Sickle Cell Disease (SCD) is a genetic disorder that affects hemoglobin. This leads to vaso-occlusive crises and chronic pain. The problem is when misshapen red blood cells block blood vessels. This causes tissue ischemia and triggers intense pain episodes.
At Liv Hospital, we understand the complexities of SCD pain. We know how it affects patients’ daily lives. Why does sickle cell disease cause pain, Our goal is to provide evidence-based, multidisciplinary care. We aim to alleviate suffering and improve the quality of life.
Key Takeaways
- SCD is a genetic disorder causing abnormal hemoglobin production.
- Vaso-occlusive crises lead to tissue ischemia and pain.
- Understanding pain mechanisms is key for effective management.
- Liv Hospital offers top-notch, internationally competitive treatment.
- Multidisciplinary care is essential for better patient outcomes.
The Fundamentals of Sickle Cell Disease

To understand Sickle Cell Disease, we must look at its genetic roots and its worldwide effect. SCD is a genetic disorder caused by a mutation in the HBB gene. This mutation results in abnormal hemoglobin, known as sickle hemoglobin or HbS.
Genetic Basis and Inheritance Patterns
SCD is an autosomal recessive disorder. This means an individual must inherit two defective HBB genes to have the disease. Carriers, with one normal and one defective gene, usually don’t show all symptoms but can pass the mutated gene to their children. Knowing how SCD is inherited is key for genetic counseling and family planning.
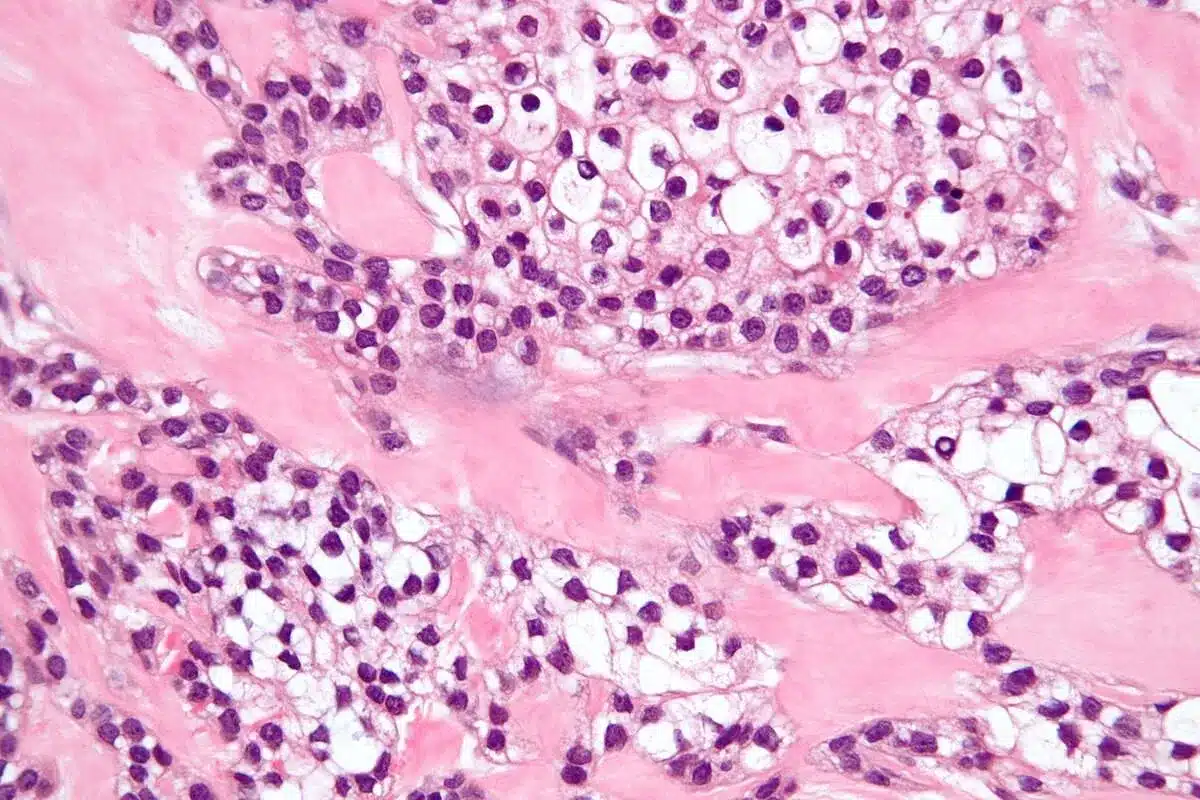
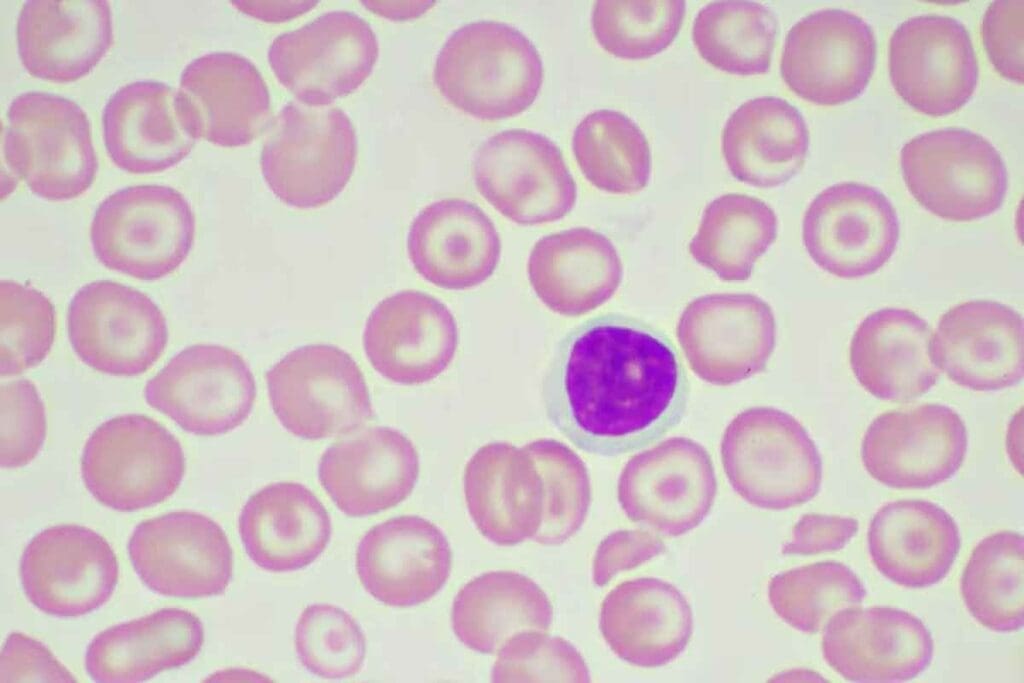
Abnormal Hemoglobin and Red Blood Cell Sickling
The abnormal hemoglobin (HbS) in SCD causes red blood cells to become sickle-shaped under low oxygen levels. This makes the cells rigid and prone to destruction, leading to anemia and other issues.
