Last Updated on November 26, 2025 by Bilal Hasdemir

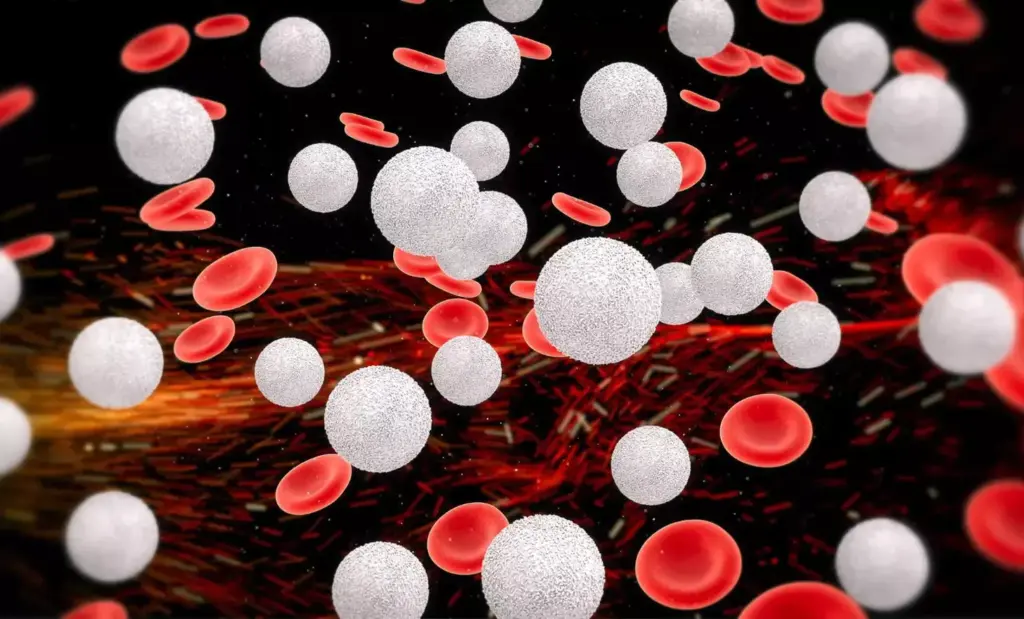
Chemotherapy is key in fighting cancer, but it can be delayed if white blood cell counts are low. This is called neutropenia. At Liv Hospital, we know how important it is to manage neutropenia. This helps prevent infections and keeps treatment on track.
Neutropenia makes infections more likely, which is why it’s so important to tackle it. Colony-stimulating factors are modern treatments that help increase white blood cells. Studies at the ESMO Congress show that managing neutropenia is essential during chemotherapy.
We focus on keeping our care up-to-date and centered on the patient. By understanding why chemo might be delayed and what can be done, patients can handle their treatment better.
Key Takeaways
- Chemotherapy delays due to low white blood cell counts are a common concern for cancer patients.
- Neutropenia increases the risk of infections, making it a critical condition to manage.
- Modern treatments, such as colony-stimulating factors, can boost white blood cell production.
- Liv Hospital emphasizes patient-centered care and up-to-date protocols to address neutropenia.
- Understanding the reasons behind chemotherapy delays can help patients navigate their treatment journey.
Understanding White Blood Cells and Their Role in the Body
At Liv Hospital, our team stresses the importance of knowing about white blood cells. We’ll look at the different types and their roles. We’ll also cover what counts are considered normal.
Types of White Blood Cells and Their Functions
There are many types of white blood cells, each with its own job. Together, they help our body fight off infections.
- Neutrophils: These cells are vital in fighting off bacterial infections. They are often the first to respond.
- Lymphocytes: Lymphocytes, including B cells and T cells, are important in specific immune responses. They help recognize and remember pathogens.
- Monocytes: Monocytes turn into macrophages. These cells clean up cellular debris and pathogens.
- Eosinophils: Eosinophils help fight parasitic infections and are involved in allergic reactions.
- Basophils: Basophils play a role in inflammation and allergic responses.
