Last Updated on November 26, 2025 by Bilal Hasdemir
Ovarian cancer is a major health concern, with nearly 20,000 new cases diagnosed every year in the United States. Research shows that the immune system’s reaction to this disease can be seen in white blood cell counts. Studies indicate that ovarian cancer can change white blood cell counts, but it’s not simple.
It’s important to understand how white blood cells and ovarian cancer are connected. This knowledge helps in finding better ways to diagnose and treat the disease. This article will look into how white blood cell count and ovarian cancer are linked, shedding light on the immune system’s role in fighting this disease.
Key Takeaways
- The immune system’s response to ovarian cancer can be indicated by changes in white blood cell counts.
- Ovarian cancer can affect white blood cell counts, but the relationship is complex.
- Understanding the link between white blood cells and ovarian cancer is key for diagnosis and treatment.
- Research is ongoing to develop effective diagnostic and treatment strategies.
- The connection between ovarian cancer and immune system response is an area of growing research.
Understanding White Blood Cells and Their Normal Function
White blood cells are key to how our bodies fight off sickness, including ovarian cancer. They are a big part of our immune system. They help keep us safe from infections and diseases.
Types of White Blood Cells and Their Roles
There are many types of white blood cells, each with its own job. Neutrophils are the most common and fight bacterial infections. Lymphocytes, like B cells and T cells, help with specific immune responses. They make antibodies and fight off diseases.
Monocytes turn into macrophages, which clean up and destroy harmful cells and germs. Eosinophils and basophils help with parasite attacks and allergic reactions.
Normal White Blood Cell Count Ranges
A normal white blood cell count is between 4,500 and 11,000 cells per microliter of blood. This number can change slightly depending on the lab. If your count is outside this range, it could mean you have an infection, inflammation, or a problem with your bone marrow.
Factors That Naturally Affect WBC Levels
Many things can change your white blood cell count. Age and gender can play a role, with women often having higher counts, like during their period or when pregnant. Stress, whether it’s physical or emotional, can also affect your count. Some medicines, like corticosteroids, can lower your count by weakening your immune system.
Ovarian Cancer: An Overview
Ovarian cancer is a big health problem because of its many types and late detection. It’s a complex disease that affects thousands of women every year.
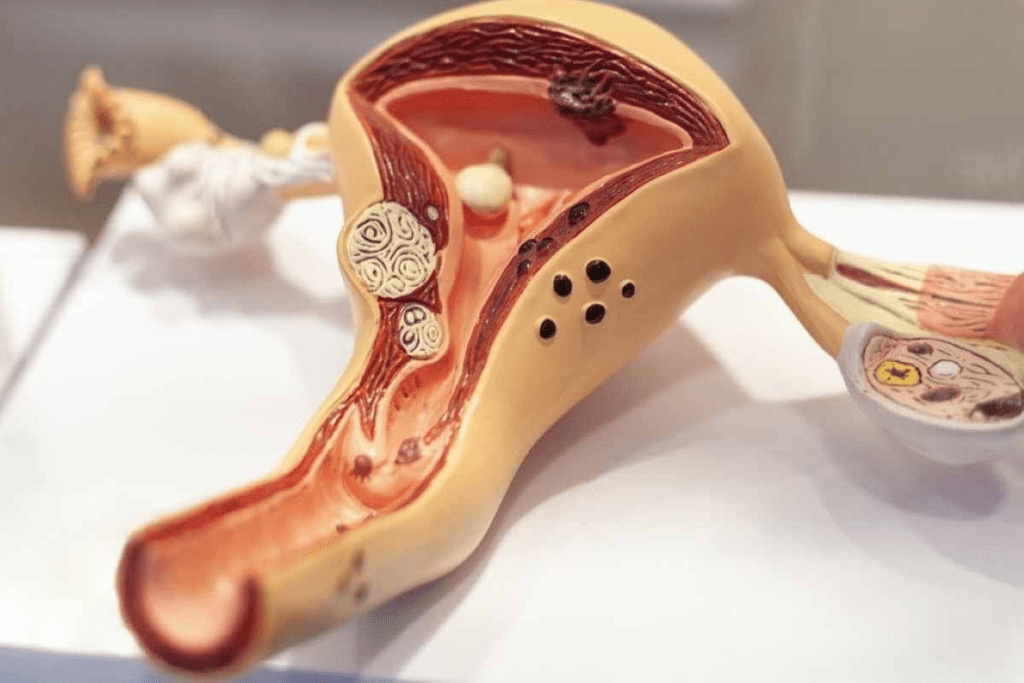
Types and Stages of Ovarian Cancer
Ovarian cancer is not just one disease but a group of cancers that start in the ovaries. The most common type is epithelial ovarian cancer, making up about 90% of cases. Other types include germ cell tumors and sex cord-stromal tumors.
