Last Updated on November 26, 2025 by Bilal Hasdemir

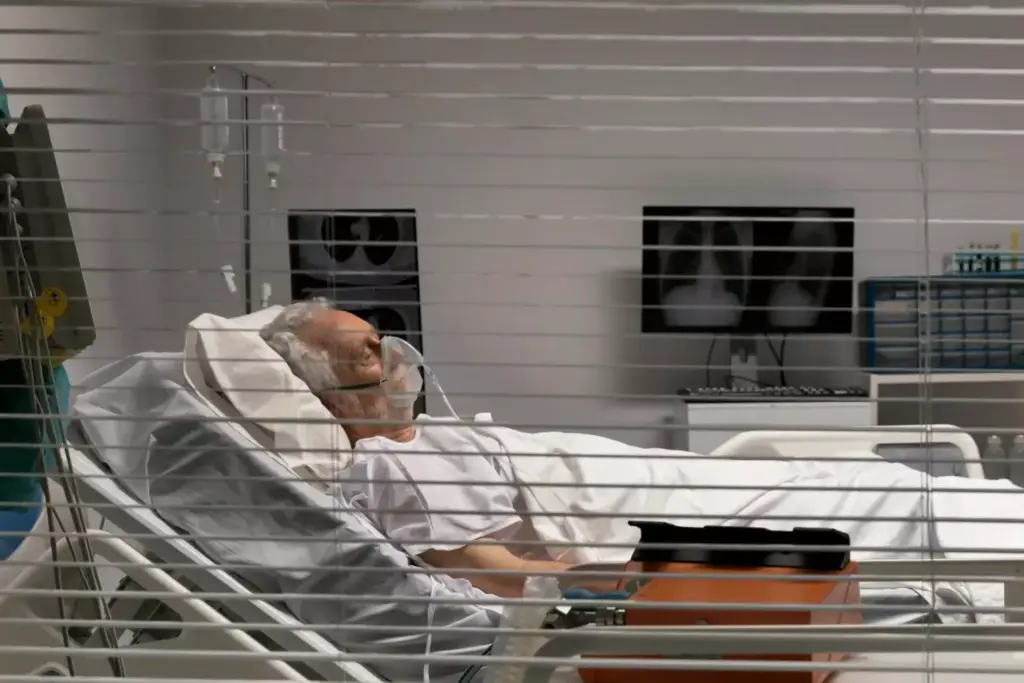
Cancer treatment, like chemotherapy, often makes patients very tired. This tiredness, called cancer-related fatigue, affects up to 90% of those getting treatment. At Liv Hospital, we know how much this exhaustion affects patients’ lives. Studies show that cancer-related fatigue makes simple tasks hard.
We know that fighting fatigue after chemotherapy is key for patients to get stronger. By understanding why chemotherapy and tiredness happen, we can help patients more during their treatment.
Key Takeaways
- Cancer-related fatigue affects up to 90% of chemotherapy patients.
- Understanding the causes of fatigue is key to managing it.
- Liv Hospital is dedicated to helping patients through cancer treatment.
- Managing fatigue is vital for improving patients’ quality of life.
- Supportive care is essential for those undergoing chemotherapy.
The Prevalence of Cancer-Related Fatigue
It’s important to know how common cancer-related fatigue is. This issue affects many patients going through cancer treatment. It’s a complex problem that impacts a lot of people.
Statistics on Fatigue Among Cancer Patients
Research shows that up to 90% of cancer patients feel tired during chemotherapy (Hanna et al., 2018). This shows how widespread cancer-related fatigue is. It can make daily activities hard to do.
Fatigue after chemotherapy treatment is common. Many patients feel tired long after treatment ends. It affects their body, mind, and emotions.
Differentiating Normal Tiredness from Cancer Fatigue
It’s key to tell normal tiredness from cancer-related fatigue. Normal tiredness goes away with rest, but cancer fatigue doesn’t. Knowing this helps patients and doctors manage it better.