Global Prevalence and Demographics
SCD is more common in sub-Saharan Africa, the Mediterranean, and parts of India. It affects millions globally, putting a strain on healthcare systems in these areas. Knowing the global prevalence and demographics of SCD is vital for public health strategies.
The disease’s prevalence in certain groups shows the need for awareness and education. By grasping the genetic basis, inheritance patterns, and global impact of SCD, we can better meet the needs of those affected and their communities.
Why Does Sickle Cell Disease Cause Pain? The Basic Mechanisms
Pain in SCD is complex, mainly due to vaso-occlusive events and inflammatory responses. Knowing these mechanisms helps in finding better pain management.
Sickled Cells and Blood Flow Obstruction
In SCD, sickled red blood cells block small blood vessels. This is because of abnormal hemoglobin. It leads to vaso-occlusive crises.
Key factors contributing to blood flow obstruction include:
- Increased adhesion of sickled red blood cells to the endothelium
- Enhanced aggregation of sickled cells
- Activation of various cellular and molecular pathways that promote vaso-occlusion
Tissue Ischemia and Oxygen Deprivation
Blocked blood vessels cause tissue ischemia and oxygen deprivation. This leads to pain. Ischemia triggers a series of cellular responses.
The pain from tissue ischemia in SCD is sharp or stabbing. It can happen in the chest, abdomen, back, and limbs.
The Inflammatory Cascade
The inflammatory cascade is key in SCD pain. Tissue ischemia and damage release pro-inflammatory cytokines. These cytokines make inflammation worse and sensitize nociceptors.