The stage of ovarian cancer is key for knowing how well it can be treated. It’s staged from I (just in the ovaries) to IV (spread to other parts of the body). Early ovarian cancer often has no symptoms, making it hard to find.
| Type of Ovarian Cancer | Description | Frequency |
| Epithelial Ovarian Cancer | Arises from the outer layer of the ovary | 90% |
| Germ Cell Tumors | Originates from the cells that produce eggs | 5% |
| Sex Cord-Stromal Tumors | Develops from the connective tissue of the ovary | 5% |
Common Symptoms and Diagnostic Challenges
Ovarian cancer symptoms are often not clear and can be like other common issues. Symptoms include bloating, pelvic pain, and trouble eating.
Finding ovarian cancer early is hard because there’s no good screening test. Doctors use imaging like ultrasound and surgery to diagnose it.
Risk Factors and Prevalence
Some things can raise your risk of getting ovarian cancer. These include family history, certain genetic changes, and reproductive factors. Women with endometriosis or trouble getting pregnant are also at higher risk.
Ovarian cancer is the fifth leading cause of death from cancer in women in the U.S. The American Cancer Society says there were about 21,750 new cases in 2023. Sadly, about 13,940 women died from it.
White Blood Cells Ovarian Cancer: The Relationship Explained
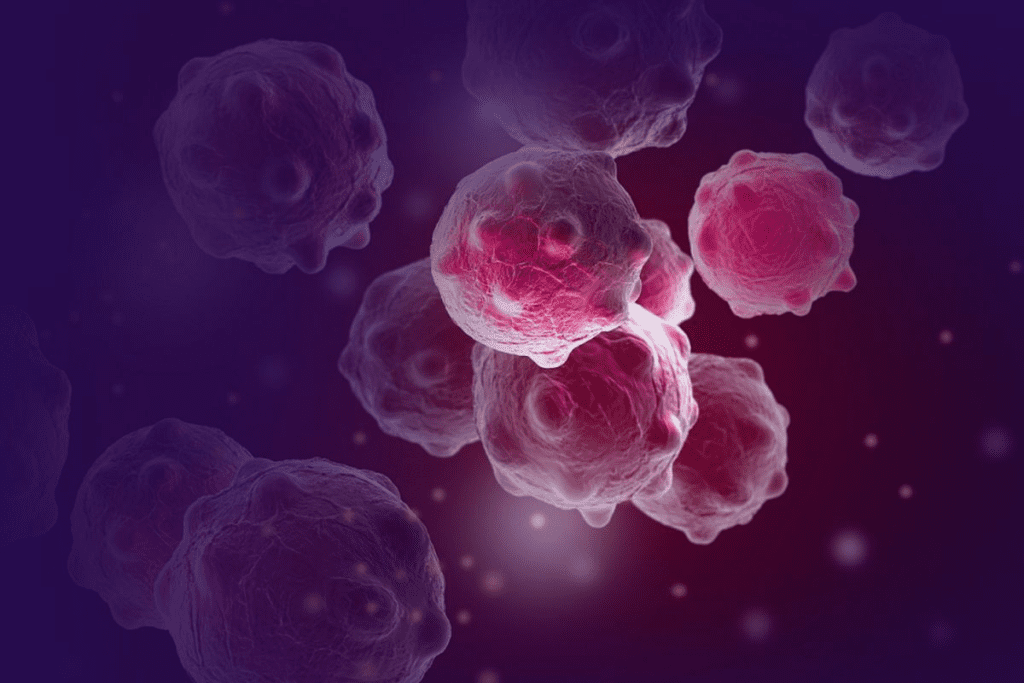
Ovarian cancer and the immune system, including white blood cells, have a complex relationship. The immune system fights cancer, and white blood cells are key in this battle.
