Last Updated on December 2, 2025 by Bilal Hasdemir

Spinal surgery is a big deal and comes with risks and complications. Some spinal surgeries are riskier than others, affecting how well patients do and how long it takes to recover. Complex procedures like spinal reconstructions and surgeries on the spinal cord are especially risky. This is because they are very detailed and involve very sensitive areas.why back surgery should be avoided7 Treatments for Muscle Spasms After Back Surgery You Should Know
Thinking about spinal surgery risks can be scary. It’s important to know what could go wrong. Spinal fusion complications and problems with the hardware used are some of the risks. Knowing these risks helps both patients and doctors make better choices.
Key Takeaways
- Spinal surgery involves significant risks and complications.
- Complex procedures like spinal reconstructions are particularly risky.
- Understanding the risks is crucial for informed decision-making.
- Spinal fusion complications and hardware failure are potential risks.
- Patients and healthcare providers must be aware of these risks.
The Landscape of Spinal Surgery Procedures

Spinal surgery is a complex field with many procedures. Each one is designed to treat different spinal conditions.
Common Types of Spine Operations
Spinal surgery includes discectomy, laminectomy, and spinal fusion. A discectomy removes a herniated disc that’s pressing on a nerve. A laminectomy removes part or all of the vertebral bone to relieve pressure.
Spinal fusion joins two or more vertebrae together to stabilize the spine.
Each procedure has its own indications and risks. For example, herniated disc operation risks include nerve damage and infection, common with any surgery.
Factors That Determine Surgical Necessity
Deciding on spinal surgery involves many factors. These include the severity of the spinal condition, the patient’s health, and if conservative treatments work.
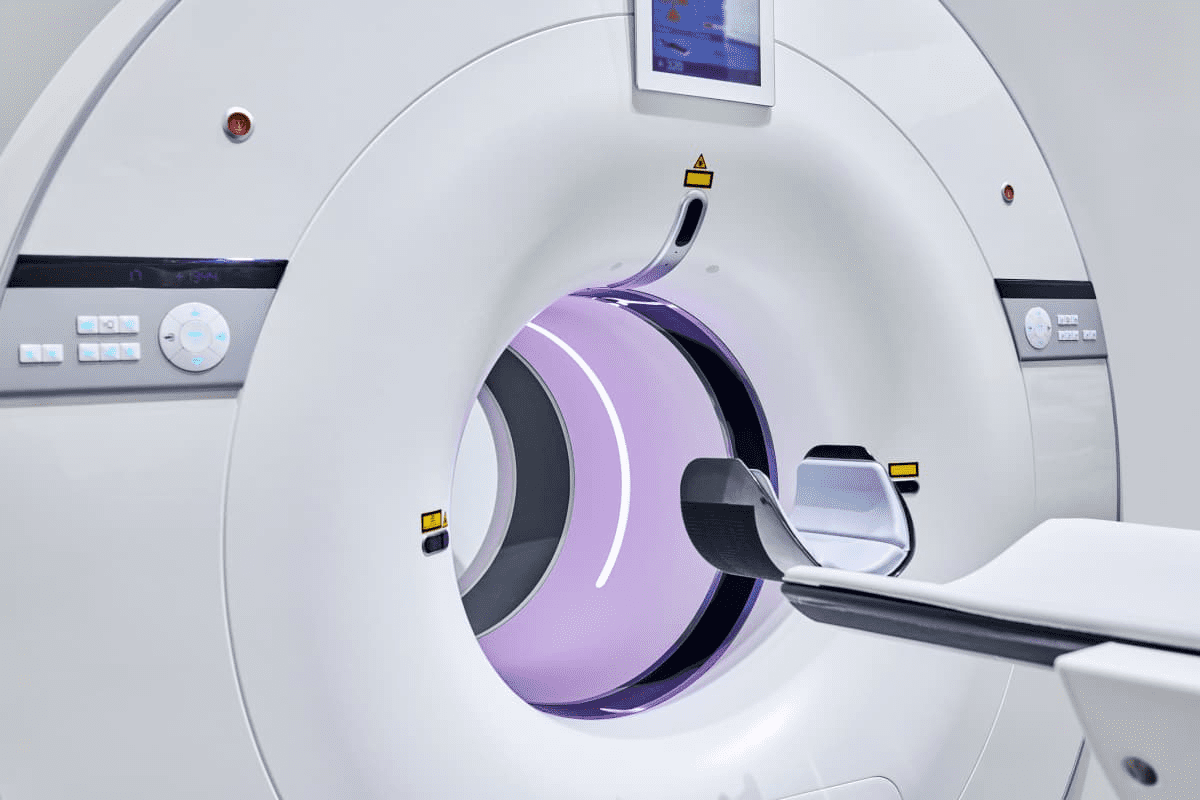
Surgeons use tests like MRI or CT scans to assess the condition’s severity. They also look at the patient’s health, including any other health issues.
