Last Updated on November 26, 2025 by Bilal Hasdemir

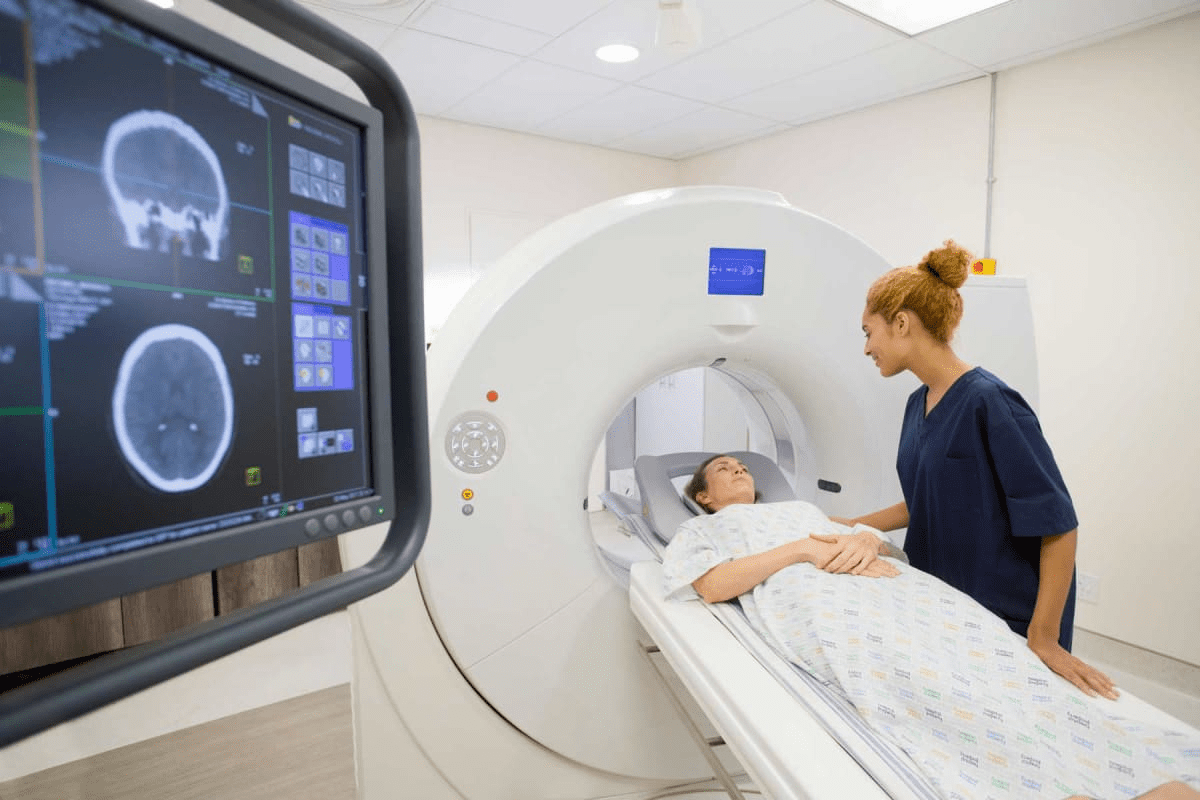
Feeling very tired after cancer treatment is a big challenge for many patients. At Liv Hospital, we know that understanding why this happens can help with recovery. It also makes life better for those who have beaten cancer.
Research shows that up to 80% of patients feel very tired after cancer treatment. We see how this side effect can really hurt a patient’s life quality. Our aim is to give top-notch care to patients from around the world who need advanced treatments.
Key Takeaways
- Chemotherapy fatigue affects up to 80% of cancer patients.
- Understanding the causes of cancer treatment exhaustion is key for getting better.
- Liv Hospital offers care that focuses on the patient and uses the latest methods to fight chemo tiredness.
- Good management can make a big difference in a survivor’s daily life.
- Comprehensive care is vital for international patients looking for top medical treatments.
The Prevalence and Impact of Cancer-Related Tiredness
Cancer-related fatigue is a big problem that affects millions of people around the world. It’s not just feeling tired; it’s a complex issue that can really change a person’s life during and after treatment.