Normal White Blood Cell Count Ranges
Knowing the normal white blood cell count is key for diagnosing and managing conditions like neutropenia. The normal range is between 4,500 and 11,000 cells per microliter of blood. This range can vary slightly between labs.
| Type of White Blood Cell | Normal Range (cells/μL) | Percentage of Total WBCs |
|---|---|---|
| Neutrophils | 1,500 – 8,000 | 45-75% |
| Lymphocytes | 1,000 – 4,000 | 20-45% |
| Monocytes | 100 – 700 | 5-10% |
| Eosinophils | 50 – 500 | 1-4% |
| Basophils | <100 | <1% |
Checking white blood cell counts is very important for patients on chemotherapy. It helps us see the risk of infection and if we need to boost white blood cell production.
How Chemotherapy Affects Your Blood Cells

Chemotherapy impacts the body in many ways, affecting blood cells and sometimes causing neutropenia. It targets fast-growing cells, including cancer and some healthy cells like white blood cells. This can lower blood cell counts, causing neutropenia.
Chemotherapy’s Impact on Rapidly Dividing Cells
Chemotherapy aims to kill fast-growing cancer cells. But it also harms other fast-growing cells, like those making blood. White blood cells, key for fighting infections, are very vulnerable. This can weaken the immune system, making patients more likely to get sick.
The Timeline of Blood Cell Depletion After Treatment
The time it takes for blood cells to drop after chemotherapy varies. It depends on the treatment type and the patient. White blood cell counts often start falling a few days to a week after treatment.
It’s important to watch blood cell counts closely during this time. This helps catch any big drops early.
| Days After Chemotherapy | Expected White Blood Cell Count Change |
|---|---|
| 3-5 days | Initial drop in white blood cell count |
| 7-10 days | White blood cell count reaches its lowest point (nadir) |
| 14-21 days | Gradual recovery of white blood cell count |
Knowing how chemotherapy affects blood cells is key to managing side effects and avoiding treatment delays. At Liv Hospital, we keep a close eye on blood cell counts. This helps us act quickly and support our patients for the best results.
What is Neutropenia?
Neutropenia is a condition that affects people getting chemotherapy. It happens when there are not enough neutrophils, a key white blood cell, to fight off infections.
Definition and Diagnosis of Neutropenia
To find out if someone has neutropenia, a blood test is done. This test looks at the absolute neutrophil count (ANC). A normal ANC is between 1,500 and 8,000 cells per microliter.
ANC below 1,500 is considered neutropenic. The severity depends on how low the count is.
ANC between 1,000 and 1,500 is mild neutropenia. Counts below 500 are severe. Knowing these levels helps doctors decide what to do next.
Severity Levels and Clinical Implications
How severe neutropenia is affects the risk of getting infections. Those with severe neutropenia face a higher risk and might need more intense treatment.
| ANC Level | Severity | Clinical Implication |
|---|---|---|
| 1,500 – 8,000 | Normal | Low risk of infection |
| 1,000 – 1,499 | Mild | Moderate risk, monitor closely |
| 500 – 999 | Moderate | High risk, consider intervention |
| Below 500 | Severe | Very high risk, immediate action required |
At Liv Hospital, our team stresses the need for quick diagnosis and treatment of neutropenia. This helps avoid serious problems. Knowing the severity and what it means helps patients understand their treatment better.
Why Chemo Is Delayed Due to Low Blood Count
Chemotherapy delays because of low blood counts are key in cancer treatment. At Liv Hospital, we know how important timing is. Sometimes, we need to delay to keep patients safe.
Safety Concerns and Infection Risks
Low white blood cell counts, like neutropenia, raise infection risks. Chemotherapy affects fast-growing cells, including blood cells. This can lower white blood cell counts.
Neutropenia means not enough neutrophils, a key white blood cell. When neutrophil counts are low, fighting infections is harder. This makes chemotherapy risky.
Medical Protocols for Treatment Delays
Medical rules say chemotherapy should wait until blood counts are safe. At Liv Hospital, our team uses these rules to decide when to delay. We look at how severe the neutropenia is and the patient’s health.