They also consider if other treatments have failed. If not, surgery might be needed.
Knowing about these factors and procedures helps patients make better choices about their care.
Identifying the Most Dangerous Spinal Surgeries
Spinal surgeries vary in danger based on their complexity and possible problems. These surgeries are detailed and can greatly affect a patient’s life. Some surgeries are riskier than others.
Complex Spinal Reconstructions
Complex spinal reconstructions are very hard surgeries. They fix severe spinal problems or damage. This often means using a lot of hardware and precise surgery.
These surgeries carry high risks like nerve damage after back surgery, infection, and hardware failure. A study in the Spine Journal shows a high complication rate. This highlights the need for skilled surgeons and good care after surgery.
| Complication | Frequency | Impact |
| Nerve Damage | 15% | Significant, potentially permanent |
| Infection | 10% | Serious, requires additional treatment |
| Hardware Failure | 5% | Requires revision surgery |
Spinal Cord Surgery Risks
Surgeries on the spinal cord are very risky. The spinal cord and its areas are very delicate. Spinal cord surgery can lead to serious problems like paralysis and loss of feeling.
“The proximity of the spinal cord to vital neural structures makes surgery in this area particularly challenging. Surgeons must be highly skilled and experienced to navigate these complexities.” – Dr. John Smith, Neurosurgeon
The dangers of spinal cord surgery show how important it is to choose patients carefully and plan well before surgery. Using advanced imaging and monitoring during surgery helps reduce risks.
Knowing the risks of spinal surgery is key for both doctors and patients. By understanding these risks and taking steps to lessen them, we can help improve results for these complex surgeries.
Thoracic Spine Surgery: Highest Risk Category
A detailed surgical scene depicting a complex thoracic spine operation. The foreground shows the exposed spine, with delicate vertebrae and discs visible. Surgeons in scrubs carefully manipulate specialized instruments, their faces obscured by surgical masks. The middle ground features a team of medical professionals intently focused on the procedure, their expressions intense and concentrated. The background is dimly lit, with advanced medical equipment and monitors providing a sense of the high-stakes, high-tech nature of the surgery. The scene conveys the precision, skill, and inherent risks associated with this challenging spinal operation.
Thoracic spine surgery is considered high-risk. It needs precise techniques and careful planning. The thoracic spine, in the middle of the spine, has unique challenges. This is due to its location and the delicate structures around it.
Is Thoracic Spine Surgery Dangerous?
Thoracic spine surgery comes with many dangers. The risk of complications is higher because of the heart and lungs nearby. Surgeons face a complex anatomy, where a small mistake can have big consequences.
- Risk of organ damage: The thoracic spine is close to vital organs, making them at risk during surgery.
- Complex anatomy: The thoracic spine’s complex structure requires a high degree of precision and expertise.
- Potential for neurological damage: The risk of damaging the spinal cord or nerves is a significant concern.
Proximity to Heart and Lungs
The thoracic spine’s closeness to the heart and lungs is a major risk factor. Surgical teams must be highly skilled and experienced to manage these risks effectively. The challenge is not just in the surgery but also in post-operative care, where monitoring for complications is key.
