Last Updated on November 20, 2025 by Ugurkan Demir
Ever wondered why your blood seems thinner than normal or noticed unexplained bruising or bleeding? It’s important to know the causes and risks for your health.Understand why is my blood so thin and key causes, symptoms, and health risks.
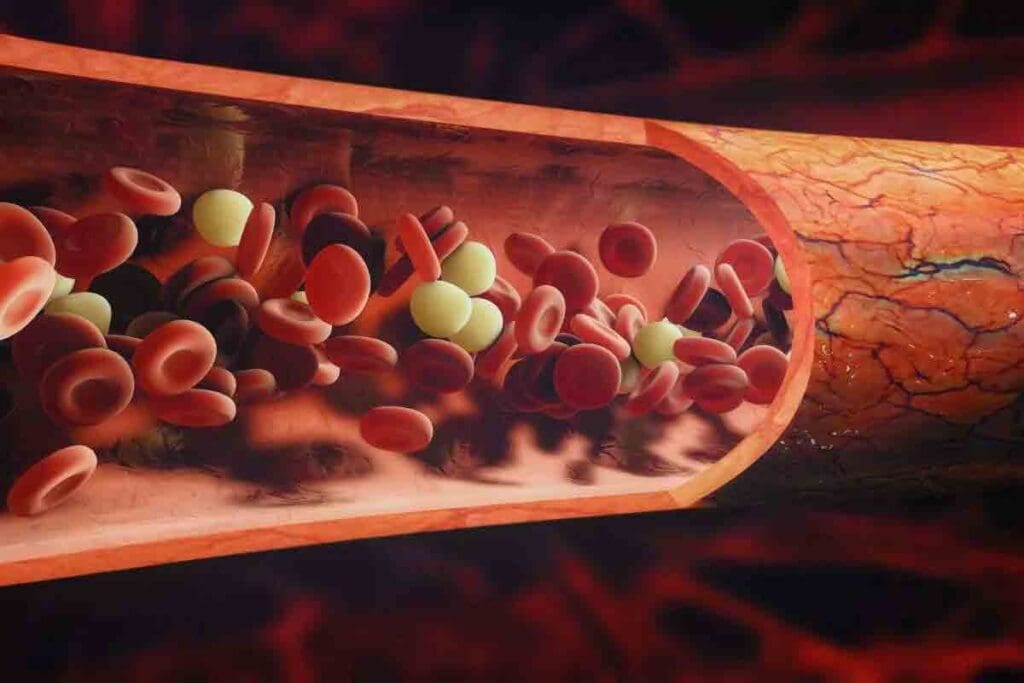
Thin blood, or thrombocytopenia, means your blood has fewer platelets. This makes it harder for your blood to clot and can lead to more bleeding or bruising. Liv Hospital’s commitment to international standards and patient-first care ensures you get the best treatment.
With fewer platelets, your body can’t clot blood as well. This makes stopping bleeding hard. You might get nosebleeds, bruise easily, and bleed longer after injuries.

The term ‘thin blood’ often refers to thrombocytopenia. This condition means you have too few platelets in your blood. Platelets are key for blood to clot, and not enough can cause health problems.
Thrombocytopenia is when you have less than 150,000 platelets per microliter of blood. Normal counts are between 150,000 and 450,000. If your count is too low, you might bleed more easily.
“A low platelet count can come from many things, like some medicines, diseases, or genes,” says a hematologist. “Knowing why it happens helps us treat it better.”
It’s important to know the difference between normal and low platelet counts. Normal counts are 150,000 to 450,000 platelets per microliter. Counts under 150,000 are low and can cause easy bruising and bleeding that lasts longer.
It’s important to know the difference between ‘thin blood’ and ‘watery blood.’ Thin blood means you have too few platelets, or thrombocytopenia. Watery blood, on the other hand, means you have fewer red blood cells. Both affect your blood but in different ways.
Key differences:
Knowing these differences helps with the right diagnosis and treatment. If you think your blood is too thin, see a doctor to get the right care.

Thin blood, or thrombocytopenia, can come from many sources. This includes some medicines, health issues, and genes. Knowing why your blood is thin is key to getting the right medical help.
Some medicines can change how thick your blood is. Anticoagulants and antiplatelet drugs are used to stop blood clots. But, they can sometimes cause your platelet count to drop.
It’s important to keep an eye on your platelet count while taking these medicines.
Different diseases can make your blood thinner. They can harm the bone marrow or make your body attack platelets.
| Disease | Effect on Blood |
| HIV/AIDS | Directly infects megakaryocytes, the cells that make platelets. |
| Hepatitis C | Causes thrombocytopenia through immune attacks and bone marrow issues. |
| Bone Marrow Disorders | Leukemia or aplastic anemia can directly affect platelet production. |
Some people are born with conditions that affect their platelet count. These genetic disorders can increase the risk of bleeding problems.
