
Stem cell transplants give kids with serious blood cancers and rare genetic disorders a second chance. We use stem cell therapy to treat diseases like leukemia and lymphoma by replacing bad stem cells with healthy ones.
Getting a stem cell transplant is a major step for children. It’s a complex process that requires careful planning and care. Stem cell therapy works by adding healthy stem cells, which then create normal blood cells and can cure the disease.
Understanding what stem cells are and how they function is essential. They have the unique ability to turn into many different types of cells in our bodies. Success stories, such as a successful bone marrow baby transplant, highlight the power of this treatment in saving young lives.
Key Takeaways
- Stem cell transplants are used to treat life-threatening conditions like leukemia and lymphomas.
- The process involves replacing damaged stem cells with healthy ones.
- Stem cell therapy has shown impressive survival outcomes due to advances in pediatric transplant care.
- Understanding stem cells and their function is key to seeing the benefits of stem cell transplants.
- Comprehensive care is essential for children undergoing stem cell transplants.
Understanding Stem Cell Transplants in Pediatric Patients
Stem cell transplants have changed the way we treat some diseases in kids. They offer hope to families all over the world. This complex procedure replaces a child’s sick or damaged stem cells with healthy ones.
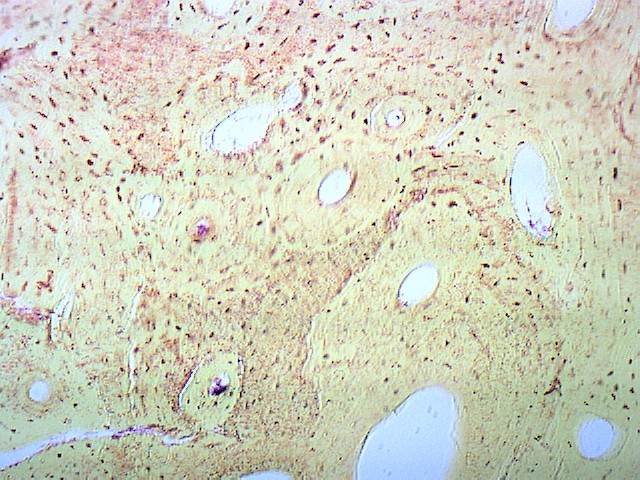
What Are Stem Cells and How Do They Work?
Stem cells are important because they turn into different blood cells. This includes red blood cells, white blood cells, and platelets. They help the body make new blood cells, which is key to treating blood-related issues.
Stem cell transplantation uses these cells to fix a child’s bone marrow. This can save the lives of kids with certain diseases.

Differences Between Adult and Pediatric Transplants
Pediatric stem cell transplants are different from adult ones. Kids’ health, the disease being treated, and how they react to the transplant vary from those of adults.
Studies show that over 89% of kids survive a year after a transplant. This shows how far pediatric stem cell transplants have come.
Every child is unique, and transplant decisions are made with their specific needs in mind. This ensures the best care for each child.
Life-Threatening Conditions Requiring Stem Cell Transplantation
Life-threatening conditions like leukemia and severe aplastic anemia need quick medical help. Often, this means a stem cell transplant. Without the right treatment, these conditions can greatly harm a child’s life and chances of survival.
Stem cell transplants are a key treatment for many blood disorders in kids. We’ll look at some serious conditions that might need this procedure.
Leukemia and Lymphomas in Children
Leukemia is a common cancer in kids, with acute lymphoblastic leukemia (ALL) being the most common. Lymphomas are less common but just as serious. A stem cell transplant is considered when these cancers don’t respond to usual treatments or come back after treatment.
Doctors decide on a stem cell transplant for kids with leukemia or lymphoma after checking the disease’s severity and the child’s health. Early treatment can greatly increase the chances of survival.
Severe Aplastic Anemia
Severe aplastic anemia is a rare but deadly condition where the bone marrow can’t make blood cells. Stem cell transplantation is usually the best option, mainly when other treatments don’t work.
The success of stem cell transplantation for severe aplastic anemia depends on several things. These include finding a good donor and the child’s health. Quick diagnosis and treatment are key to better results.
High-Risk Acute Myeloid Leukemia (AML)
High-risk AML is a blood cancer with fast-growing, abnormal white blood cells. Stem cell transplantation is often suggested for kids with high-risk AML, after they’ve had chemotherapy to get into remission.
Stem cell transplants have shown good results in treating high-risk AML. But the success depends on how well the child responds to initial treatment and if a compatible donor is found.
About 20% of kids who get a transplant develop chronic graft-versus-host disease. This can affect their long-term health and quality of life. It’s important to manage this complication for the transplant’s success.