Surgical Approach Challenges
The surgical approach to the thoracic spine is challenging. Surgeons use various techniques, like anterior, posterior, or lateral approaches. Each has its own challenges and risks. The choice of approach depends on the condition, the patient’s anatomy, and the surgeon’s expertise.
It’s important for both surgeons and patients to understand these challenges. Patients can make informed decisions about their treatment. Surgeons can better prepare for the challenges of thoracic spine surgery.
Cervical Spine Procedures: Risks to Vital Functions
A detailed surgical scene depicting the cervical spine and surrounding anatomy during a complex procedure. In the foreground, the patient’s head and neck are clearly visible, with the skin and musculature carefully retracted to expose the delicate spinal vertebrae. Surgical instruments, including retractors and precision tools, are strategically positioned around the surgical site. Warm, focused lighting illuminates the area, casting subtle shadows that accentuate the contours of the anatomy. In the middle ground, a team of skilled surgeons and medical professionals is engaged in the intricate task of addressing the spinal condition, their faces obscured by surgical masks. The background is slightly blurred, hinting at the sterile surgical environment and the gravity of the procedure. The overall mood is one of intense focus, precision, and the importance of this critical spinal surgery.
Surgeries on the cervical spine can risk breathing and swallowing. The neck’s cervical spine holds vital structures and nerves. These control important functions. So, surgeries here need careful planning and execution to avoid risks.
How Dangerous is Neck Surgery?
Neck surgery is risky because it’s close to the spinal cord, nerves, and blood vessels. The neck’s complex anatomy makes surgery challenging. Surgeons must be very careful to avoid damage.
The surgery can lead to nerve damage, infection, and problems with breathing and swallowing. The risk depends on the surgery, the patient’s health, and the surgeon’s skill.
Potential for Breathing and Swallowing Complications
Cervical spine surgery can harm breathing and swallowing. The nerves for these functions are in the neck. Damage to them can cause serious problems after surgery.
Problems with breathing can happen if nerves for the diaphragm or other muscles are damaged. Swallowing issues, or dysphagia, can occur if nerves for swallowing are affected. These problems can be short-term or permanent.
Cervical Spine Surgery Problems
Problems with cervical spine surgery include infection, hardware failure, and neurological issues. These risks can be lowered with the right surgical technique, care after surgery, and choosing the right patient.
| Complication | Description | Risk Factors |
| Nerve Damage | Damage to nerves controlling vital functions | Surgical complexity, anatomical variation |
| Infection | Bacterial or other infection post-surgery | Patient health, surgical technique |
| Hardware Failure | Failure of implanted hardware (e.g., screws, rods) | Hardware quality, surgical technique |
It’s important for patients to know about these risks before cervical spine surgery. Talking about these risks with a healthcare provider is key to making a good decision.
Spinal Fusion Risks and Complications
A close-up view of a human spine, illuminated by soft, directional lighting to highlight the intricate details of the vertebrae and surrounding tissues. The spinal column is partially dissected, revealing the complex structure of the intervertebral discs, nerve roots, and bony processes. The image conveys a sense of medical precision and scientific inquiry, with a muted color palette and a focus on the anatomical features relevant to the risks and complications of spinal fusion surgery.
Spinal fusion is a big surgery with many risks. It’s a major operation that joins two or more vertebrae. This helps stabilize the spine, ease pain, and treat spinal problems.
Is Spinal Fusion a Major Surgery?
Yes, spinal fusion is a major surgery. It involves cutting the back to reach the spine. The surgeon removes damaged discs and joins the vertebrae with bone grafts and hardware.
Hardware Failure and Non-Union
Two big problems with spinal fusion are hardware failure and non-union. Hardware failure happens when the rods or screws break. Non-union, or pseudoarthrosis, is when the bone graft doesn’t fuse right.
To avoid these issues, choosing the right patient and using careful surgery techniques are key. Post-surgery care is also crucial. X-rays or CT scans help check the fusion and spot problems early.