How Cancer Affects the Immune System
Ovarian cancer can harm the immune system, changing white blood cell counts. The tumor environment can weaken or change immune cells’ function. This makes it harder for the body to fight cancer.
The immune system’s response to ovarian cancer involves different cells like neutrophils, lymphocytes, and macrophages. Each cell type has a unique role in battling cancer.
Typical Blood Count Patterns in Ovarian Cancer Patients
In ovarian cancer patients, white blood cell counts can vary. Some may have more white blood cells, while others may have fewer or normal counts.
- Leukocytosis, or high white blood cell counts, can happen due to the body’s inflammatory response to the tumor.
- Some patients may have neutropenia, or low neutrophil counts, after chemotherapy.
- Lymphocyte counts can also change, affecting the body’s fight against tumors.
Why WBC Counts May Change in Cancer Patients
Several factors can cause changes in white blood cell counts in ovarian cancer patients. The tumor can cause inflammation, leading to more white blood cells.
Treatment-related changes can also affect white blood cell counts. For example, chemotherapy can lower white blood cell counts by weakening bone marrow.
Understanding these changes is key to managing ovarian cancer well and reducing complications.
Are WBC Levels High in Ovarian Cancer?
It’s important to know about WBC levels in ovarian cancer for diagnosis and treatment. White blood cells help fight off infections and can show signs of health issues, like cancer.
Statistical Evidence on WBC Elevation in Ovarian Cancer
Research has looked into WBC levels in ovarian cancer. It found that WBC counts are higher in more advanced stages of the disease.
A study in a well-known medical journal linked high WBC counts to a worse prognosis in ovarian cancer patients. This suggests that WBC counts can help doctors understand how serious the disease is.
Differences Between Early and Advanced Stage Disease
Understanding the difference between early and advanced ovarian cancer is key. Studies show that WBC counts are usually higher in advanced stages than in early stages.
| Stage | Average WBC Count | Percentage of Patients with Elevated WBC |
| Early Stage | 8,000 cells/μL | 20% |
| Advanced Stage | 12,000 cells/μL | 60% |
When to Be Concerned About Elevated Counts
High WBC counts in ovarian cancer patients should raise concern. It’s vital to keep an eye on WBC levels, more so in advanced stages or when symptoms don’t go away.
Doctors should watch WBC counts closely and adjust treatments as needed. High WBC counts might mean it’s time for more tests or a change in treatment.
Causes of Elevated White Blood Cell Counts in Ovarian Cancer
Several factors can raise white blood cell counts in ovarian cancer patients. Knowing these causes is key to managing the disease well.
Inflammatory Response to Tumor Growth
Ovarian tumors cause an inflammatory response in the body. This response sends out cytokines and chemokines. These attract white blood cells to the tumor.
Secondary Infections and Their Impact
Ovarian cancer patients face a higher risk of secondary infections. These infections can raise WBC counts. They might come from the tumor or treatments like surgery or chemotherapy.
Paraneoplastic Syndromes and Leukocytosis
Paraneoplastic syndromes are rare disorders caused by an immune system reaction to cancer. In ovarian cancer, they can change WBC counts.
| Cause | Description | Impact on WBC Count |
| Inflammatory Response | Body’s reaction to tumor growth | Increases WBC count due to cytokine release |
| Secondary Infections | Infections related to tumor or treatment | Elevates WBC count as part of immune response |
| Paraneoplastic Syndromes | Rare disorders caused by cancer | Can lead to leukocytosis |
The Tumor Microenvironment and White Blood Cell Infiltration
The tumor microenvironment is complex and key to understanding ovarian cancer. It includes cancer cells, immune cells, and other non-cancerous cells. These cells interact in a dynamic and complex way.