Genetic and Immune System Disorders Treated with Stem Cell Therapy
Stem cell therapy is a key treatment for many genetic and immune system disorders in kids. These issues often stem from immune system flaws or genetic mutations. Stem cell transplants can replace or fix damaged cells, potentially curing or greatly improving the lives of these children.
Severe Combined Immunodeficiency (SCID)
Severe Combined Immunodeficiency (SCID) is a serious condition where kids are born without a working immune system. This makes them very prone to infections. SCID happens when B and T cells, key to the immune system, don’t work right. Wiskott-Aldrich syndrome, another immunodeficiency, also benefits from this therapy.
B cells grow in the bone marrow, while T cells grow in the thymus. In SCID, these cells don’t mature properly. Stem cell transplants can fix this by introducing healthy cells that can grow into working B and T cells.
Inherited Metabolic Disorders
Inherited metabolic disorders affect how the body breaks down food. They can cause toxic substances to build up, harming organs. Stem cell transplants can replace bad cells with healthy ones, potentially stopping or reversing disease.
Conditions like Hurler syndrome and adrenoleukodystrophy are treated with stem cell therapy. The goal is to give the body cells the ability to make the needed enzymes or fix metabolic problems.
Other Genetic Conditions Benefiting from Transplantation
Stem cell therapy also helps with other genetic conditions. This includes certain anemias, like Fanconi anemia, and other immune disorders. The aim is to fix the genetic issue and restore normal cell function.
Thanks to better treatment plans and care teams, kids are living longer and recovering better after stem cell transplants. Tailored treatments help ensure the best outcomes for each patient.
The Path to a Successful Bone Marrow Baby: From Diagnosis to Treatment
Getting a successful bone marrow transplant in kids needs a detailed plan. It starts with finding out what’s wrong and then treating it. New ways of caring for kids have made survival rates better, giving families hope.
Initial Diagnosis and Evaluation Process
The first step to a successful transplant is finding out what’s wrong. We use many tools to get a clear picture of the child’s health. This includes looking at their medical history, doing physical checks, and running lab tests.
It’s important to know how we can get stem cells for the transplant. Stem cells can come from donors or the child themselves. The evaluation helps figure out the best source for the child.
Finding a Compatible Donor
After deciding a transplant is needed, finding a matching donor is key. We do HLA typing to find a donor with the right tissue type. We look at family members, unrelated donors, and cord blood units for a match. The transplant process depends on finding the best donor to avoid problems.
Preparing a Child for Transplantation
Getting ready for a transplant means making the child’s body ready. We do a conditioning regimen to get rid of bad cells and weaken the immune system. We also take care of any side effects and make sure the child is healthy for the transplant. Knowing the bone marrow transplant failure symptoms helps us watch the child’s health after the transplant.
As kids grow, they can handle treatments better. Learning about when males mature mentally and physically helps us support them more. It makes their recovery from transplants easier.
By managing each step of the transplant process well, we can help kids recover better. Our team works with families to give the best care. This ensures kids have a good quality of life during and after treatment.
Types of Stem Cell Transplants for Children
Stem cell transplants offer hope for kids with severe diseases. Knowing the different types is key. The choice depends on the child’s condition, health, and donor availability.
Autologous Transplants: Using the Child’s Own Cells
Autologous transplants use the child’s stem cells. They’re often used for some cancers. The child’s stem cells are collected, stored, and then given back after chemotherapy.
The big plus of autologous transplants is that they avoid graft-versus-host disease (GVHD). GVHD is a serious issue where donor cells attack the body.
Allogeneic Transplants: Donor-Derived Stem Cells
Allogeneic transplants use stem cells from a donor. This donor can be a sibling, parent, or unrelated match. They’re used for genetic disorders or certain leukemias.
The success of these transplants depends on HLA matching. Top centers report over 89% one-year survival rates for kids. This shows allogeneic transplants can be very successful.
Cord Blood Transplants: A Valuable Alternative
Cord blood transplants use stem cells from the umbilical cord. They’re great when an adult donor isn’t available. They have a lower GVHD risk than other transplants.
They’re also quick to use when needed urgently. This makes them a good choice for some patients.
In summary, the transplant type for a child depends on their condition and donor availability. Knowing about autologous, allogeneic, and cord blood transplants helps families make better choices for their child’s care.
The Transplantation Procedure: What Parents Should Expect
Understanding the stem cell transplant process is key for parents. It includes pre-transplant prep, the infusion, and post-transplant care. We’ll walk you through these steps, sharing what to expect and how to prepare.