Examples include:
It’s important to know the signs of thinning blood to avoid serious health problems. Blood that’s too thin can cause a range of issues, from mild to severe. Being aware of these symptoms helps manage the condition better.
Easy bruising is a common sign of thin blood. When your blood can’t clot right, you might get bruises without any reason. Also, bleeding that lasts longer than usual is a symptom. This happens because your blood can’t stop bleeding as it should.
Frequent nosebleeds and bleeding gums are also signs of thin blood. These happen because your blood can’t clot right, causing bleeding in your nose and gums. While some bleeding is normal, too much might mean your blood is too thin.
Women with thin blood might have very heavy periods. This can cause a lot of bleeding during menstruation, leading to discomfort and possibly anemia. If your bleeding is much heavier than usual or you see big clots, it could be a sign of thin blood.
There are other signs that might mean your blood is too thin. These include:
Knowing these symptoms can help spot thin blood early. If you notice any of these signs, seeing a healthcare professional is key for diagnosis and treatment.
| Symptom | Description |
| Easy Bruising | Bruises appear without apparent reason due to poor clotting. |
| Prolonged Bleeding | Bleeding from cuts or injuries takes longer to stop. |
| Frequent Nosebleeds | Nosebleeds occur frequently due to poor clotting. |
| Heavy Menstrual Periods | Excessive bleeding during menstruation, potentially leading to anemia. |
Thin blood, or thrombocytopenia, can be caused by many medical conditions. It’s important to understand these conditions to diagnose and treat thin blood effectively.
Viral infections like HIV and hepatitis C can harm the body’s platelet production. This is because these viruses affect the bone marrow, where platelets are made.
HIV directly infects the megakaryocytes in the bone marrow, which are key to platelet production. Heatitis C can also cause thin blood through autoimmune reactions and bone marrow suppression.
Bone marrow disorders are a major cause of thin blood. Leukemia, lymphoma, and aplastic anemia can all disrupt the bone marrow’s ability to produce blood cells, including platelets.
Autoimmune diseases happen when the body attacks its own tissues. Some autoimmune diseases can cause thin blood.
Immune thrombocytopenic purpura (ITP) is when the immune system attacks platelets, leading to low counts and increased bleeding risk.
Chronic liver disease can also lead to thin blood. The liver is key in making clotting factors. Liver problems can lower these factors, raising the risk of bleeding.
Liver diseases like cirrhosis can cause hypersplenism. This is when the spleen removes too many platelets, lowering their count in the blood.
| Medical Condition | Effect on Blood |
| Viral Infections (HIV, Hepatitis C) | Affects platelet production |
| Bone Marrow Disorders (Leukemia, Lymphoma) | Impairs blood cell production |
| Autoimmune Diseases (ITP) | Destroys platelets |
| Chronic Liver Disease | Reduces clotting factors |
Medications that thin the blood are both helpful and risky. They protect against clots but can also make the blood too thin. It’s important to watch them closely to avoid problems.
Anticoagulants stop blood clots from forming or growing. They’re for people with DVT, pulmonary embolism, or stroke risk. Drugs like warfarin, apixaban, and rivaroxaban are common. But, they can make blood too thin, raising bleeding risks.
Antiplatelet drugs stop platelets from clumping. Aspirin and clopidogrel are used to prevent heart attacks and strokes. But, they can also make blood thinner, leading to easy bruising and longer bleeding times.
Some OTC drugs and supplements can thin the blood without you knowing. High doses of aspirin or ibuprofen can affect clotting. Herbal supplements like ginkgo biloba and fish oil also thin the blood. Always check with your doctor before taking these with prescription blood thinners.
Too thin blood from medication can be serious, even life-threatening. Signs include frequent nosebleeds, bleeding gums, and heavy periods. If you’re on blood thinners, watch for these signs and talk to your doctor if you notice them.
Nutritional deficiencies can affect blood clotting. They involve many vitamins and minerals important for blood health. These deficiencies can lead to conditions like thrombocytopenia.
Vitamin K is key for blood clotting. It helps make proteins needed for clotting. Without enough vitamin K, easy bruising and bleeding can happen. Foods like spinach, kale, and sauerkraut are good sources.
Iron is vital for healthy blood. It helps prevent anemia and supports blood health. Iron deficiency can cause fatigue and make infections more likely. It can also affect blood clotting indirectly.
Other nutrients are important for blood clotting and health. These include:
Eating a balanced diet is key for healthy blood. It helps prevent thin blood.
In summary, nutritional deficiencies play a big role in thin blood. Knowing about vitamins like vitamin K and minerals like iron helps. People can prevent or manage thin blood by eating right and, if needed, taking supplements.
Thin blood and blood pressure are connected in many ways. Lifestyle and health issues play a big role. People with high blood pressure might take medicine to keep it in check. But, some blood pressure medicines can also change how thick the blood is.