Cancer fatigue lasts a long time and really affects a patient’s life. It’s not just from being tired. It makes daily tasks hard.
Impact on Quality of Life
Chemo fatigue has a big impact on a patient’s life. It affects their health, feelings, and social life. Patients might feel lonely or upset because they can’t do things they love.
Understanding and tackling cancer-related fatigue is key to better patient care. By recognizing its effects, doctors can help more. They can teach ways to manage fatigue and improve life quality.
Understanding Chemo and Tiredness: The Direct Connection
Chemotherapy can cause a chain of effects that lead to extreme tiredness in many patients. We will look into how chemotherapy directly causes this exhausting condition.
How Chemotherapy Affects Energy Production
Chemotherapy targets cells that grow fast, including some healthy ones that help make energy. This can stop the body from making energy, making people feel very tired. The effect on energy production is a key reason for chemotherapy-induced fatigue.
Cellular Damage and Energy Depletion
Chemotherapy can harm cells, leading to less energy (Altomare et al., 2022). Damaged cells can’t work right, including making energy for the body. This damage adds to the tiredness patients feel during chemotherapy.
Variability of Fatigue Based on Treatment Types
The type of chemotherapy can affect how tired patients feel. Different treatments have different effects on the body, with some causing more tiredness. Knowing the specific treatment and its side effects can help manage expectations and fatigue.
We know that each patient’s experience with chemotherapy and tiredness is different. It depends on the type of cancer, treatment, and their health. By understanding the link between chemotherapy and tiredness, we can help patients deal with this tough side effect.
The Biological Mechanisms Behind Chemotherapy Fatigue
Fatigue from chemotherapy is more than just feeling tired. It’s a complex issue tied to many biological processes. Millions of cancer patients worldwide face this problem, which greatly affects their life quality. We will look into the biological reasons behind this side effect.
Cytokine Production and Inflammation
Cytokine production and inflammation are key in causing chemotherapy fatigue. Studies show that chemotherapy boosts pro-inflammatory cytokines, which spark inflammation in the body (Gupta et al., 2012). This inflammation messes with the body’s functions, making patients feel tired. Inflammation disrupts normal cellular processes, contributing to the exhaustion experienced by cancer patients.
Some important points about cytokine production and inflammation are:
- Chemotherapy can trigger the release of pro-inflammatory cytokines.
- Increased cytokine levels can lead to systemic inflammation.
- Inflammation can impair energy production at the cellular level.
Mitochondrial Dysfunction
Mitochondrial dysfunction is another major factor in chemotherapy-induced fatigue. Mitochondria are the cells’ powerhouses, making energy. Chemotherapy can harm these organelles, making it hard for them to produce energy. This mitochondrial dysfunction can lead to a decrease in ATP (adenosine triphosphate) production, which is essential for various cellular functions.
The effects of mitochondrial dysfunction on fatigue include:
- Reduced energy production due to impaired mitochondrial function.
- Increased oxidative stress, further damaging cellular components.
- Potential long-term effects on cellular energy metabolism.
Muscle Wasting and Weakness
Muscle wasting and weakness are common in cancer patients on chemotherapy, adding to their fatigue. Chemotherapy can cause a loss of muscle mass and strength, making daily tasks harder. Muscle wasting not only affects physical function but also contributes to the overall feeling of exhaustion.
Factors contributing to muscle wasting and weakness include:
- Chemotherapy-induced changes in metabolism.
- Reduced physical activity due to treatment-related fatigue.
- Nutritional deficiencies that impact muscle health.
Understanding these biological mechanisms is key to managing chemotherapy-induced fatigue. By tackling the root causes, healthcare providers can offer better ways to improve cancer patients’ quality of life.
Anemia: A Major Contributor to Chemo Exhaustion
Anemia is a big reason why cancer patients feel tired during chemotherapy. It happens when the body doesn’t have enough red blood cells or when those cells don’t carry enough oxygen. Chemotherapy can stop the body from making enough red blood cells, leading to anemia.