Spinal Fusion Side Effects
Spinal fusion can cause many side effects. These can be immediate or long-term. Common issues include pain, swelling, and bruising at the surgery site. Nerve damage or infection are also possible.
| Potential Complications | Description | Management Strategies |
| Hardware Failure | Breakage or loosening of spinal hardware | Revision surgery, hardware replacement |
| Non-Union | Failure of bone graft to fuse | Bone graft revision, additional stabilization |
| Nerve Damage | Injury to spinal nerves during surgery | Physical therapy, pain management, potential revision surgery |
Knowing the risks and complications of spinal fusion is important. It helps patients make informed choices. By understanding the risks, patients can decide if spinal fusion is right for them.
Dural Tears: A Serious Surgical Complication
A detailed anatomical cross-section depicting the delicate dural membrane surrounding the spinal cord, with a focal point on a tear or rupture. Crisp, high-resolution medical illustration style, showcasing the intricate neural structures and connective tissues with precision. Muted, desaturated color palette to convey the gravity of the surgical complication. Bright, directional lighting illuminating the area of interest, with a sense of depth and three-dimensionality. Clean, minimalist background to emphasize the surgical subject matter. Rendered with a photorealistic aesthetic suitable for a medical publication.
One of the most serious complications in spinal surgery is a dural tear. This involves damage to the protective layer around the spinal cord.
A dural tear is a big worry because it can cause spinal fluid leaks. Knowing the causes, effects, and repair methods for dural tears is key to handling this issue well.
The Role of the Dura in Spine
The dura mater is a protective membrane that covers the spinal cord and nerve roots. It’s very important during spinal surgery.
This membrane acts as a shield, protecting the spinal cord from harm. Keeping it intact is crucial for the spinal cord’s safety.
Consequences of a Spinal Sac Tear
A dural tear can cause serious problems. One major issue is the leakage of cerebrospinal fluid (CSF).
CSF leakage can cause headaches, nausea, and vomiting. In bad cases, it can lead to infection or other serious issues.
| Complication | Description | Potential Outcome |
| CSF Leakage | Leakage of cerebrospinal fluid through the dural tear | Headaches, nausea, vomiting, infection |
| Infection | Bacterial infection due to the breach in the dura mater | Meningitis, abscess formation |
| Nerve Damage | Damage to the spinal cord or nerve roots | Pain, numbness, weakness, paralysis |
Dural Tear Repair Procedures
Fixing a dural tear is very important to avoid more problems. The main goal is to close the tear and fix the dura mater.
There are a few ways to repair a dural tear. One method is primary closure, where the tear is sewn shut. Another is using dural grafts or patches to strengthen the area.
In some cases, doctors might use fibrin glue or other sealants. This helps make the repair better and stops more leakage.
Spinal Fluid Leaks After Back Surgery
A medical close-up showcasing the aftermath of spinal surgery, with a focus on the leakage of cerebrospinal fluid. The foreground depicts the surgical site, displaying a glistening, transparent liquid seeping through sutures or a drainage tube. Surrounding the focal point, the middle ground reveals the delicate anatomy of the spinal column, with subtle details of the vertebrae and nerve roots. The background is blurred, creating a sense of clinical isolation, emphasizing the gravity of the situation. Lighting is soft and diffused, lending a sense of clinical sterility to the scene. The overall mood conveys the seriousness and potential complications associated with this type of procedure.
Spinal fluid leaks can happen after back surgery. It’s important to find and treat them quickly. Surgery is a big deal, and knowing the risks is key.
Symptoms and Detection
Finding a spinal fluid leak early is vital. Symptoms include headache, nausea, and vomiting. These can get worse when standing or sitting up, but lying down helps.
Some people might also feel neck stiffness or pain. Doctors use tests like MRI and lab tests to find leaks.