The key components of the inflammatory cascade include:
- Release of pro-inflammatory cytokines
- Activation of various inflammatory cells, such as macrophages and T lymphocytes
- Production of prostaglandins and other inflammatory mediators that enhance pain transmission
Understanding the link between vaso-occlusive crises and inflammation is vital. It helps in creating effective pain management for SCD.
Vaso-Occlusive Crisis: The Primary Pain Generator
Vaso-occlusive crises are a key part of Sickle Cell Disease. They are the main way pain happens. These crises happen when sickled red blood cells block blood vessels. This causes tissue ischemia and pain.
Triggers and Precipitating Factors
Many things can start a vaso-occlusive crisis. Dehydration, infections, and stress are some of them. Dehydration makes the blood thicker, which increases the chance of blockages. Infections cause inflammation, which can also lead to blockages. Stress, both physical and emotional, can make things worse by increasing oxygen demand.
Knowing what triggers these crises is key to managing SCD. By understanding and reducing these triggers, patients and doctors can lessen the number and severity of crises.
Pathophysiology of Vascular Occlusion
The way vascular occlusion works in SCD is complex. It involves sickled red blood cells, the vascular endothelium, and inflammatory mediators. Sickled cells are less flexible and stickier, making them get trapped in the microvasculature and cause blockages.
| Factor | Role in Vaso-Occlusion |
| Sickled Red Blood Cells | Obstruct blood vessels due to their rigidity and adhesiveness |
| Inflammatory Mediators | Enhance the adhesion of sickled cells to the endothelium |
| Vascular Endothelium | Becomes activated, promoting adhesion and vaso-occlusion |
Reperfusion Injury and Pain Amplification
Reperfusion injury happens when blood flow returns to an ischemic area. It causes more tissue damage and pain. This injury involves the release of reactive oxygen species and inflammatory mediators, making tissue injury worse and increasing pain during crises.
Managing reperfusion injury is vital in treating vaso-occlusive crises. It’s important to reduce tissue damage and pain to improve patient outcomes.
The Neurobiological Basis of Sickle Cell Pain
Sickle cell pain is complex. It involves how our body’s pain sensors work. Knowing this helps us find better ways to manage pain.
Nociceptor Activation and Sensitization
Nociceptors are special sensors that feel pain. In sickle cell disease, these sensors get activated by inflammation. This sends pain signals to our brain.
Over time, these sensors can become more sensitive. This makes them react more easily to pain. This is why some people with sickle cell disease experience chronic pain.
Pain Signal Transmission
Pain signals in sickle cell disease travel from sensors to the brain. This journey is helped by certain chemicals in our bodies. These chemicals, like substance P and CGRP, play a big role in how we feel pain.
We will look into how these chemicals help send pain signals. This will help us understand SCD pain better.
Neurochemical Mediators in SCD Pain
Chemicals in our body are key in how we feel pain in sickle cell disease. Here’s a list of some important ones:
| Neurochemical Mediator | Role in SCD Pain |
| Substance P | Transmits pain signals, involved in neurogenic inflammation |
| Calcitonin Gene-Related Peptide (CGRP) | Modulates pain transmission, vasodilation |
| Prostaglandins | Enhances pain by sensitizing nociceptors |
Understanding sickle cell pain is key to finding new treatments. By studying how pain signals work, we can improve how we manage pain. This will help patients with sickle cell disease feel better.
Acute vs. Chronic Pain in Sickle Cell Disease
People with Sickle Cell Disease face two types of pain: acute and chronic. Each type has its own traits. Knowing these differences helps in finding better ways to manage pain.
Characteristics of Acute Pain Episodes
Acute pain in SCD starts suddenly and is very intense. It can be caused by dehydration, infections, or extreme weather. This pain is so severe that it needs quick medical help.
Key characteristics of acute pain episodes include:
- Sudden onset
- Severe pain intensity
- Often triggered by specific factors
- Typically requires immediate medical attention
The Transition to Chronic Pain
Switching from acute to chronic pain in SCD involves changes in how the body feels pain. This shift makes managing pain harder.