We will look at the numbers of cancer-related fatigue and how it affects patients every day. Fatigue can be different for everyone, but it’s a common problem in cancer care.
Statistics: 80% of Patients Experience Significant Fatigue
Research shows that about 80% of cancer patients feel very tired during treatment. This number shows how common the problem is and why we need better ways to manage it.
| Patient Group | Percentage Experiencing Fatigue |
|---|---|
| Undergoing Chemotherapy | 80% |
| Receiving Radiation Therapy | 70% |
| Post-Treatment | 40% |
How Fatigue Affects Quality of Life During Treatment
Cancer-related tiredness can really change a patient’s life. It can make it hard to do everyday things, keep up with friends, and follow treatment plans. Fatigue affects not just the body but also the mind and feelings.
Key areas affected by cancer-related fatigue include:
- Physical functioning and mobility
- Cognitive function and concentration
- Emotional well-being and mood
- Social interactions and relationships
It’s important to understand these effects to create better care plans. Plans that help the whole person, not just the disease.
The Science Behind Chemotherapy Fatigue
Chemotherapy fatigue is more than just a side effect. It’s a complex mix of changes in the body caused by treatment. These changes affect how we feel and function.
Damage to Healthy Red Blood Cells
Chemotherapy aims to kill fast-growing cancer cells. But it can harm healthy cells too, like red blood cells. Studies show that chemotherapy can damage these cells, reducing their count and how well they work.
Anemia and Reduced Oxygen Delivery
When red blood cells are damaged, anemia can occur. This is when the body doesn’t have enough red blood cells to carry oxygen. Anemia makes people feel tired because their bodies can’t produce energy well.
Inflammatory Responses in the Body
Chemotherapy can also start inflammation in the body. Inflammation can make us feel tired by messing with how cells work and energy production. The chemicals released during treatment can make exhaustion worse.
Knowing how chemotherapy fatigue works helps find ways to manage it. By tackling issues like anemia and inflammation, doctors can help patients feel better during and after treatment.
Why Does Chemo Make You Tired? The Biological Mechanisms
Chemotherapy-induced fatigue comes from many factors. It involves how cells, hormones, and the immune system react. When we get chemotherapy, it doesn’t just attack cancer cells. It also hits healthy cells, causing a chain of effects that make us tired.
Direct Effects of Chemotherapy Drugs on Cells
Chemotherapy drugs aim to kill fast-growing cancer cells. But they also harm other cells that grow quickly, like in the bone marrow, gut, and hair follicles. This can lower the number of red blood cells, which carry oxygen to our tissues.
With fewer red blood cells, our body can’t make as much energy. This makes us feel tired.
The damage to healthy cells is a big reason for chemotherapy-induced fatigue. Research shows that how tired we feel often matches how strong the chemotherapy is.
Hormone Regulation Disruption
Chemotherapy can mess with our hormones. For example, it can change how we make red blood cells. This can cause anemia, making us even more tired. It can also affect our energy levels by changing cortisol, a hormone that helps us feel awake.
“The hormonal changes induced by chemotherapy can have a profound impact on a patient’s energy levels.”
Immune System Response to Treatment
Our immune system is key in fighting off chemotherapy. The treatment can start an inflammatory response. This releases cytokines that can change how we use energy.
The complex relationship between our immune system and chemotherapy is a big area of study for treatment-related fatigue. By understanding these connections, doctors can find ways to reduce fatigue and help patients feel better.
Recognizing Cancer Fatigue Symptoms
It’s key to spot cancer fatigue signs early to manage it well and help patients feel better. This condition is complex and affects people differently, mainly those getting chemotherapy.
Physical Manifestations
People often feel very tired and can’t do everyday tasks. This is because chemotherapy affects the body and can cause anemia and less oxygen to tissues.
Other signs include persistent tiredness that doesn’t go away with rest, weaker muscles, and feeling generally unwell. These symptoms make it hard for patients to live their lives as they normally would.
Cognitive Effects
Cancer fatigue also messes with your mind, causing difficulty concentrating and memory issues. It’s hard to focus, make choices, or remember things. These brain problems can really lower a patient’s quality of life.
Why these brain effects happen isn’t fully known. But it’s believed that chemotherapy’s inflammation and the emotional stress of cancer play a role.