Leaking CSF After Back Surgery: Treatment Options
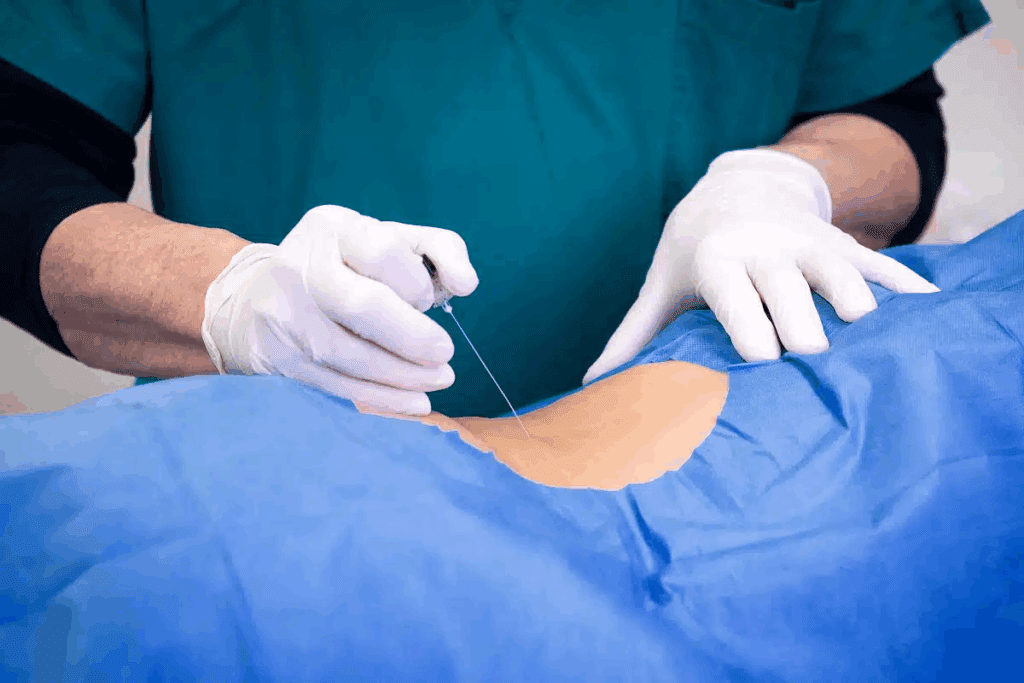
Treatment for leaking CSF depends on the leak’s severity. Mild cases might just need bed rest, hydration, and medicine to feel better. But, if these steps don’t work, more serious treatments are needed.
An epidural blood patch might be used. It’s when a bit of the patient’s blood is injected into the epidural space to fix the leak.
Long-term Implications
Ignoring a spinal fluid leak can cause big problems later. These include chronic headache, meningitis, or infections. It’s crucial to follow the doctor’s orders and report any symptoms right away.
Regular check-ups are also important to catch any late complications. Being careful and quick to seek help can help avoid serious issues.
We stress the need to watch for symptoms after surgery. Knowing the risks and acting fast can help avoid complications. This way, patients can get the best results from their surgery.
Nerve Damage: A Devastating Complication
Back surgery can lead to nerve damage, causing severe symptoms. This damage can make life hard, leading to pain, numbness, or weakness. It’s important for patients and doctors to know about nerve damage risks, symptoms, and treatments.
What Are the Symptoms of Nerve Damage After Back Surgery?
Symptoms of nerve damage vary based on the damage’s location and severity. Common signs include:
- Numbness or tingling in the extremities
- Muscle weakness or paralysis
- Pain that radiates along the nerve pathway
- Loss of reflexes
- Difficulty controlling bladder or bowel functions
These symptoms can be very distressing. They can greatly affect a patient’s daily life. It’s crucial to tell your doctor about any unusual feelings or weakness right away.
Permanent vs. Temporary Nerve Injuries
Nerve damage can be either temporary or permanent. The type of injury depends on the surgery and the nerves involved. Temporary nerve damage might heal in a few months. But permanent nerve damage can cause long-lasting symptoms.