Neutrophils and Their Role in Tumor Growth
Neutrophils are a type of white blood cell important in the innate immune response. In ovarian cancer, they are found in the tumor microenvironment. They can influence tumor growth and progression by releasing pro-tumorigenic factors, such as ROS and cytokines.
Lymphocytes and Anti-Tumor Immunity
Lymphocytes, including T cells and B cells, are vital for adaptive immunity. They play a key role in anti-tumor responses. Tumor-infiltrating lymphocytes (TILs) are a key part of the anti-tumor immune response. Their presence is often linked to a better prognosis in ovarian cancer patients.
- T cells can directly kill cancer cells through cell-mediated cytotoxicity.
- B cells can produce antibodies against tumor antigens, aiding in tumor recognition and destruction.
Monocytes and Macrophages in Ovarian Cancer
Monocytes and macrophages are critical in the tumor microenvironment. Monocytes can differentiate into macrophages, involved in phagocytosis and antigen presentation. Tumor-associated macrophages (TAMs) can have dual roles, either promoting or inhibiting tumor growth, depending on their polarization state.
Natural Killer Cells and Cancer Surveillance
Natural Killer (NK) cells are lymphocytes vital for cancer surveillance. They can recognize and kill cancer cells without prior antigen exposure. The presence and activity of NK cells in the tumor microenvironment are important for controlling tumor growth and metastasis.
- NK cells can directly kill tumor cells through the release of cytotoxic granules.
- NK cells can also produce cytokines that enhance anti-tumor immune responses.
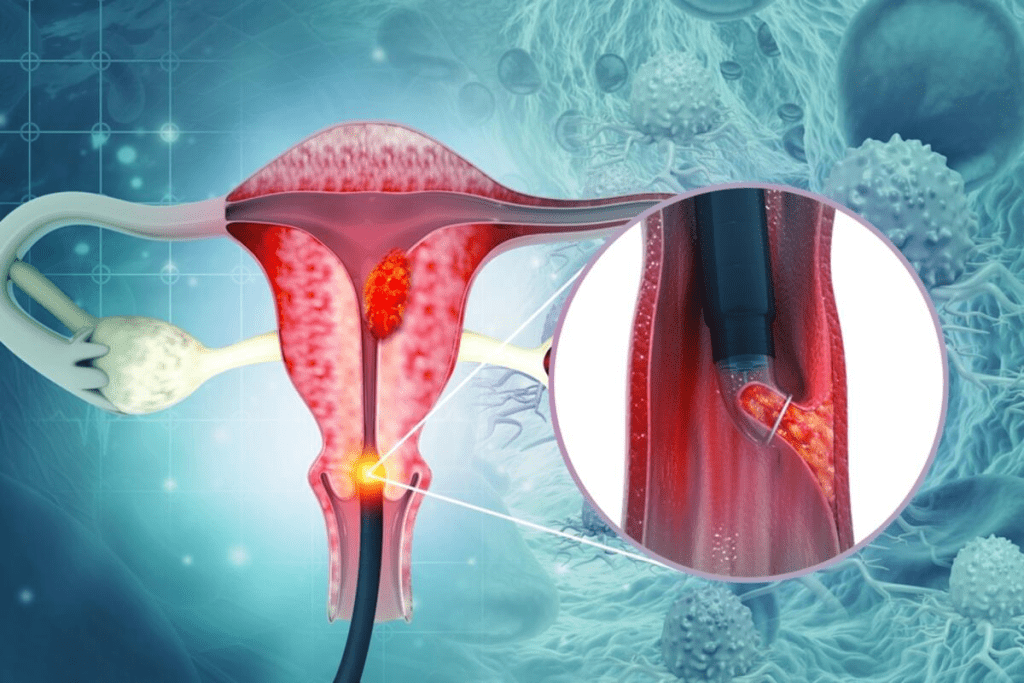
Blood Tests for Ovarian Cancer: Beyond White Blood Cell Count
Diagnosing ovarian cancer involves looking at many blood test results, not just white blood cell count. Blood tests are key in finding and managing ovarian cancer. They help see how the disease is growing and how well treatments are working.