Impact of Chemotherapy on Red Blood Cell Production
Chemotherapy fights cancer by targeting fast-growing cells. But it also affects the bone marrow, where red blood cells are made. This can cause a drop in red blood cell production, leading to anemia. Studies show that anemia from chemotherapy is common in cancer patients, making them feel more tired and exhausted.
The Link Between Hemoglobin Levels and Energy
Hemoglobin carries oxygen to the body’s tissues. Low hemoglobin means less oxygen for the body, causing tiredness and weakness. Lower hemoglobin levels mean less oxygen for the body’s tissues, making fatigue worse.
Importance of Monitoring Blood Counts During Treatment
Checking blood counts, including hemoglobin, is key in managing anemia from chemotherapy. Regular tests help doctors see how bad the anemia is and what to do next. Early treatment of anemia can greatly improve the lives of cancer patients on chemotherapy by cutting down on fatigue and boosting energy.
Here are some ways to manage anemia:
- Regular blood count checks
- Iron supplements or other treatments as advised by doctors
- Blood transfusions when needed
- Eating foods rich in iron and other nutrients
By understanding how chemotherapy affects red blood cells and keeping an eye on hemoglobin levels, we can fight anemia. This helps reduce fatigue in cancer patients.
Psychological Factors Intensifying Cancer Fatigue
It’s important to know how psychological factors make cancer fatigue worse. A cancer diagnosis and treatment can deeply affect a person’s mental health. This can lead to emotional distress, sleep problems, and a mix of fatigue and depression.
Emotional Distress and Energy Levels
Emotional distress is a big factor that makes cancer fatigue worse. The emotional weight of a cancer diagnosis and the stress of treatment can increase anxiety and depression. A study found that emotional distress can take a lot of energy, making it hard to deal with treatment demands.
It’s key to tackle emotional distress to manage fatigue well.
Patients with high emotional distress can benefit from help to reduce anxiety and depression. This help can include counseling, cognitive-behavioral therapy, and other supportive care. By lessening emotional distress, we can boost energy and improve life quality for cancer patients.
Sleep Disturbances During Treatment
Sleep problems are another big factor that makes cancer fatigue worse. Side effects of treatment, pain, and emotional distress can disrupt sleep. Sleep issues not only slow down physical recovery but also make fatigue and tiredness worse. It’s important to ensure good sleep and find ways to improve sleep quality to manage fatigue.
Improving sleep hygiene is key. This includes keeping a regular sleep schedule, making a sleep-friendly environment, and avoiding things that can keep you awake before bed. By fixing sleep problems, we can lessen the severity of fatigue in cancer patients.
The Vicious Cycle of Fatigue and Depression
Fatigue and depression can make a bad cycle that’s hard to get out of. Fatigue can lead to depression, and depression can make fatigue worse. To break this cycle, we need a plan that tackles both the physical and mental sides of fatigue.
“The link between fatigue and depression shows we need a treatment plan that includes mental support and ways to manage fatigue.”
By understanding and tackling the psychological factors that make cancer fatigue worse, we can offer better support to patients. This includes managing emotional distress, improving sleep, and breaking the cycle of fatigue and depression.
Timeline of Fatigue During and After Chemotherapy
Knowing when fatigue happens during chemotherapy is key. It helps patients and doctors plan better. Fatigue from chemotherapy can start at different times and last for varying lengths.
Acute Fatigue: During and Immediately After Sessions
Many patients feel very tired during and right after chemotherapy. This feeling of being extremely exhausted is common. It happens because chemotherapy kills off fast-growing cells in the body.
Cumulative Fatigue: The Building Effect
As chemotherapy goes on, fatigue gets worse. This is because the body keeps getting tired from each treatment. The body also builds up toxins from the chemotherapy.
Post-Treatment Persistence: Months to a Year
Studies show that fatigue can last for months to a year after treatment ends. How long it lasts depends on the cancer type, treatment intensity, and the person’s health.