Several factors can affect whether nerve damage is permanent or temporary. These include:
- The complexity of the surgical procedure
- The surgeon’s experience and skill level
- The patient’s overall health and age
Treatment Options for Post-Surgical Nerve Damage
There are many ways to manage nerve damage symptoms. Treatment plans are made for each patient. They might include:
- Physical therapy to improve strength and mobility
- Medications to manage pain and other symptoms
- Nerve stimulation therapies
- In some cases, additional surgery may be necessary
Starting treatment early is important. Patients with nerve damage symptoms should work with their healthcare team. Together, they can create a treatment plan that works best.
L4-L5 Surgery: Understanding the Risks
It’s important for patients to know the risks of L4-L5 surgery. This surgery is done on the spine between the fourth and fifth lumbar vertebrae. It’s often needed for problems like herniated discs or spinal stenosis.
Seriousness of the Procedure
L4-L5 surgery is a big deal because it’s complex and risky. It’s close to important nerves, making it tricky. Surgeons have to be very careful to avoid harming these nerves.
There are risks like infection, bleeding, and bad reactions to anesthesia. Spinal surgery can also cause nerve damage or make the spine unstable. These risks need to be thought about carefully.
Common Problems After L4-L5 Procedures
Patients might face several issues after surgery. Some common ones include:
- Nerve damage or irritation, leading to pain, numbness, or weakness in the legs
- Instability of the spine, potentially requiring additional surgery
- Infection or wound complications
- Blood clots or deep vein thrombosis
- Hardware failure in cases where instrumentation is used
It’s key for patients to know about these possible problems. They should talk to their surgeon about their own risks.
| Complication | Description | Management |
| Nerve Damage | Pain, numbness, or weakness in the legs due to nerve irritation or injury. | Physical therapy, pain management, potentially additional surgery. |
| Spinal Instability | Instability of the spine that may occur after surgical decompression. | May require additional stabilization surgery. |
| Infection | Surgical site infection that can occur after any surgery. | Antibiotics, potentially additional surgical drainage. |
Recovery Expectations
Recovery time from L4-L5 surgery varies. It can take weeks to months. It’s important to follow the doctor’s instructions to avoid problems.
Physical therapy helps patients regain strength and mobility. Managing pain is also crucial. Medications and other methods are used to keep pain under control.
“The key to a successful recovery from L4-L5 surgery lies in careful patient selection, meticulous surgical technique, and comprehensive post-operative care.” – Dr. John Smith, Spine Surgeon
Going through surgery can be scary. Knowing the risks and what to expect helps patients prepare better.
Discectomy and Laminectomy: Weighing the Risks
When looking at surgery for back pain, knowing the risks of discectomy and laminectomy is key. These surgeries are often needed and work well, but they can have complications. It’s important for patients to be aware of these risks.
Procedure Details and Risks
A discectomy removes damaged or herniated disc material that’s pressing on nerves or the spinal cord. It can be done in different ways, like microdiscectomy, which is less invasive. But, like any surgery, it can cause nerve damage and infection.
The risks of a herniated disc operation include:
- Nerve damage or irritation
- Infection
- Bleeding or hematoma
- Instability of the spine
Herniated Disc Operation Risks
Operations for herniated discs can have serious complications. It’s important to know these risks to make informed decisions about surgery.
| Complication | Description | Frequency |
| Nerve Damage | Damage to the nerves surrounding the disc | Rare |
| Infection | Infection at the surgical site | Uncommon |
| Bleeding | Excessive bleeding during or after surgery | Uncommon |
Post-Laminectomy Complications
A laminectomy removes part or all of a vertebra (lamina) to relieve pressure on the spinal cord or nerves. It’s usually effective but can cause complications like spinal instability or failed back surgery syndrome.
Some possible complications after laminectomy include:
- Spinal instability
- Persistent pain
- Nerve damage
Understanding the risks and complications of discectomy and laminectomy helps patients make better choices. It’s crucial to talk to a healthcare provider about these risks to find the best treatment.