Sleep Pattern Disruptions
Disrupted sleep patterns are common in cancer fatigue. People might have trouble sleeping or sleep too much, making them feel even more tired. Sleep issues can come from the stress of treatment, side effects of meds, and changes in routine.
Fixing sleep problems is important for fighting cancer fatigue. Good sleep habits, like a regular sleep schedule and a comfy sleep space, can help.
The Timeline of Tiredness After Chemotherapy
Knowing when tiredness after chemotherapy happens is key for patients and doctors. Fatigue from chemo, or chemo fatigue, affects many people’s lives. Each person’s experience with fatigue is different, but there are common patterns.
Acute Fatigue During Treatment Cycles
Patients often feel very tired during chemo cycles. This tiredness comes from the chemo drugs affecting the body. Chemotherapy drugs harm both cancer cells and healthy cells, causing fatigue. How tired someone feels can depend on the chemo, its dose, and their health.
Persistent Fatigue Weeks After Treatment
Many patients stay tired long after chemo ends. This lasting tiredness can be hard because patients want to get back to normal. Studies show that cancer patients often stay tired for weeks or months after chemo.
Long-Term Recovery Patterns
Getting over chemo fatigue takes time. Some people start to feel better soon after chemo, but others take longer. How long it takes to recover depends on the chemo, the patient’s health, and any other health issues. Knowing this helps doctors give better support.
It’s important for patients and their families to know about the timeline of tiredness after chemo. Understanding what to expect helps them manage their energy better during and after treatment.
Factors That Intensify Chemo Exhaustion
It’s important to know what makes chemotherapy exhaustion worse. Fatigue from chemo is a big problem for many patients. Different things can make it even harder to deal with.
Treatment-Related Contributors
Many things about treatment can make chemo exhaustion worse. These include:
- How often and how intense the chemo sessions are
- The type of chemo drugs used
- When chemo is combined with other treatments like radiation
Studies have shown that more intense chemo can lead to more fatigue. For example, a study in the Journal of Clinical Oncology found that dose-dense chemo made patients feel more tired than standard chemo.
Secondary Factors
Other things can also make chemo exhaustion worse. These include:
| Secondary Factor | Impact on Fatigue |
|---|---|
| Poor nutrition and dehydration | Increases fatigue by reducing energy levels |
| Infections and comorbidities | Exacerbates fatigue by adding to the body’s stress |
| Sleep disturbances | Contributes to fatigue by disrupting rest and recovery |
As highlighted in a
“…the interplay between these secondary factors and chemotherapy-induced fatigue is complex, and addressing them is key for managing fatigue.”
Emotional Stress and Psychological Burden
Emotional stress and the psychological burden of chemo are big factors. The emotional impact of a cancer diagnosis and the stress of treatment can make fatigue worse.
Mindfulness and stress reduction techniques can help. A study in the Journal of Clinical Psychology found that mindfulness reduced fatigue and improved life quality for patients.
Understanding and tackling these factors can help healthcare providers better manage chemo-induced fatigue. This can improve patient outcomes and quality of life.
Medical Management of Chemotherapy and Tiredness
Managing chemotherapy and tiredness is key to better patient outcomes and quality of life. Chemotherapy-induced fatigue is common and complex. It requires a full approach, including medical treatment and lifestyle changes.
Treating Underlying Anemia
One major strategy for managing fatigue is treating anemia. Anemia happens when there are not enough red blood cells or when the red blood cells don’t carry enough oxygen. Chemotherapy can damage the bone marrow, where red blood cells are made.
To treat anemia, we use:
- Iron Supplements: To increase iron levels and help make more red blood cells.
- Erythropoiesis-Stimulating Agents (ESAs): Medications that help the bone marrow make more red blood cells.
- Blood Transfusions: Sometimes, blood transfusions are needed to quickly raise red blood cell counts.
Medications to Combat Fatigue
There are also medicines to fight fatigue. These include:
- Psychostimulants: Drugs like methylphenidate that boost alertness and energy.
- Antidepressants: Antidepressants might be used if depression is causing fatigue.
- Steroids: Short-term steroids can also help increase energy.
It’s important to talk to your healthcare provider to find the right medication for you. Everyone reacts differently to treatments.