The factors contributing to the transition to chronic pain include:
- Repeated episodes of acute pain
- Inflammation and tissue damage
- Neuroplastic changes in pain processing pathways
Mixed Pain Syndromes
Mixed pain syndromes mix acute and chronic pain. To manage them, we need a plan that covers both types of pain.
Effective management strategies for mixed pain syndromes include:
- Pharmacological interventions tailored to the specific pain type
- Non-pharmacological strategies such as cognitive-behavioral therapy
- Lifestyle modifications to reduce pain triggers
Peripheral and Central Sensitization Mechanisms
SCD patients often face repeated pain episodes. This leads to changes in how they process pain. These changes happen through peripheral and central sensitization.
How Repeated Pain Episodes Change Pain Processing
When SCD patients experience pain again and again, their body’s pain sensors become more sensitive. This is because of chemicals released that make these sensors react more easily.
The central nervous system also gets more sensitive to pain. This makes the pain signal stronger. It’s a big reason why SCD patients often develop chronic pain.
Neuroplasticity and Pain Memory
The brain’s ability to change in response to injury or experience is key. Repeated pain episodes can change the brain’s pain centers. This creates a “pain memory.”
This painful memory makes patients more likely to feel pain again. Their nervous system is ready to respond strongly to stimuli.
Hyperalgesia and Allodynia in SCD
Hyperalgesia and allodynia are common in SCD patients. Hyperalgesia means feeling more pain from stimuli. Allodynia is feeling pain from things that don’t usually hurt.
These issues come from the body’s and brain’s sensitization to pain.
| Condition | Description | Mechanism |
| Hyperalgesia | Increased sensitivity to pain | Peripheral and central sensitization |
| Allodynia | Pain from non-painful stimuli | Central sensitization |
It’s important to understand these mechanisms for better pain management in SCD patients. By tackling both peripheral and central sensitization, healthcare providers can offer better care.
Neuropathic Pain Components in Sickle Cell Disease
Understanding neuropathic pain in SCD is key to managing pain. This type of pain comes from nerve damage. It’s a big part of the disease’s pain profile.
Nerve Damage from Ischemic Events
In SCD, ischemic events damage tissues and nerves. This damage messes up nerve function. It makes pain signals send without a clear reason.
Ischemic events in SCD block blood flow, causing tissue damage. This damage releases chemicals that make nerves more sensitive. This leads to neuropathic pain.
Clinical Presentation of Neuropathic Pain
The way neuropathic pain shows up in SCD can differ a lot. Common signs include:
- Burning or shooting pain
- Allodynia (pain from a stimulus that doesn’t usually hurt)
- Hyperalgesia (more pain from normal stimuli)
These symptoms can really hurt a patient’s quality of life. It’s very important to find and treat them well.
Diagnostic Challenges
Diagnosing neuropathic pain in SCD patients is hard. Pain is hard to measure and there are no clear signs. This makes it tough to know if someone has neuropathic pain.
Doctors use patient history and exams to try to figure it out. They use pain questionnaires and check for nerve damage. These tools help them understand the pain better.
| Diagnostic Tool | Description | Use in SCD |
| Pain Questionnaires | Standardized questionnaires to assess pain characteristics and severity. | Helps in understanding the pain experience. |
| Neurological Examination | Clinical assessment to identify neurological deficits. | Aids in diagnosing nerve damage. |
| Neuropathic Pain Scales | Specific scales designed to measure neuropathic pain. | Assesses the severity of neuropathic pain. |
Managing neuropathic pain in SCD needs a full plan. This plan should include medicines and other treatments.
Inflammatory Markers and Pain Signaling
Inflammatory markers are key in the pain pathway of Sickle Cell Disease. Sickled red blood cells cause inflammation. This leads to the release of cytokines and other inflammatory mediators. These substances contribute to the pain patients feel.
We will look at cytokines, prostaglandins, and leukotrienes. These are important in pain signaling. Knowing how they work can help manage SCD pain better.
Key Cytokines and Their Roles
Cytokines are small proteins that affect cell interactions. In SCD, certain cytokines are important in pain and inflammation.
- TNF-alpha: Tumor Necrosis Factor-alpha is a pro-inflammatory cytokine that promotes inflammation and is involved in pain signaling.
- IL-1beta: Interleukin-1 beta is another pro-inflammatory cytokine that contributes to the inflammatory cascade and pain in SCD.
- IL-6: Interleukin-6 is a cytokine with both pro-inflammatory and anti-inflammatory properties, influencing pain and inflammation.