CA-125 and Other Tumor Markers
The CA-125 test is a common blood test for ovarian cancer. CA-125 is a protein found on many ovarian cancer cells. High levels might mean cancer is present. But, it’s important to know CA-125 can also be high in other conditions, like endometriosis or pregnancy.
Other markers, like HE4, are used with CA-125 to get a clearer picture. Using several markers together can spot ovarian cancer better than one test alone.
Complete Blood Count as a Diagnostic Tool
A Complete Blood Count (CBC) is also important in ovarian cancer care. It’s not specific to ovarian cancer but shows the patient’s overall health. A CBC can show if white blood cell count is off, which might mean infection or inflammation.
Limitations of Blood Tests in Ovarian Cancer Detection
Blood tests for ovarian cancer have big limitations. No single blood test can say for sure if you have ovarian cancer. Many things can affect the results. For example, CA-125 can be high in many non-cancerous conditions, leading to false positives. Also, some cancers might not raise CA-125 levels, causing false negatives.
It’s key for doctors and patients to know these limits. Blood tests should be part of a full check-up that includes imaging, physical exams, and medical history.
Treatment Effects on White Blood Cells in Ovarian Cancer Patients
Ovarian cancer treatments can greatly affect white blood cells, which are key for fighting off infections. Chemotherapy and surgery are common treatments. They can change white blood cell counts in different ways.
Chemotherapy and WBC Suppression
Chemotherapy targets fast-growing cancer cells. But it also hits other fast-growing cells, like those in the bone marrow. This can cause a drop in neutrophils, making infections more likely.
Key effects of chemotherapy on WBC:
- Suppression of bone marrow activity
- Reduction in neutrophil count (neutropenia)
- Increased risk of infections
Surgical Interventions and Immune Response
Surgery for ovarian cancer can also affect the immune system. It aims to remove as much tumor as possible. But it can stress the body, impacting white blood cell counts.
The immune response after surgery may include:
- An initial inflammatory response
- Changes in white blood cell distribution
- Potential for immune suppression if complications arise
Managing Treatment-Related WBC Abnormalities
It’s important to manage white blood cell issues during ovarian cancer treatment. This means keeping an eye on blood counts and taking steps to reduce risks.
Strategies for managing WBC abnormalities include:
- Administering growth factors to stimulate bone marrow
- Adjusting chemotherapy doses to minimize suppression
- Implementing infection prevention measures
Understanding how treatments affect white blood cells helps doctors care for patients better. This can reduce risks and improve results.
Impact of White Blood Cells on Ovarian Cancer Survival and Prognosis
Ovarian cancer’s outcome is closely tied to the immune system, mainly through white blood cell counts. Research has shown how white blood cells affect cancer outcomes. This knowledge helps find markers for prognosis and new treatments.
Neutrophil-to-Lymphocyte Ratio as a Prognostic Marker
The neutrophil-to-lymphocyte ratio (NLR) is a key marker in many cancers, including ovarian. It’s the ratio of neutrophils to lymphocytes in blood. A high NLR is linked to a worse prognosis and lower survival rates in ovarian cancer patients.
NLR Significance: High NLR levels are tied to more advanced disease, aggressive tumors, and less treatment success. Watching NLR helps doctors spot patients at risk of poor outcomes.
Tumor-Infiltrating Lymphocytes and Survival Outcomes
Tumor-infiltrating lymphocytes (TILs) are vital for ovarian cancer prognosis. TILs are lymphocytes that fight cancer in the tumor. More TILs mean better survival and treatment response.
TILs and Prognosis: TILs in tumors suggest a strong immune fight against cancer. This has sparked research into boosting TIL activity for better treatments.