When to Contact Your Healthcare Provider
If you’re feeling very tired from chemotherapy, know when to get help. It’s important to call your healthcare provider if you have:
- Severe Fatigue: If you’re too tired to do daily things.
- Shortness of Breath: If you’re out of breath even when sitting or doing light activities.
- Dizziness or Fainting: If you feel dizzy or faint, which can be a sign of severe anemia.
Understanding your options can help you deal with chemotherapy tiredness. This can improve your life during treatment.
Nutritional Strategies to Combat Cancer-Related Fatigue
The right food can really help with cancer-related fatigue. Eating well can ease symptoms, boost health, and aid in recovery during and after treatment.
Energy-Boosting Foods During Treatment
Choosing the right foods can increase energy. Foods rich in antioxidants like berries and leafy greens can fight off stress from treatment. Complex carbohydrates from whole grains and quinoa give lasting energy.
Iron-rich foods like lean meats and beans help fight anemia, a common fatigue cause. Nuts and seeds add healthy fats and protein.
Protein Intake for Muscle Preservation
Enough protein is key to keep muscles strong during treatment. Include lean protein sources like poultry and beans in every meal.
Studies show eating 1.2 to 1.5 grams of protein per kilogram of body weight daily helps keep muscles. Spread out protein intake for best results.
Hydration and Electrolyte Balance
Drinking enough water is critical for cancer patients to avoid dehydration. Drinking plenty of water and electrolyte-rich drinks like coconut water helps balance fluids.
Hydrating foods like watermelon and cucumbers also help with hydration. Check urine color and output to see if you’re drinking enough.
Working With Oncology Nutritionists
Oncology nutritionists offer personalized dietary advice for cancer patients. They create nutrition plans that meet specific needs and manage side effects.
Getting help from an oncology nutritionist can guide patients in making better food choices. This can help reduce fatigue and improve life quality.
“Nutrition plays a critical role in the management of cancer-related fatigue. A personalized nutrition plan can help patients maintain their strength and energy levels throughout treatment.”
Physical Activity: A Counterintuitive Approach to Chemo Fatigue
At first, it might seem like resting is the best thing to do when feeling tired from chemotherapy. But, gentle physical activity can actually help fight fatigue. It’s important to find a balance between rest and activity to avoid feeling even more tired.
Benefits of Gentle Movement
Studies show that gentle exercise can help cancer patients feel less tired. Regular physical activity can boost energy levels, improve sleep, and lower the risk of other health problems. Start with simple activities like short walks or light stretching.
Exercise also has mental benefits, like reducing stress and anxiety. Choose activities that you enjoy and that match your current energy levels.
Safe Exercise Options During Treatment
When exercising during chemotherapy, safety is key. Low-impact activities like yoga, tai chi, or swimming are good choices. These exercises help keep you flexible and strong without overexerting your body.
Always talk to your healthcare provider before starting any new exercise plan, even more so during treatment. They can tell you what exercises are safe and right for you.
Collaborating With Physical Therapists
Working with a physical therapist can be very helpful. They can create a workout plan that fits your health, energy, and treatment. Physical therapists can also guide you on how to safely increase your activity levels as you get better.
Team up with a physical therapist to make sure you’re doing exercises that are safe and effective for managing your symptoms.
Adapting Exercise to Energy Levels
It’s important to listen to your body and adjust your exercise routine as needed. On days when you have more energy, you can do more intense or longer workouts. But on days when you’re really tired, it’s okay to take it easy.
Respecting your body’s limits is key. This might mean taking breaks during exercise or doing less intense activities on really tired days.
Energy Conservation Techniques for Daily Living
Living with cancer-related tiredness requires a smart plan for daily tasks. We know that fighting fatigue is key to a good life during treatment.
Prioritizing Activities and Tasks
Learning to pick what’s most important is a big help. Make a list of daily tasks and sort them by how urgent and important they are. This way, you save energy for the most critical tasks.
For example, if you have a hospital visit in the morning, plan your day around it. Choosing what to do first helps use your energy better.
| Task | Priority Level | Energy Required |
|---|---|---|
| Hospital Appointment | High | High |
| Grocery Shopping | Medium | Medium |
| Social Gathering | Low | High |
Pacing Strategies Throughout the Day
Managing your energy means pacing yourself. Break big tasks into smaller ones and take breaks. This keeps you from getting too tired and helps you stay productive.