These cytokines work with cells and pathways to increase pain. Studies show that high levels of these cytokines are linked to more pain in SCD patients.
| Cytokine | Role in SCD Pain |
| TNF-alpha | Promotes inflammation and pain signaling |
| IL-1beta | Contributes to the inflammatory cascade and pain |
| IL-6 | Influences pain and inflammation with dual properties |
Prostaglandins and Leukotrienes
Prostaglandins and leukotrienes are important in SCD pain. Prostaglandins are made at damaged or inflamed tissue sites. They make pain worse by making nociceptors more sensitive.
“Prostaglandins play a critical role in inflammation, making nociceptors more sensitive to pain.”
Leukotrienes are part of the inflammatory response. They help in the development of inflammatory diseases, including SCD.
Biomarkers of Pain Crisis
Finding biomarkers for SCD pain crisis is key for managing pain. Studies have looked at inflammatory markers and other biochemical signs.
Potential biomarkers include:
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Pro-inflammatory cytokines (e.g., TNF-alpha, IL-1beta)
These biomarkers can help spot patients at risk of pain episodes. This allows for early action.
Organ-Specific Pain Manifestations
Sickle Cell Disease (SCD) causes pain in different parts of the body. This includes bones, joints, the abdomen, and the chest. The pain comes from the disease’s complex effects, like vaso-occlusion, inflammation, and tissue damage.
Bone and Joint Pain
Bone and joint pain are common in SCD. This pain comes from vaso-occlusive crises that block blood flow and cause tissue damage. The pain can be very severe and may need hospital care.
Infarctions in the bone marrow release pro-inflammatory mediators. This makes the pain worse. Joint pain can also happen due to aseptic necrosis, where bone tissue dies because of lack of blood. Treatment includes medicines and physical therapy.
Abdominal Pain
Abdominal pain is a common issue for SCD patients. It can be caused by gallstones, biliary obstruction, or vaso-occlusive crises in the abdomen. The pain can be sudden or long-lasting and may include nausea and vomiting.
Managing abdominal pain in SCD requires finding the cause. Some cases are treated with hydration and pain relief. Others might need surgery, like for cholecystitis.
Chest Pain and Acute Chest Syndrome
Chest pain in SCD patients is a serious issue. It can be a sign of acute chest syndrome (ACS), a dangerous condition. ACS has symptoms like fever, respiratory issues, and chest pain, along with a new lung problem on X-rays.
ACS can be caused by infections, fat embolism, or lung infarction. Quick action is needed, including antibiotics, bronchodilators, and sometimes blood transfusions. It’s important to watch patients closely in the hospital because their condition can get worse fast.
Pain Management Approaches in Sickle Cell Disease
Managing pain in sickle cell disease requires a mix of medicines and non-medical methods. We’ll dive into these methods to see how they help in caring for patients.
Pharmacological Interventions
Medicines are key in fighting SCD pain. Here are some:
- Opioids: For really bad pain, opioids are vital in handling crises.
- NSAIDs: These drugs help with mild to moderate pain and work well with opioids.
- Other Medications: There are also other treatments like anticonvulsants or antidepressants for nerve pain.
It’s important to match medicines to each patient’s needs. This includes looking at how bad the pain is, their health history, and possible side effects.
Non-pharmacological Strategies
Non-medical ways are also important in managing SCD pain. Here are some:
- Cognitive-behavioral therapy (CBT): CBT helps patients change how they see and deal with pain.
- Relaxation Techniques: Deep breathing, meditation, and muscle relaxation can help reduce pain and stress.
- Physical Therapy: Gentle exercises and therapy can make moving easier and lessen pain.
These methods help patients take charge of their pain. This improves their life quality a lot.
Emerging Treatment Modalities
New research is bringing hope for SCD treatments. Here are some promising ones:
- Gene Therapy: It’s a possible cure that fixes the SCD genetic problem.
- Stem Cell Transplantation: This could cure SCD by replacing bad bone marrow with healthy cells.
- New Pharmacological Agents: Scientists are working on new drugs to better manage SCD pain or stop crises.
These new treatments offer hope for better pain control and maybe even a cure for SCD in the future.