How Immune Status Affects Treatment Response
The immune status of ovarian cancer patients greatly affects treatment success. A strong immune response is key for controlling cancer and better survival.
| Immune Marker | Prognostic Significance |
| Neutrophil-to-Lymphocyte Ratio (NLR) | High NLR associated with poor prognosis |
| Tumor-Infiltrating Lymphocytes (TILs) | High TILs linked to improved survival |
| White Blood Cell Count | Abnormal counts may indicate poor outcomes |
Understanding white blood cells’ role in ovarian cancer survival is key for better treatments. By tracking immune markers and using the body’s immune power, doctors can improve patient results and fight ovarian cancer better.
Immunotherapy Approaches for Ovarian Cancer
Ovarian cancer treatment is changing with immunotherapy. This method uses the body’s immune system to fight cancer. It has shown great promise in improving patient outcomes and survival rates.
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors are a new class of drugs for cancer treatment. They include ovarian cancer. These drugs help the immune system attack cancer cells more effectively.
Examples of immune checkpoint inhibitors include:
- PD-1 inhibitors (e.g., pembrolizumab)
- PD-L1 inhibitors (e.g., atezolizumab)
- CTLA-4 inhibitors (e.g., ipilimumab)
Adoptive Cell Transfer Therapies
Adoptive cell transfer (ACT) therapies boost the immune system against cancer. In ovarian cancer, ACT therapies are showing promise in clinical trials.
Tumor-infiltrating lymphocytes (TILs) are a form of ACT therapy. T cells are taken from the tumor, grown, and then given back to the patient.
Cancer Vaccines and Immune Stimulation
Cancer vaccines aim to get the immune system to fight cancer cells. In ovarian cancer, researchers are looking at different vaccine types. These include peptide-based vaccines and dendritic cell vaccines.
Combination Approaches with Conventional Treatments
Researchers are also exploring combining immunotherapy with traditional treatments. This includes chemotherapy and surgery. These combinations might offer better results for patients.
Potential benefits of combination therapies include:
- Enhanced anti-tumor immune responses
- Improved overall survival rates
- Reduced risk of recurrence
The Role of White Blood Cell Monitoring During Ovarian Cancer Treatment
White blood cell monitoring is key in managing ovarian cancer treatment. It helps track how the body reacts to treatment. This insight is vital for healthcare providers.
Tracking Treatment Response Through WBC Changes
Doctors use white blood cell counts to check if treatment is working. Changes in WBC counts show how effective the treatment is. They also help decide if treatment needs to be changed.
Key aspects of WBC monitoring in treatment response:
- Detecting changes in WBC counts over time
- Identifying patterns that may indicate treatment efficacy
- Adjusting treatment plans based on WBC count data
Predicting Complications and Recurrence
WBC monitoring can also predict complications and cancer recurrence. Abnormal WBC counts may signal infections or tumor growth.
| WBC Count Pattern | Potential Indication |
| Elevated WBC count | Infection or inflammation |
| Low WBC count | Bone marrow suppression |
| Changing WBC count patterns | Treatment response or tumor progression |
Personalized Medicine Based on Immune Parameters
WBC monitoring data helps tailor treatment plans for each patient. It lets doctors understand a patient’s immune response. This knowledge guides more informed care decisions.
Personalized medicine approaches may include:
- Adjusting chemotherapy dosages based on WBC count
- Using immunotherapy to boost the immune system
- Monitoring for signs of treatment-related toxicity
Current Research on Immune System and Ovarian Cancer
Recent studies have uncovered the complex link between the immune system and ovarian cancer. Researchers are working hard to understand how the immune system reacts to ovarian cancer cells. They aim to use this knowledge to create new treatments.
The immune system is key in fighting cancer, with white blood cells playing a big role. Research is looking into how different white blood cells help the body fight ovarian cancer.