When to Expect Improvement
Fatigue usually starts to get better slowly after treatment stops. But, how fast it improves varies. Health, other health issues, and how well fatigue is managed play a big role.
| Period | Characteristics of Fatigue | Expected Improvement |
|---|---|---|
| During Chemotherapy | Acute and cumulative fatigue; intense tiredness | Variable, depends on treatment cycle |
| Immediately After Chemotherapy | Peak fatigue levels; significant exhaustion | Gradual improvement expected |
| Post-Treatment (Months to a Year) | Gradual decrease in fatigue; potentially persistent | Improvement varies; influenced by health and management strategies |
By knowing when fatigue happens, patients and doctors can tackle it better. This makes life better for those going through chemotherapy.
Communicating About Fatigue with Your Healthcare Team
Talking about your fatigue with your healthcare team can really help your treatment. It’s important to work together to manage cancer-related fatigue. By sharing your symptoms and worries, you get better support and care.
Tracking and Reporting Your Symptoms
It’s key to track and report your fatigue symptoms well. Keeping a diary can help you see how bad your fatigue is and when it happens. This makes it easier to talk about with your healthcare team.
Tips for Tracking Fatigue:
- Record the severity of your fatigue daily
- Note any factors that seem to improve or worsen your fatigue
- Bring your diary to appointments to discuss with your healthcare team
When to Seek Immediate Medical Attention
While fatigue is common with cancer treatment, sometimes it means something serious. Knowing when to get help right away is important.
| Symptom | Action |
|---|---|
| Severe fatigue that interferes with daily activities | Contact your healthcare team |
| Signs of anemia, such as pale skin or shortness of breath | Seek immediate medical attention |
| Fatigue accompanied by other concerning symptoms like fever or pain | Consult your healthcare provider promptly |
Working with Your Oncology Team on Fatigue Management
Working with your oncology team is key to managing fatigue. Together, you can find the best ways to help you feel better and live better.
Good communication is more than just talking about symptoms. It’s about sharing your worries, what you prefer, and any changes in your health. This teamwork makes sure your care is just right for you.
Medical Interventions for Managing Chemo Fatigue
Managing chemotherapy fatigue needs a mix of medical steps to help patients. At Liv Hospital, we know how important it is to tackle this side effect. We aim to improve our patients’ quality of life during chemotherapy.
Pharmacological Approaches
One key way to fight chemotherapy fatigue is through medicine. Medications like psychostimulants can boost alertness and energy. But, we watch for side effects closely.
Antidepressants and anti-anxiety medications also play a role. They help by tackling the mind’s part in fatigue. Our team at Liv Hospital picks the best medicine for each patient.
Blood Transfusions and Iron Supplementation
Blood transfusions and iron help with anemia, a big cause of fatigue. They increase red blood cells and oxygen to tissues. This cuts down on fatigue a lot.
At Liv Hospital, we check blood counts often. This helps us decide if blood transfusions or iron are needed. Our experts make sure patients get the right treatment.
Addressing Underlying Conditions
Managing fatigue also means fixing any other health issues. This includes pain, nutrition, and other medical problems.
Our team at Liv Hospital works together to create a detailed care plan. We make sure to tackle all factors that cause fatigue.
Liv Hospital’s Approach to Cancer-Related Fatigue
Liv Hospital is dedicated to caring for patients with chemotherapy fatigue. We use a mix of medical steps, tailored for each patient.
We use the latest research and treatments to improve patient outcomes. Our team focuses on caring for the whole person, not just the fatigue.
Lifestyle Strategies to Combat Cancer Treatment Exhaustion
Managing cancer treatment exhaustion needs a mix of lifestyle changes. These changes help improve well-being. By adopting certain habits, patients can fight fatigue and live better during and after treatment.
