal | None |
| 50,000 – 149,000 | Mild Thrombocytopenia | Increased risk of bruising and bleeding |
| Severe Thrombocytopenia | High risk of spontaneous bleeding |
Bleeding Risks Associated with Low Platelets
Low platelet counts raise bleeding risks. Severe cases can be life-threatening. If you have severe symptoms like headache, confusion, or trouble breathing, seek medical help right away.
Key Risks:
- Easy bruising and petechiae (small spots on the skin)
- Prolonged bleeding from minor cuts
- Nosebleeds or bleeding gums
- Internal bleeding, which can be life-threatening
Low Platelets as a Cancer Symptom vs. Treatment Effect
Low platelet counts can be a cancer symptom or a treatment side effect. Some cancers, like leukemia, can directly affect platelet production. Treatments like chemotherapy can also lower platelet counts by affecting bone marrow.
Knowing why platelet counts are low is key to managing it. Healthcare providers must monitor counts closely. This helps adjust treatment plans to manage risks effectively.
Comprehensive Metabolic Panel: Beyond Blood Cells
The CMP is a blood test that checks many substances in the blood. It looks at electrolytes like sodium, potassium, and chloride. It also checks liver and kidney function.
Liver Function Tests
Liver function tests are key in the CMP. They measure enzymes and proteins in the blood. This helps check if the liver is healthy.
Kidney Function and Electrolyte Balance
The CMP also checks kidney function with creatinine and urea levels. It looks at electrolyte levels too. These are important for fluid balance and nerve function.
Chemotherapy’s Impact on Blood Chemistry
Chemotherapy can change blood chemistry a lot. It affects electrolyte levels and kidney function. The CMP helps doctors keep an eye on these changes.
By looking at CMP results, doctors can make better treatment plans. This helps reduce side effects and improves patient outcomes during chemotherapy.
Interpreting Your Blood Test Results
It’s key for chemotherapy patients to understand their blood tests well. This helps them manage their treatment better. Lab ranges help doctors see how you’re doing and change treatment plans if needed.
Understanding Laboratory Reference Ranges
Laboratory reference ranges are the standards for blood test results. They show what’s normal for things like white blood cells, red blood cells, and platelets. Knowing these ranges helps spot problems and guide patient care.
Table: Normal Blood Count Ranges
| Blood Component | Normal Range |
| White Blood Cells (WBC) | 4,500 – 11,000 cells/μL |
| Red Blood Cells (RBC) | 4.32 – 5.72 million cells/μL (men), 3.90 – 5.03 million cells/μL (women) |
| Platelets | 150,000 – 450,000 cells/μL |
What “Slightly Low” WBC Means
A “slightly low” WBC count, between 3,000 and 4,000 cells/μL, might not be a big deal. But, doctors keep a close eye on it. They look at your health, treatment, and past to decide what to do next.
Patterns That Concern Oncologists vs. Normal Fluctuations
Oncologists watch blood tests for patterns that might mean trouble, like a low WBC count that doesn’t go away. It’s important to tell the difference between worrying signs and normal changes. This helps adjust treatment and keep patients safe.
By knowing lab ranges and understanding blood test results, patients and doctors can better handle chemotherapy side effects. This leads to better treatment outcomes.
The Minimum WBC Count Required for Chemotherapy
Knowing the minimum white blood cell (WBC) count needed for chemotherapy is key for cancer patients. Chemotherapy can harm the bone marrow, making it hard to produce white blood cells. These cells are essential for fighting off infections.
Treatment Delays Due to Low Blood Counts
Low WBC counts, or leukopenia, can cause treatment delays. If a patient’s WBC count is too low, they’re at higher risk of getting sick. Chemotherapy might be put off until the count goes back up. This delay can affect how well the treatment works.
Factors Influencing Treatment Delays:
- Severity of leukopenia
- Type of cancer being treated
- Intensity of the chemotherapy regimen
Decision-Making Process for Continuing or Pausing Chemotherapy
Deciding to keep going with chemotherapy or to pause it is a big decision. Doctors look at many things, like the patient’s health, the cancer type, and the chemotherapy plan. They weigh the risks against the benefits.