Some blood pressure medicines can make the blood thinner. For example, certain beta-blockers and diuretics can affect how blood clots. But their main job is to lower blood pressure.
Key Medications and Their Effects:
| Medication Type | Effect on Blood Thickness |
| Anticoagulants | Directly thin blood by inhibiting clotting factors |
| Antiplatelet Agents | Prevent platelets from aggregating, which thins the blood |
| Certain Beta-Blockers | May have an indirect effect by reducing blood pressure, potentially influencing clotting |
Dealing with thin blood and high blood pressure at the same time needs a careful plan. Doctors have to find the right balance. They need to control blood pressure without making the blood too thin.
Monitoring and Adjustments: It’s important to keep an eye on both blood pressure and blood thickness. Doctors might need to change the medicine to keep things right.
People with thin blood and high blood pressure should watch for signs of bleeding or bruising. They should also keep an eye on their blood pressure. Regular blood tests are key.
It’s important to understand how thin blood and blood pressure work together. By watching closely and making changes as needed, doctors can help patients manage these conditions.
Thin blood, or thrombocytopenia, is a serious health issue. It can lead to internal bleeding. When blood is too thin, it can’t clot well, causing problems.
One big danger of thin blood is internal bleeding. This is when blood bleeds inside the body. It’s very dangerous and needs quick treatment.
Common sites for internal bleeding include:
People with thin blood face more risks during surgery. The chance of too much bleeding is a big worry. It’s key to keep the patient safe.
| Surgical Complication | Description | Management Strategy |
| Excessive Bleeding | Bleeding that is difficult to control during or after surgery | Use of clotting agents, careful monitoring |
| Hematoma Formation | Collection of blood outside blood vessels | Drainage, compression |
In severe cases, thin blood can be very dangerous. This happens when there’s a lot of internal bleeding. Or when the body can’t stop the bleeding on its own.
Signs that thin blood has become life-threatening include:
Not all thin blood cases are the same. The danger level depends on the cause, how thin the blood is, and the person’s health.
Understanding the risks of thin blood is key. It helps people take steps to stay safe.
It’s important to know about diagnosis and treatment options for thin blood. Finding out what causes thin blood is key. This helps pick the right treatment.
A Complete Blood Count (CBC) test is often the first step. It checks the blood’s parts, like platelets and red blood cells. Low platelets can mean thin blood.
More tests might be needed to find thin blood’s cause. These include:
Treatment for thin blood varies based on the cause and how severe it is. Options include:
Medical treatments aren’t the only way to manage thin blood. Making lifestyle changes can also help. These include:
Understanding diagnosis and treatment options for thin blood helps manage it. This can lower the risk of serious problems.
It’s important to know what causes and shows thin blood. This knowledge helps people manage the condition and avoid problems. To live well with thin blood, one needs to see a doctor and make lifestyle changes.
Managing thin blood means keeping an eye on your meds and treating any health issues. You might also need to change your diet. For example, avoid foods rich in vitamin K, as they can make thin blood worse.
Preventing thin blood problems involves regular doctor visits. These check-ups help keep an eye on your blood’s thickness and adjust your treatment if needed. Taking these steps can lower your risk of complications and improve your life quality.
Knowing the risks of thin blood and managing it well can help you stay healthy and active. Proper management of thin blood is essential to avoid related issues and maintain good health.
Thin blood, or thrombocytopenia, means your blood has fewer platelets. This makes it harder for your blood to clot. It also raises your risk of bleeding.
Blood platelet counts should be between 150,000 to 450,000 per microliter of blood. This is the normal range.
Signs of thin blood include easy bruising and prolonged bleeding. You might also get frequent nosebleeds, heavy periods, and bleeding gums.
Thin blood can come from many sources. This includes some medicines, diseases like HIV and hepatitis C, and bone marrow issues. Autoimmune diseases and chronic liver disease can also cause it.
Yes, not getting enough vitamin K or iron can lead to thin blood. This is because they help with blood clotting.
Anticoagulant medicines stop blood clots from forming. This makes your blood thinner and increases the risk of bleeding.
Thin blood can be serious, but the danger level varies. It depends on the cause and how severe it is. Sometimes, it’s not life-threatening but needs medical care.
Doctors use a Complete Blood Count (CBC) test to find thin blood. This test checks the platelet count. They might also do other tests.
Treatments for thin blood include medicines to boost platelet count. You might also need to make lifestyle changes to manage bleeding risks.
Yes, managing both thin blood and high blood pressure is possible. It requires careful monitoring and treatment to reduce risks.
Very thin blood can lead to serious issues. These include internal bleeding, complications during surgery, and life-threatening situations.
To avoid thin blood, manage any health conditions you have. Stay away from certain medicines. Also, eat a balanced diet rich in vitamin K and iron.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!