Energy Conservation Techniques
One key way to fight fatigue is to save energy. This means focusing on what’s important, taking breaks, and not overdoing it. Here are some tips:
- Make a daily plan that balances rest and activity
- Ask family or friends for help when you can
- Use tools like canes or walkers to save energy
Nutrition and Hydration Strategies
Eating right and drinking enough water are key to fighting fatigue. Nutritional strategies include:
- Eat small meals often to keep energy up
- Choose foods rich in nutrients, like fruits, veggies, and lean proteins
- Stay away from foods high in caffeine and sugar
Physical Activity and Exercise Recommendations
Even though it might seem odd, gentle exercise can help fight fatigue. Good activities include:
- Short walks or light stretching
- Yoga or tai chi to improve balance and reduce stress
- Swimming or water aerobics for a low-impact workout
Sleep Hygiene Practices
Good sleep habits are vital for managing fatigue. Patients can benefit from:
- Keeping a regular sleep schedule
- Having a calming bedtime routine, like reading or meditation
- Avoiding screens and exciting activities before bed
By using these lifestyle tips, cancer patients can manage exhaustion better and improve their life quality.
Conclusion: Moving Forward with Hope Beyond Fatigue
Understanding and managing cancer-related fatigue is key for better living during chemotherapy. With the right care and support, patients can feel much better. This helps them face the challenges of fatigue head-on.
Studies, like the one by Carlson et al. in 2023, show the need for a full approach to fight fatigue. Mixing medical help with lifestyle changes helps patients deal with chemotherapy exhaustion. This includes saving energy, eating right, staying active, and getting enough sleep.
Hope and support are vital for patients moving forward. Fighting chemo fatigue is tough, but with the right help, patients can get through it. Working with their healthcare team and using available resources, patients can find hope and improve their life quality.
FAQ
What is cancer-related fatigue?
Cancer-related fatigue is a deep and lasting tiredness linked to cancer and its treatment, like chemotherapy. It’s not just feeling tired. It can really hurt a patient’s life quality.
How common is fatigue among cancer patients undergoing chemotherapy?
Fatigue is a big side effect of chemotherapy, hitting most patients. It can really lower a person’s life quality during and after treatment.
Why does chemotherapy cause fatigue?
Chemotherapy can make you tired by messing with how your body makes energy. It can also damage cells and cause anemia. The type and strength of treatment play a big role in how tired you get.
How can anemia contribute to fatigue during chemotherapy?
Anemia, caused by chemotherapy’s impact on making red blood cells, lowers hemoglobin. This makes it hard for your body to carry oxygen, leading to tiredness and weakness.
Can psychological factors influence fatigue during cancer treatment?
Yes, feelings like sadness, trouble sleeping, and depression can make you feel more tired. It’s important to handle these feelings to feel better during treatment.
How long does chemotherapy fatigue last?
How long you feel tired from chemotherapy can vary. It might start during treatment, last after it’s over, and sometimes for months or even a year. Everyone recovers at their own pace.
What can be done to manage chemotherapy fatigue?
To fight chemotherapy fatigue, you need medical help and lifestyle changes. This includes fixing anemia, saving energy, eating right, staying hydrated, exercising gently, and getting enough sleep.
Why is it important to communicate fatigue symptoms to the healthcare team?
Telling your healthcare team about your tiredness is key. It helps them create a plan to help you feel better. This improves your life quality during and after treatment.
Are there any medical interventions for managing chemotherapy-induced fatigue?
Yes, there are treatments like medicines, blood transfusions, iron pills, and fixing anemia. Places like Liv Hospital offer treatments that fit each person’s needs.
How can patients conserve energy during chemotherapy?
To save energy, focus on what’s important, take breaks, and don’t push yourself too hard. Using energy-saving tips, eating well, and staying hydrated can help fight fatigue.
Can physical activity help with chemotherapy fatigue?
Yes, gentle exercises that fit your health can help beat chemotherapy fatigue. Always talk to your doctor before starting any new exercise.
What role does sleep hygiene play in managing fatigue?
Good sleep habits, like regular sleep times, a comfy sleep space, and avoiding activities before bed, can improve sleep. This helps reduce tiredness.