Key Considerations:
- Current WBC count and trend
- Presence of any infections or signs of illness
- Patient’s overall health and resilience
How Different Cancer Types Affect Minimum Count Requirements
Each cancer type and chemotherapy plan has its own WBC count needs. For example, leukemia patients might need different counts than those with solid tumors.
| Cancer Type | Typical Minimum WBC Count Requirement | Considerations |
| Leukemia | 1,000-1,500 cells/μL | Higher risk of infection; close monitoring required |
| Solid Tumors | 1,500-2,000 cells/μL | Risk of infection; treatment may be delayed |
| Lymphoma | 1,000-2,000 cells/μL | Variable risk based on chemotherapy intensity |
In conclusion, the minimum WBC count needed for chemotherapy varies. It depends on the cancer type, the chemotherapy plan, and the patient’s health. Understanding these factors is key to managing treatment well.
Recovery Patterns of Blood Cells After Chemotherapy
Patients on chemotherapy need to know that blood cell recovery takes time. Chemotherapy harms the bone marrow, reducing white blood cells, red blood cells, and platelets. Knowing how these cells recover is key to good patient care.
Typical Timeline for Blood Count Recovery
The time it takes for blood counts to recover varies. It depends on the chemotherapy type, health, and age. White blood cells usually start to recover in a few days to a week. Red blood cells and platelets might take longer.
It’s vital for patients to keep in touch with their doctors to check blood counts.
Factors Affecting Recovery Speed
Many things can affect how fast blood counts recover. These include age, nutrition, and health conditions. The chemotherapy type and dosage also play a big role. Some treatments can slow down blood cell production.
To increase WBC count during chemotherapy, patients should eat well, drink plenty of water, and rest enough. Doctors might also prescribe medicines to help.
When Blood Counts Indicate a Possible Relapse
Watching blood counts is important during and after chemotherapy. Low counts can mean a relapse might be coming. But, doctors look at all health signs and tests together.
Knowing how blood cells recover helps patients take charge of their health. By watching their counts and acting fast on any issues, patients can lower risks and get better results.
Medical Interventions for Low Blood Counts
Managing low blood counts is key in cancer treatment, after chemotherapy. Low blood counts can cause infections, anemia, and bleeding disorders. Luckily, there are medical ways to reduce these risks.
Growth Factors for White Blood Cell Stimulation
Growth factors are proteins that help make white blood cells. These cells fight infections. Granulocyte-colony stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF) are used to increase white blood cell counts. They help lower infection risks and let patients keep up with their chemotherapy.
G-CSF is given as an injection, starting a day or two after chemotherapy. It makes the bone marrow produce more neutrophils. Neutrophils are white blood cells that fight infections.
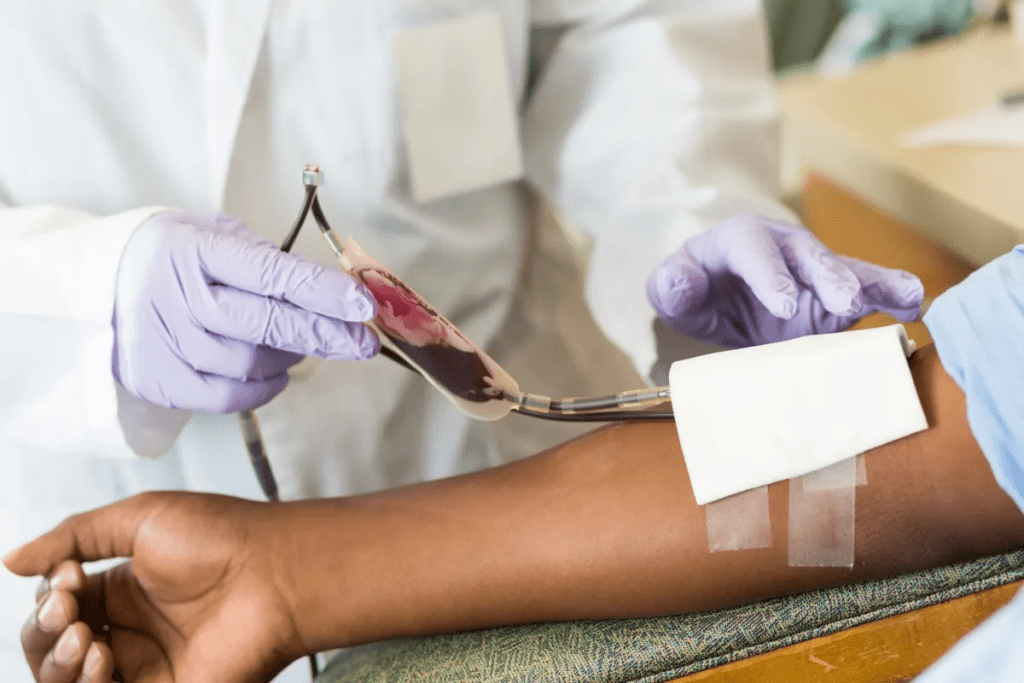