Psychosocial Dimensions of Sickle Cell Pain
SCD pain deeply affects patients’ lives, impacting their mental state and social interactions. Living with SCD is complex, involving physical pain management and dealing with its psychosocial effects.
Impact on Quality of Life
SCD significantly changes a person’s life quality. Pain crises and complications limit daily activities, strain relationships, and affect well-being. Patients often find it hard to participate in social and fun activities, leading to feelings of isolation and frustration.
- Restrictions in daily activities due to pain and fatigue
- Difficulty maintaining employment or attending school
- Strained personal and professional relationships
The effects of SCD go beyond physical; they also touch on emotional and social challenges. Effective management of SCD pain must consider these multifaceted aspects to improve patient outcomes.
Psychological Comorbidities
People with SCD often face depression and anxiety. The disease’s chronic nature and unpredictable pain crises contribute to these mental health issues. It’s vital to address these comorbidities as part of overall care.
- Depression: Characterized by persistent sadness and loss of interest
- Anxiety: Manifests as excessive worry and fear about future pain crises
Recognizing and treating these psychological aspects can greatly improve SCD patients’ quality of life.
Social and Cultural Factors in Pain Experience
Social and cultural factors greatly influence how people experience and cope with SCD pain. Cultural beliefs and practices shape pain perception and expression. Social support networks offer emotional and practical help.
- Cultural beliefs about illness and pain
- Family and community support systems
- Access to healthcare services and cultural competency of providers
Understanding these factors is key to delivering culturally sensitive care that meets diverse patient needs.
Conclusion: The Complex Nature of Sickle Cell Pain
Sickle cell disease (SCD) pain is complex. It comes from vaso-occlusive crises, inflammation, and neuropathic pain. We’ve looked at how these factors cause pain in people with SCD.
Understanding SCD pain is key. Knowing about sickled cells, inflammation, and neuropathic pain helps doctors create better treatment plans. This knowledge is vital for improving patient outcomes and quality of life.
Managing SCD pain needs a team effort. This includes using medicines and other methods. As we learn more about SCD pain, we see the importance of a treatment plan made just for each patient.
By taking a whole-person approach to pain management, we can help those with SCD live better. This approach improves their overall well-being.
FAQ
What is sickle cell disease, and how does it cause pain?
Sickle cell disease is a genetic disorder that affects blood. It makes red blood cells misshapen. This blocks blood vessels, causing pain.
What are the triggers and precipitating factors of vaso-occlusive crises in sickle cell disease?
Dehydration, infection, and stress can trigger pain crises. These factors cause blood vessels to block, leading to pain.
How does the inflammatory cascade contribute to pain in sickle cell disease?
Tissue ischemia starts an inflammatory cascade. This makes pain worse by sensitizing nerves and releasing pain chemicals.
What is the role of nociceptors in sickle cell pain?
Nociceptors are key in sickle cell pain. They send pain signals and are affected by pain chemicals.
What is the difference between acute and chronic pain in sickle cell disease?
Acute pain comes on suddenly and is very severe. Chronic pain is ongoing and can be mixed with acute pain.
How do repeated pain episodes affect pain processing in sickle cell disease?
Repeated pain changes how pain is processed. It leads to chronic pain and affects how the brain handles pain.
What are the clinical presentations of neuropathic pain in sickle cell disease?
Neuropathic pain is unusual and can feel like burning or shooting. It’s caused by nerve damage from lack of blood flow.
How do inflammatory markers contribute to pain signaling in sickle cell disease?
Inflammatory markers like TNF-alpha and IL-1beta play a big role in pain. They help identify who is at risk of pain episodes.
What are the different types of organ-specific pain manifestations in sickle cell disease?
Pain can affect different organs. This includes bone and joint, abdominal, and chest pain. Acute chest syndrome is a serious condition.
What are the pharmacological and non-pharmacological strategies for managing pain in sickle cell disease?
Medications like opioids and NSAIDs help manage pain. Non-medical strategies include therapy and relaxation techniques. New treatments like gene therapy are being explored.
How does sickle cell disease pain affect quality of life?
Pain from sickle cell disease impacts daily life and well-being. It also leads to mental health issues like depression and anxiety.
What are the social and cultural factors that influence pain experience in sickle cell disease?
Cultural beliefs and support networks shape how pain is experienced. They play a big role in managing pain.
Reference
- National Center for Biotechnology Information (NCBI) Bookshelf