Pre-Transplant Conditioning Regimens
Before the transplant, kids get a conditioning regimen. This uses chemotherapy and sometimes radiation. It:
- Gets rid of cancer cells, if there are any
- Weakens the immune system to lower rejection risk
- Makes room in the bone marrow for new stem cells
This part can be tough and may cause side effects like tiredness, nausea, and hair loss. Our team will watch your child closely and help manage these side effects.
The Stem Cell Infusion Process
The infusion is like a blood transfusion. The stem cells, from a donor or your child, are given through a central line. The whole process usually takes a few hours, with our team watching your child’s health closely. The stem cells are frozen and may have special protectants to keep them safe.
“The actual infusion is quite simple,” says, a top pediatric hematologist. “But the prep and care afterward are very important.”
Immediate Post-Transplant Care
After the infusion, your child will be watched closely in a clean area to avoid infections. This period is very important because their immune system is weak. We’ll give:
- Supportive care, like antibiotics and other meds to fight off infections
- Food support to help your child get better
- Emotional support for your child and your family
About 20% of kids might get chronic graft-versus-host disease (GVHD). This is when the donor’s immune cells attack the recipient’s body. Our team is ready to handle GVHD and other issues, aiming for the best results for your child.
We’re here to give your family all the care and support you need. Knowing what to expect helps you support your child better during this tough time.
Recovery and Outcomes: Creating a Successful Bone Marrow Baby
Families need to know about the recovery and outcomes of bone marrow transplants for kids. Thanks to medical progress, kids have better chances of success with stem cell transplants.
Current Survival Statistics for Pediatric Transplants
Recent studies show big improvements in survival rates for kids getting transplants. Top hospitals report over 89% of kids survive the first year. This success comes from better care plans and teamwork among doctors.
Survival rates depend on many things. These include the child’s health before the transplant, the type of transplant, and the disease being treated.
Factors Affecting Transplant Success
Several important factors can influence the success of a bone marrow transplant in kids. These include:
- Donor compatibility: A well-matched donor greatly boosts the chances of success.
- Pre-transplant conditioning regimens: Getting the patient ready for the transplant is key.
- Post-transplant care: Good follow-up care helps manage risks and ensures the best outcome.
These factors work together to affect the transplant’s success.
Measuring Quality of Life After Transplantation
Checking the quality of life after a transplant is complex. Doctors look at many things, including:
- Physical health and any lasting side effects
- Emotional and mental health
- How well the child can fit back into social activities
By focusing on these areas, healthcare teams aim to improve the quality of life for kids after a transplant.
Potential Complications and Management Strategies
Stem cell transplantation offers hope for many children. But it comes with risks and complications. Knowing these and how to manage them is key to good care.
Graft-Versus-Host Disease Incidence and Impact
Graft-versus-host disease (GVHD) is a big risk after allogeneic stem cell transplantation. It happens when the donor’s immune cells attack the recipient’s body. About 20% of kids get chronic GVHD, affecting the skin, liver, and gut.
Managing GVHD well is vital to avoid long-term harm and improve life quality for these kids.
“GVHD is a major challenge in allogeneic transplantation,” say top researchers. It’s all about finding the right balance in managing GVHD without harming the immune system too much.
Infection Risks and Prevention
Infections are a big worry after a stem cell transplant. The treatment and immunosuppression weaken the immune system. Preventing infections is key, with antimicrobial therapy and isolation. We also watch for early signs of infection and start treatment quickly to avoid serious problems.
- Prophylactic antimicrobial therapy
- Strict isolation protocols
- Monitoring for signs of infection
Long-Term Side Effects and Monitoring
Children who survive a stem cell transplant may face long-term side effects. These include endocrine issues, secondary cancers, and psychosocial problems. Long-term care is vital to catch these issues early and treat them. We help families create follow-up plans that meet each child’s needs.
“Long-term follow-up care is not just about monitoring for complications; it’s about supporting the overall well-being of our young patients as they grow and develop.”
In summary, stem cell transplantation is a powerful treatment but comes with risks. Knowing these risks and how to manage them is essential. By tackling these challenges, we can improve outcomes and quality of life for children undergoing stem cell transplant.
Multidisciplinary Care and Innovative Approaches
Pediatric stem cell transplantation is complex. It needs a team effort. A full team is key for successful bone marrow transplants in kids.
The Team Behind Successful Pediatric Transplants
A team is essential for kids’ stem cell transplants. This team has doctors, surgeons, nurses, and more. They all work together for the best care.
They make sure every part of a child’s health is covered. This is from the start to after the transplant.
Each team member is important:
- Pediatric hematologists and oncologists find and treat the problem.
- Transplant surgeons do the transplant.
- Nurses give critical care and support.
- Psychologists and social workers help with emotional and social needs.