Transfusions and Other Supportive Treatments
Transfusions and other treatments also help with low blood counts. Red blood cell transfusions increase red blood cell counts. This reduces anemia and its symptoms like fatigue and shortness of breath. Platelet transfusions prevent bleeding by raising platelet counts.
Other treatments include antibiotics to fight infections and medications for symptoms of low blood counts.
Medication Adjustments to Manage Blood Count Issues
Sometimes, changing medications is needed to handle blood count problems. This might mean reducing the dosage or delaying the administration of chemotherapy. Doctors may also prescribe drugs to boost blood cell production or manage symptoms.
It’s important to watch blood counts closely. This way, problems can be caught early, and treatments can be started quickly to avoid complications.
How to Increase WBC Count During Chemotherapy
To boost your white blood cell count during chemotherapy, you need a few strategies. Chemotherapy can weaken your body’s ability to make white blood cells. It’s key to support blood cell production and overall health.
Prescribed Medical Approaches
Medical treatments are vital for managing low white blood cell counts during chemotherapy. Growth factors are often used to help the bone marrow make more white blood cells. This can lower the risk of infections and prevent delays in treatment.
Filgrastim and pegfilgrastim are common growth factors used. Your doctor will choose the best one for you based on your treatment plan.
| Medication | Purpose | Common Side Effects |
| Filgrastim | Stimulates WBC production | Bone pain, fatigue |
| Pegfilgrastim | Long-acting WBC stimulation | Bone pain, nausea |
Nutrition for Blood Cell Production
Eating a balanced diet is essential for blood cell production. Foods rich in protein, vitamin C, and zinc are great. Include fruits, vegetables, lean proteins, and whole grains in your meals.
- Protein-rich foods: chicken, fish, beans, and eggs
- Vitamin C-rich foods: citrus fruits, strawberries, bell peppers
- Zinc-rich foods: oysters, beef, chicken, fortified cereals
Physical Activity and Rest Balance
It’s important to balance physical activity and rest during chemotherapy. Stay active but also listen to your body and rest when needed. Gentle exercises like walking or yoga can help.
Finding the right balance can help manage fatigue and support recovery. Always talk to your healthcare team before starting or changing any exercise routine during chemotherapy.
Long-Term Blood Monitoring After Completing Chemotherapy
After finishing chemotherapy, the body needs to recover. Monitoring blood levels is key to catch any problems early. This helps doctors keep an eye on how well the body is doing and fix any issues quickly.
Follow-up Schedule for Blood Tests
The timing of blood tests after chemotherapy changes based on the cancer type and treatment. Tests are usually done:
- Every few weeks at first
- Every few months later
- Annually or as needed for ongoing checks
This schedule helps doctors see how blood counts are recovering. It also helps spot any late effects of chemotherapy.