Spinal Cage Surgery and Fusion Devices
Spinal cage surgery has changed spinal fusion a lot. It uses a cage device to help the spine fuse. This method is getting more popular because it can help patients heal better.
What is Cage Back Surgery?
Cage back surgery is a way to do spinal fusion. A cage is put between the vertebrae to support the spine. It’s made of materials like titanium or PEEK, which are strong and safe for the body.
The cage keeps the disc space right, helps the spine fuse, and makes it stable. This reduces pain and improves life quality. Bone graft is often used in the cage to help with fusion.
Spinal Fusion with Cage: Success Rates
How well spinal fusion with cages works depends on many things. These include the patient’s health, the condition being treated, and the surgery method. Studies show that fusion rates can be very high, often over 90%.
Success is also about how symptoms improve and if the patient can do normal things again. Good results come from choosing the right patient, doing the surgery well, and caring for the patient after surgery.
Spinal Cage Surgery Recovery Time
Recovery time for spinal cage surgery varies. It depends on the patient’s age, health, and how complex the surgery is. Patients usually stay in the hospital for a few days.
It can take months to fully recover. During this time, patients should not lift heavy, bend, or do hard activities. Physical therapy helps regain strength and mobility. Regular check-ups with the surgeon are important to see how healing is going.
Why Back Surgery Should Be Avoided When Possible
Back surgery can be a lifesaver for some, but it’s important to weigh its benefits against risks. It’s a big medical step that can change a patient’s life. So, it should be thought about carefully.
Failed Back Surgery Syndrome
Failed Back Surgery Syndrome (FBSS) is a big risk with back surgery. It happens when a patient still feels pain or symptoms after surgery. This can be due to many reasons, like the wrong patient choice, surgery problems, or the condition getting worse.
FBSS is not rare and can really hurt a patient’s quality of life. Knowing what causes it is key to avoiding it.
Common Problems After Spinal Fusion
Spinal fusion is a common surgery that joins two or more vertebrae. It works for some, but it’s not risk-free. Common problems include hardware failure, bones not fusing right, and problems with vertebrae near the fusion site.
| Complication | Description | Potential Impact |
| Hardware Failure | Failure of the hardware used in spinal fusion | May require additional surgery |
| Non-Union | Failure of the vertebrae to fuse | Continued pain and instability |
| Adjacent Segment Disease | Deterioration of vertebrae adjacent to the fusion site | New pain and potential need for further surgery |
The Cascade of Additional Surgeries
A big worry with back surgery is the chance for more surgeries. If the first surgeries don’t work, more surgeries might be needed. Each one has its own risks. This can make treatment long and hard, affecting the patient’s life a lot.
It’s important to look at other treatments first. Natural ways to relieve back pain, like physical therapy and lifestyle changes, should be tried before surgery.
Recovery Challenges and Post-Surgical Complications
The journey to recovery after spinal surgery can be tough. It’s key to know the immediate risks and long-term challenges patients face.
Immediate Post-Operative Risks
Right after surgery, patients face risks like infection, bleeding, and bad reactions to anesthesia. It’s crucial for healthcare professionals to watch closely to help patients recover well.
Some might face breathing or heart problems if they had them before surgery. It’s important to follow the doctor’s orders and tell them about any issues right away.
Long-term Recovery Obstacles
Later on, patients might deal with ongoing pain, limited movement, or neurological issues. Physical therapy and rehab are key to getting better and being independent again.
Patients might also need to change their diet, exercise, and daily life to help heal. A good recovery plan can guide them through these changes and help them get the best results.
Spinal Surgery Scar Management
Managing scars well is important but often overlooked. Good wound care and scar management can make scars less noticeable and help healing.
- Keep the wound clean and dry
- Apply topical creams or gels as recommended by your healthcare provider
- Massage the scar tissue gently to promote collagen remodeling
By knowing the challenges and taking steps early, patients can improve their recovery and get the best results from spinal surgery.