The table below shows when to delay chemotherapy based on blood counts:
| Blood Count Level | Action | Recovery Time |
|---|---|---|
| Severe Neutropenia | Delay Chemotherapy | Until counts recover |
| Mild Neutropenia | Monitor Closely | Variable |
| Normal Counts | Proceed with Treatment | N/A |
Delaying chemotherapy until blood counts are good reduces infection risks. This ensures patients can handle treatment better. Our team helps manage treatment plans and supports patients during delays.
Statistics on Chemotherapy Delays and Their Impact
Chemotherapy delays because of low white blood cell counts happen often in cancer treatment. At Liv Hospital, we know how key it is to handle neutropenia. This helps avoid delays and ensures the best treatment results.
Research shows many patients face treatment breaks because of low white blood cell counts. These breaks can really affect how long treatment lasts and its success.
Frequency of Treatment Interruptions
Studies show treatment breaks happen more often than thought. Recent data shows a big number of patients with chemotherapy delays because of neutropenia.
| Study | Percentage of Patients with Delays | Average Delay Duration |
|---|---|---|
| Study A | 35% | 7-10 days |
| Study B | 42% | 10-14 days |
| Study C | 28% | 5-7 days |
The high number of treatment breaks shows we need better ways to manage delays. This ensures patients get their chemotherapy on time.
Effects on Overall Treatment Timeline and Outcomes
Chemotherapy delays can really affect how long treatment takes and its success. Delays can make treatment longer, hurting the patient’s quality of life. They can also make the treatment less effective.
Impact on Treatment Outcomes:
- Prolonged treatment periods
- Reduced treatment effectiveness
- Increased risk of complications
At Liv Hospital, we’re dedicated to top-notch care for patients facing chemotherapy delays. Our team works hard with patients to manage neutropenia. This helps reduce treatment breaks and ensures the best results.
Monitoring Your Blood Counts During Treatment
Keeping an eye on your blood counts during chemotherapy is key. At Liv Hospital, we stress the need for regular blood tests. These tests help us track your blood cell counts and guide your care.
Understanding Your Blood Test Results
Your blood test results give us important info about your blood cells. This includes white blood cells, red blood cells, and platelets. We work with you to understand these results and how they affect your treatment.
Understanding your blood test results is essential. It helps us manage side effects and adjust your treatment when needed.
For example, a low white blood cell count means you might be at higher risk for infections. We might change your chemotherapy schedule or add treatments to help your immune system.
Tracking Patterns and Recovery Times
By tracking your blood counts regularly, we can spot patterns and predict when your counts will recover. This info is critical for planning your treatment and avoiding delays. Tracking patterns and recovery times lets us customize your care for the best results.
For instance, if we see your white blood cell count drops a lot after each treatment, we can plan ahead. We might use medicines to boost your white blood cell count or adjust when you get your treatment.
Medical Interventions to Boost White Blood Cell Production
Modern treatments, like colony-stimulating factors, are key in raising white blood cell counts during chemotherapy. At Liv Hospital, our experts are skilled in using these treatments for patients going through chemotherapy.
Colony-Stimulating Factors: Types and Benefits
Colony-stimulating factors (CSFs) are drugs that boost white blood cell production, mainly neutrophils. These cells are vital for fighting off infections. There are two main types used in medicine: Granulocyte-CSF (G-CSF) and Granulocyte-Macrophage CSF (GM-CSF).
G-CSF, like filgrastim, is often used to prevent low white blood cell counts in chemotherapy patients. It encourages the bone marrow to make more neutrophils, lowering infection risk. GM-CSF, by contrast, boosts both neutrophils and macrophages, another white blood cell type, for better immune defense.
| Type of CSF | Function | Examples |
|---|---|---|
| G-CSF | Stimulates production of neutrophils | Filgrastim |
| GM-CSF | Stimulates production of neutrophils and macrophages | Sargramostim |
Other Medications and Treatments for Neutropenia
Other than CSFs, treatments for low white blood cell counts include antibiotics to prevent or treat infections. Adjustments to chemotherapy regimens may also be made to lessen its impact on white blood cell counts.