What Doctors Look for in Long-Term Monitoring
Doctors check for several important signs during long-term monitoring. These include:
| Indicator | Significance |
| Blood Count Recovery | Normalization of white blood cell, red blood cell, and platelet counts |
| Late Effects of Chemotherapy | Detection of long-term side effects on the blood and other systems |
| Signs of Relapse | Early detection of cancer recurrence through changes in blood counts or other markers |
When Blood Counts Typically Return to Normal
How long it takes for blood counts to get back to normal varies. Usually, it starts within a few weeks to months after treatment ends. But, it can take up to a year or more for all counts to fully recover. This depends on the treatment’s intensity and the patient’s health.
Knowing the blood test schedule and what doctors look for helps patients. It helps them understand what to expect and work closely with their doctors. This ensures the best possible recovery.
When to Seek Immediate Medical Attention for Blood Count Issues
After getting chemotherapy, it’s key to watch your health closely. Chemotherapy can lower your blood counts. This makes you more likely to get infections and face other problems.
Warning Signs
Look out for these warning signs that mean you need to see a doctor fast: fever over 100.4 °F (38 °C), chills, extreme tiredness, unusual bleeding or bruising, and trouble breathing. If you see any of these, get medical help right away.
Emergency Situations
Some situations need quick action. If you have severe chest pain, trouble breathing, or bad stomach pain, go to the emergency room. These can be serious and need fast medical help.
Communicating with Your Healthcare Team
Tell your healthcare team about any new or getting worse symptoms. Ask them questions about your treatment and side effects. They can offer important advice and support as you get better.
Conclusion: The Vital Role of Blood Testing in Cancer Recovery
Regular blood testing is key for cancer patients. It helps healthcare teams keep an eye on their health and spot problems early. This knowledge is vital for patients to understand their treatment better.
Blood tests let doctors check a patient’s health and decide on the best care. By regularly testing and acting quickly, patients can get better results. This approach is essential for their recovery.
FAQ
What blood test is done after chemotherapy?
After chemotherapy, the main blood test is the Complete Blood Count (CBC). It checks the blood’s different parts, like white and red blood cells, and platelets.
What does a low white blood cell count mean?
A low white blood cell count means you might get sick easier. If it’s 3.1 or lower, you need to watch it closely and manage it well.
What is the normal range for WBC count?
The normal WBC count is between 4,500 and 11,000 cells per microliter. This range is usually considered healthy.
How often are CBC tests performed during treatment?
CBC tests are done often to check how you’re doing. How often depends on your health and treatment plan.
What is the minimum WBC count required for chemotherapy?
The minimum WBC count needed for chemotherapy varies. It depends on your health and treatment plan. Doctors must decide if to keep going or stop chemotherapy.
How can I increase my WBC count during chemotherapy?
To boost your WBC count, you need medical help, good nutrition, and lifestyle changes. This includes following your doctor’s advice, eating well, and balancing rest and activity.
What are the warning signs of dangerously low blood counts?
Danger signs include fever, bleeding, and other symptoms. If you have these, get medical help right away.
How long does it take for blood counts to recover after chemotherapy?
Blood count recovery time varies. It depends on your health, age, and chemotherapy type. Recovery speed can differ.
What is the role of growth factors in managing low blood counts?
Growth factors help make more white blood cells. They are often given to patients on chemotherapy to manage low counts.
How do different cancer types affect minimum count requirements?
Different cancers and treatments affect minimum counts. Doctors must consider these when deciding on treatment.
What is the significance of platelet count monitoring after cancer treatment?
Monitoring platelet counts is key after treatment. It helps spot bleeding risks. Low counts can lead to bleeding.
How do chemotherapy drugs affect blood chemistry?
Chemotherapy can change blood chemistry. It affects liver and kidney function and electrolyte balance. Monitoring is important to catch problems early.
What is a complete metabolic panel?
A complete metabolic panel is a detailed test. It shows your overall health, including liver and kidney function, and electrolyte balance.
How can I communicate effectively with my healthcare team about blood count issues?
Talk to your healthcare team about any symptoms or worries. Ask about your treatment and blood count results.
References
- National Health Service (NHS). (2024). Chemotherapy – Side effects and risks.https://www.nhs.uk/conditions/chemotherapy/side-effects/