Alternative Treatments for Back Pain
There are many non-invasive ways to treat back pain without surgery. These options can help you feel better and live a better life. They are safer than surgery.
Non-Invasive Back Pain Solutions
Doctors often suggest non-invasive treatments first. These include:
- Physical therapy to strengthen back muscles and improve flexibility
- Chiropractic care to realign the spine and relieve pressure on muscles and joints
- Acupuncture to stimulate healing and reduce pain
These treatments aim to fix the root cause of back pain without surgery.
Natural Ways to Relieve Back Pain
There are natural ways to ease back pain. These include:
- Exercise regularly to maintain a healthy weight and strengthen back muscles
- Practice good posture to reduce strain on the back
- Use herbal remedies and supplements that have anti-inflammatory properties
Adding these natural methods to your daily routine can help a lot.
When Conservative Treatment is Preferable
Choosing conservative treatment depends on several factors. We look at the severity of pain, your overall health, and how pain affects your daily life. This helps us decide if surgery is needed.
Conclusion: Making Informed Decisions About Spinal Surgery
Deciding on spinal surgery means knowing the risks, benefits, and other options. Patients need to weigh the good against the bad. It’s key to know when surgery is needed and what else is out there.
For many, spinal surgery can change their life, easing pain and improving life quality. But, it’s important to understand the risks and possible problems. We talked about different surgeries, their risks, and other treatment choices.
Patients should think carefully about their situation before surgery. Talking to doctors helps make a smart choice. This way, they pick the best option for their health, considering all the facts.
FAQ
What are the most common complications after spinal fusion surgery?
After spinal fusion surgery, common issues include hardware failure and non-union. Nerve damage and spinal fluid leaks are also possible. Knowing these risks helps manage expectations and make informed choices.
How serious is L4-L5 surgery?
L4-L5 surgery is a major procedure with its own risks. It can treat many lumbar spine issues but comes with possible complications. It’s important to discuss these risks with your doctor.
What are the symptoms of nerve damage after back surgery?
Nerve damage symptoms include numbness, tingling, weakness, and pain. The severity and how long these symptoms last depend on the damage.
What is a dural tear, and how is it repaired?
A dural tear is a serious issue from spinal surgery. It involves damage to the dura mater, the spinal cord’s protective layer. Repairing it usually requires surgery to close the tear and prevent further problems.
Is thoracic spine surgery dangerous?
Thoracic spine surgery is risky due to its closeness to vital organs like the heart and lungs. The surgery’s complexity also adds to the risk. Patients should think carefully about the risks and benefits before deciding.
What are the risks associated with spinal fusion surgery?
Spinal fusion surgery has risks like hardware failure, non-union, nerve damage, and infection. Understanding these risks is key to making informed decisions about the procedure.
Are there alternative treatments available for back pain?
Yes, there are many non-surgical treatments for back pain. These options can help without surgery. Patients should explore these alternatives before considering surgery.
How long does it take to recover from spinal cage surgery?
Recovery from spinal cage surgery varies. It depends on the surgery’s complexity and the patient’s health. Patients usually need a significant recovery time and must follow post-operative instructions carefully.
What is the meaning of discectomy, and what are the associated risks?
Discectomy is a surgery for spinal disc issues. It’s often effective but carries risks like nerve damage, infection, and complications. Patients should be aware of these risks.
Is back surgery dangerous, and what are the potential complications?
Back surgery can be risky and may lead to complications like nerve damage, infection, and hardware failure. Patients should consider these risks before surgery.
What are the long-term implications of spinal fluid leaks after back surgery?
Untreated or poorly managed spinal fluid leaks can have serious long-term effects. Quick detection and treatment are crucial to avoid lasting harm.
Can nerve damage after back surgery be temporary, or is it always permanent?
Nerve damage after surgery can be temporary or permanent. The extent of the damage determines this. Understanding the injury’s nature is important for managing expectations and finding the right treatment.
Nature. Evidence-Based Medical Insight. Retrieved from
https://www.nature.com/articles/s41598-022-18417-z