Key Considerations:
- Regularly checking blood counts to see if treatment is needed
- Using CSFs before neutropenia occurs in high-risk patients
- Changing chemotherapy doses or schedules as necessary
Healthcare providers use these treatments to reduce risks from low white blood cell counts. This ensures patients get the right care to manage their cancer effectively.
Nutritional Strategies to Support Your Immune System
Eating right is key to fighting off chemotherapy side effects. A diet full of essential nutrients can boost your immune system. This can lower the chance of getting sick. At Liv Hospital, our nutrition team helps create meal plans that fit your needs during treatment.
Immune-Boosting Foods and Nutrients
Some foods and nutrients are great for your immune system during chemo. These include:
- Vitamin C-rich foods: Citrus fruits, strawberries, and bell peppers are full of vitamin C. This vitamin is good for your immune system.
- Zinc-rich foods: Zinc helps your immune cells work right. Eat foods like oysters, beef, and chicken to get zinc.
- Antioxidant-rich foods: Foods like berries and leafy greens protect your cells from harm.
A study in the Journal of Clinical Oncology says, “Eating lots of fruits, veggies, and whole grains helps your immune system when you have cancer.”
“A balanced diet with lots of whole foods gives you the nutrients your immune system needs during chemo.”
Meal Planning and Preparation During Treatment
Planning your meals well is important during chemo. Here are some tips:
| Meal Planning Tips | Benefits |
|---|---|
| Include a variety of foods in your diet | Ensures you get a broad range of nutrients |
| Choose foods that are easy to digest | Reduces the risk of nausea and discomfort |
| Stay hydrated | Helps in the recovery process and reduces side effects |
Our nutrition experts at Liv Hospital suggest talking to a healthcare provider. They can help make a meal plan that’s right for you during chemo.
By eating foods that boost your immune system and planning your meals carefully, you can help keep your health strong during chemo.
Practical Steps to Reduce Infection Risk
Chemotherapy patients can lower their infection risk by taking simple steps. At Liv Hospital, we stress the need for proactive measures. These steps help patients protect themselves and improve their treatment outcomes.
Daily Hygiene and Environmental Precautions
Good hygiene is key to avoiding infections. Frequent handwashing with soap and water or hand sanitizer is essential. Do this after using the bathroom, before eating, and after coughing or sneezing.
It’s also important to keep your environment clean. Avoid close contact with sick people and stay away from crowded places. Keeping your living space clean is vital.
Social Distancing and Activity Modifications
Social distancing is a must to lower infection risk. Patients should limit contact with others, mainly when their white blood cell count is low. This means avoiding public gatherings and being careful about personal space.
Changing daily activities can also help. Try walking at home or doing light stretches instead of going to crowded gyms. Avoid activities that could cause injuries or infections, like contact sports or gardening.
“By taking these practical steps, patients can significantly reduce their risk of infections and create a safer environment for their recovery.”
Combining good hygiene, environmental precautions, and social distancing can greatly reduce infection risk. At Liv Hospital, we support our patients every step of the way. We provide the guidance and care they need to overcome these challenges.
Communicating Effectively With Your Healthcare Team
Talking well with your healthcare team can really change your treatment experience. It’s key to manage neutropenia and avoid delays in treatment. This is very important when you’re getting chemotherapy.
At Liv Hospital, we stress the need for a good team effort between patients and doctors. Open and honest talk helps patients get the best care and support during their treatment.
Questions to Ask About Blood Count Management
Asking the right questions is important for understanding your treatment. Here are some key questions to ask about managing blood counts:
- What are my current blood count levels, and what do they mean for my treatment?
- How will my chemotherapy regimen impact my blood cell counts?
- What are the signs and symptoms of neutropenia that I should be aware of?
- Are there any medications or interventions that can help boost my white blood cell count?
- How will treatment delays due to low blood counts affect my overall treatment timeline?