Emerging Biomarkers Related to White Blood Cells
Researchers are finding new biomarkers linked to white blood cells for early ovarian cancer detection. For example, studies suggest that certain ratios of neutrophils to lymphocytes could predict cancer progression.
| Biomarker | Description | Potential Use |
| Neutrophil-to-Lymphocyte Ratio (NLR) | A measure of the ratio of neutrophils to lymphocytes in the blood | Prognostic indicator for ovarian cancer |
| Platelet-to-Lymphocyte Ratio (PLR) | A measure of the ratio of platelets to lymphocytes | Predictive marker for treatment response |
Novel Immune-Based Therapeutic Approaches
New immune-based treatments are being developed for ovarian cancer. These include immune checkpoint inhibitors and adoptive cell transfer therapies. These aim to boost the immune system’s fight against cancer cells.
The Future of Immune Monitoring in Ovarian Cancer
The future of immune monitoring in ovarian cancer looks promising. Advanced technologies will help track immune system changes during treatment. This could lead to more personalized treatments.
As research deepens, we can expect better diagnostic tools and treatments for ovarian cancer.
Conclusion: The Significance of White Blood Cell Counts in Ovarian Cancer Management
Understanding white blood cells in ovarian cancer is key. WBC counts show if cancer is present, how it’s growing, and how well the body is fighting it.
Studies show WBC counts are important for predicting ovarian cancer outcomes. High WBC counts often mean a worse prognosis. This shows how white blood cells affect survival rates.
Watching WBC counts helps doctors see how well treatments are working. It also helps spot problems early. This info helps doctors make better treatment plans, which can lead to better results for patients.
The link between white blood cells and ovarian cancer is complex. It involves many immune cells and how they interact with tumors. More research is needed to understand this better and find new ways to fight cancer.
By focusing on WBC counts in ovarian cancer care, doctors can make better treatment plans. This can lead to better care and outcomes for patients.
FAQ
Are white blood cell counts always elevated in ovarian cancer?
No, not all ovarian cancer patients have high white blood cell counts. Some may have normal or even low counts.
What is the relationship between white blood cells and ovarian cancer?
White blood cells are key in fighting ovarian cancer. The tumor environment can change their types and numbers. This affects how the cancer grows and how well treatments work.
Can ovarian cancer cause changes in white blood cell counts?
Yes, ovarian cancer can change white blood cell counts. The tumor can cause inflammation, raising counts. But treatments can lower them.
How do different types of white blood cells relate to ovarian cancer?
Different white blood cells have different roles in ovarian cancer. Neutrophils might help the tumor grow. But lymphocytes can fight the cancer.
What is the significance of the neutrophil-to-lymphocyte ratio in ovarian cancer?
The neutrophil-to-lymphocyte ratio is important in ovarian cancer. High ratios often mean worse survival chances.
Can immunotherapy be used to treat ovarian cancer?
Yes, immunotherapy is a promising treatment for ovarian cancer. It includes immune checkpoint inhibitors and adoptive cell transfer therapies.
How do blood tests, including white blood cell counts, aid in ovarian cancer diagnosis?
Blood tests, like complete blood counts and CA-125, help diagnose ovarian cancer. But they have their limits.
What is the impact of chemotherapy on white blood cells in ovarian cancer patients?
Chemotherapy can lower white blood cell production. This increases infection risk and can affect treatment success.
Can white blood cell monitoring predict treatment response and outcomes in ovarian cancer?
Yes, tracking white blood cell counts can predict treatment success. It helps track response and guide treatment plans.
What are the future directions in ovarian cancer research related to white blood cells?
Future research includes new immune therapies and biomarkers. It also aims to integrate immune monitoring into care.
How does the tumor microenvironment influence white blood cell infiltration in ovarian cancer?
The tumor environment can change how white blood cells work. This affects cancer growth and treatment success.
Are there any specific white blood cell abnormalities associated with ovarian cancer?
Yes, certain white blood cell changes, like leukocytosis, are linked to ovarian cancer.
References
- National Cancer Institute. (2023). Ovarian, fallopian tube, and primary peritoneal cancer”Patient version. https://www.cancer.gov/types/ovarian