Academic Protocols Improving Outcomes
Academic protocols help a lot in pediatric stem cell transplants. Top places keep updating their plans with new research. This means patients get the best and safest treatments.
Important parts of these plans include:
- Pre-transplant plans are made just for the child.
- New ways to give stem cells.
- Post-transplant care to help recovery.
Innovative Care Pathways at Leading Institutions
Top places use new ways to help patients. They use personalized medicine and join clinical trials. This makes care better for kids with stem cell transplants.
What makes these places stand out is:
- They focus on teamwork.
- They keep up with research and trials.
- They use the latest in technology and treatments.
- They care for the whole child, not just their health.
By working together and trying new things, we can make stem cell transplants better. This leads to more successful bone marrow transplants for kids.
Supporting Your Child Through the Transplant Journey
Starting a stem cell transplant journey is tough, with many emotional and psychological challenges for families. We’re here to help you understand these complex issues.
Psychological and Emotional Considerations
The transplant process can be emotionally taxing for both the child and the family. It’s key to tackle the psychological effects of treatment. This ensures a supportive setting. We suggest getting professional psychological support to manage stress and uncertainty.
Families find counselling services and support groups very helpful. They offer a space to share experiences and get advice from others facing similar situations.
Educational and Social Reintegration
Rejoining daily life, like school and social activities, is a big step towards recovery. Work closely with your child’s healthcare team to plan for their educational and social needs.
Educational reintegration programs help your child catch up on schoolwork and adjust to physical changes post-transplant. Keeping social connections through support groups or activities also boosts their emotional health.
Resources for Families of Transplant Recipients
Families get extra support during and after the transplant journey. We offer counselling, educational materials, and connections to other families who’ve been through it.
Using these resources can greatly improve your child’s recovery and your family’s well-being. For example, knowing when males mature mentally helps understand their long-term psychological needs.
By using these resources and staying in touch with your healthcare team, you can better manage the transplant journey. This ensures the best outcomes for your child.
Conclusion: Hope and Healing Through Stem Cell Transplantation
Stem cell transplantation has changed how we treat serious diseases in kids. It brings new hope and healing. We’ve looked at how it works, the care needed, and new ways to help.
A successful bone marrow transplant can change a child’s life and their family’s. It uses stem cells to give a second chance at life. This is for kids with leukemia, lymphoma, and other genetic diseases.
We keep improving in stem cell transplantation. Our goal is to give top-notch care to international patients. Our team works hard to make sure every child gets the best care, from start to finish.
The path to a successful bone marrow transplant is tough. But with the right support, families can face it with hope. We aim to bring hope and healing through stem cell transplantation. We’re excited to keep exploring new ways to treat childhood diseases.
FAQ’s:
What is a stem cell transplant?
A stem cell transplant replaces a child’s damaged stem cells with healthy ones. These can come from the child or a donor.
How does stem cell therapy work?
Stem cell therapy introduces healthy stem cells into the body. These cells then produce new blood cells, replacing the old ones.
What are the differences between autologous and allogeneic stem cell transplants?
Autologous transplants use the child’s own stem cells. Allogeneic transplants use stem cells from a donor. Autologous is often used for cancer, while allogeneic treats more conditions, like genetic disorders.
What is SCID, and how is it treated with stem cell transplantation?
SCID is a genetic disorder that weakens the immune system. Stem cell transplantation can treat it by introducing healthy stem cells.
What are the risks and complications associated with stem cell transplantation?
Risks include graft-versus-host disease and infection risks. Long-term side effects are also possible. A team of experts helps manage these risks for the best results.
How is a compatible donor found for a stem cell transplant?
Donors are found by testing family members and unrelated donors. The donor’s HLA type is matched to the child’s for compatibility.
What is the role of cord blood in stem cell transplantation?
Cord blood is a valuable stem cell source for transplants. It’s useful when a matched donor is not available, for both related and unrelated transplants.
What are the survival statistics for pediatric stem cell transplants?
Survival rates vary based on the condition, transplant type, and other factors. Advances in care have improved outcomes, with many children surviving long-term and living well after transplant.
How is the quality of life measured after stem cell transplantation?
Quality of life is measured by the child’s physical, emotional, and social well-being after transplant. Their ability to do normal activities, health, and mental state are considered.
What kind of support is available for families undergoing stem cell transplantation?
Families get support through counselling, educational resources, and social support. A team of experts is there to help the child and their family during the transplant process.
References
- Dana-Farber/Boston Children’s Pediatric Stem Cell Transplant Program. (2025). Pediatric Stem Cell Transplant Program. https://www.dana-farber.org/cancer-care/treatment/pediatric-stem-cell-transplant


