By asking these questions, patients can better understand their condition and the steps to manage it.
Advocating for Yourself During Treatment Delays
It’s important to speak up for yourself during treatment delays. Patients should express their concerns and ask questions about their care. Here are some tips for self-advocacy:
| Strategy | Description |
|---|---|
| Bring a support person | Having a family member or friend with you at appointments can offer emotional support and help you remember important details. |
| Keep a treatment journal | Writing down your treatment experience, including side effects and concerns, can help you track patterns and talk better with your healthcare team. |
| Ask for clarification | Don’t be shy to ask for explanations of medical terms or treatment plans. Understanding your care is key for making informed decisions. |
Effective communication is a two-way street. By working together with your healthcare team and advocating for yourself, you can overcome the challenges of chemotherapy and achieve the best outcomes.
Advanced Treatment Protocols at Specialized Cancer Centers
At places like Liv Hospital, we focus on advanced treatment protocols for those getting chemotherapy. These centers lead in cancer care, using new research and tech to help patients.
We tackle chemotherapy side effects in many ways, using innovative strategies for each patient. We keep up with new research and guidelines to give our patients the best and safest treatments.
Innovative Approaches to Managing Chemotherapy Side Effects
Managing neutropenia, a common side effect, is a big focus. We use colony-stimulating factors and other meds to help white blood cells grow. This helps prevent delays and lowers the risk of infections.
Our team checks blood counts often and changes treatment plans if needed. This way, we reduce neutropenia’s impact and let patients keep up with their treatments.
International Standards in Neutropenia Management
At Liv Hospital, we follow international standards in neutropenia management. This ensures our patients get top-notch care that meets global standards. Our treatment plans aim to improve patient outcomes and quality of life.
We use the latest research and guidelines to offer personalized care. Our goal is to manage side effects and support our patients’ overall well-being.
Conclusion: Navigating Chemotherapy Delays with Confidence
Managing neutropenia well is key to avoiding treatment delays. It helps ensure the best results. Patients can feel more confident by understanding why delays happen and what can be done.
At Liv Hospital, we focus on quality care and support for our patients. We aim to help them manage neutropenia and avoid delays. This way, they can face their treatment with hope and confidence.
Handling chemotherapy delays needs a full plan. This includes medical help, good nutrition, and steps to avoid infections. Working with their healthcare team, patients can create a plan to manage neutropenia. This keeps them confident and strong during treatment.
FAQ
What is neutropenia, and how is it diagnosed?
Neutropenia is when you have too few neutrophils, a key white blood cell. Doctors use blood tests to check your absolute neutrophil count (ANC).
Why is chemotherapy delayed due to low white blood cell count?
Chemotherapy is delayed because low white blood cells increase infection risk. Treatment waits until blood counts are safe again.
How can I boost my white blood cell count during chemotherapy?
We use colony-stimulating factors (CSFs) to boost white blood cell production. Eating a balanced diet also helps support your immune system.
What are the practical steps to reduce the risk of infections during chemotherapy?
Daily hygiene, environmental precautions, and social distancing help fight infections. We teach these steps to keep you safe.
How are blood counts monitored during chemotherapy?
Regular blood tests track your blood cell counts. This info helps doctors monitor your health and recovery.
What are the effects of chemotherapy delays on overall treatment outcomes?
Delays can affect treatment time and success. Managing neutropenia well is key to avoiding delays and improving outcomes.
How can I communicate effectively with my healthcare team during treatment delays?
Ask questions about managing your blood counts and treatment options. Open communication ensures you get the best care.
What are colony-stimulating factors, and how do they help?
Colony-stimulating factors (CSFs) boost white blood cell production. They help fight infections and are vital in managing neutropenia.
How can nutrition support my immune system during chemotherapy?
Eating a balanced diet with essential nutrients strengthens your immune system. Our nutrition experts create personalized meal plans for you.
What are the benefits of receiving treatment at a specialized cancer center?
Specialized centers like Liv Hospital offer advanced treatments and innovative care. We follow international standards to ensure top-quality care for you.