Instead of cleaning the whole house in one day, clean one room at a time. Take breaks in between. This way, tasks don’t feel so big.
Creating a Fatigue-Friendly Environment
It’s also important to make your living space rest-friendly. We suggest keeping things tidy, using comfy furniture, and making your home easy to move around in.
For more tips on dealing with cancer-related tiredness, check out our resource on the topic. It offers more ways to manage fatigue.
Psychological Approaches to Coping With Chemo and Exhaustion
Dealing with the emotional side of chemotherapy and exhaustion needs a mix of strategies. It’s key to tackle the mental health side of things. This affects how well a patient lives during treatment.
Mindfulness and Stress Reduction
Mindfulness helps lower stress and anxiety in cancer patients. Activities like meditation and deep breathing help patients stay in the moment. They can better handle the emotional ups and downs of treatment.
Mindfulness benefits:
- Reduces stress and anxiety
- Improves emotional regulation
- Enhances overall well-being
Cognitive Behavioral Techniques
Cognitive Behavioral Therapy (CBT) helps patients deal with chemotherapy’s mental effects. It helps them change negative thoughts into more positive ones. This way, they can cope better.
| CBT Techniques | Benefits |
|---|---|
| Cognitive restructuring | Reduces negative thinking |
| Exposure therapy | Helps manage anxiety |
| Problem-focused coping | Enhances problem-solving skills |
Support Groups and Counseling Options
Support groups and counseling offer a place to share and get support. They are a big help in fighting off the loneliness and stress of chemotherapy.
Benefits of support groups:
- Emotional support from peers
- Reduced feelings of isolation
- Improved coping strategies
Conclusion: Navigating the Journey Through Recovery
Recovering from chemotherapy fatigue needs a full and supportive plan. We’ve looked into the challenges of tiredness from chemo, its effects on patients, and ways to handle it.
Studies show that a mix of medical care and lifestyle support can help patients get better. Nutritional plans, exercise, saving energy, and mental health support can make a big difference.
Our institution knows how vital top-notch healthcare is, including for patients from abroad. We’re committed to guiding patients through their recovery. Our team offers personalized care to meet each patient’s needs.
With a caring and all-encompassing approach, patients can live better during and after treatment. This makes their recovery journey more successful.
FAQ
What is chemotherapy fatigue?
Chemotherapy fatigue is a side effect of cancer treatment. It makes you feel very tired, weak, and without energy. This makes it hard to do daily activities.
Why does chemotherapy cause fatigue?
Chemotherapy harms healthy red blood cells, causing anemia. It also triggers inflammation. This disrupts normal body functions and hormone regulation, leading to fatigue.
How long does chemotherapy fatigue last?
How long you feel tired from chemotherapy varies. It can last during treatment, weeks after, and sometimes for months or years after treatment ends.
What are the symptoms of cancer-related fatigue?
Symptoms include feeling weak and tired, having trouble concentrating, and sleep problems. This includes insomnia or sleeping too much.
How can I manage chemotherapy fatigue?
Managing fatigue involves several steps. This includes medical care, eating right, staying active, saving energy, and mental health support.
What nutritional strategies can help combat cancer-related fatigue?
Eating foods that give you energy, enough protein, staying hydrated, and balancing electrolytes can help. Getting advice from oncology nutritionists is also helpful.
Can exercise help with chemotherapy fatigue?
Yes, gentle exercises during treatment can help. They should match your energy level. Working with physical therapists ensures a safe plan.
How can I conserve energy during daily activities?
Focus on what’s important, pace yourself, and make your environment comfortable. This helps save energy and reduce fatigue.
What psychological approaches can help cope with chemo and exhaustion?
Mindfulness, stress reduction, and cognitive behavioral techniques help. Support groups and counseling also offer emotional support during chemotherapy and fatigue.
When should I contact my healthcare provider about chemotherapy fatigue?
Contact your healthcare provider if you’re very tired or if fatigue lasts a long time. Also, if you’re worried about managing your fatigue or other symptoms.