Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, millions of people get life-saving blood transfusions. These transfusions are key in modern healthcare. They help treat many conditions, like blood loss, anemia, and cancer treatments. Listing the primary medical reasons and critical indications for Why would someone need a blood transfusion (e.g., severe anemia, acute blood loss).
A blood transfusion moves blood or blood parts from a donor to a patient. It aims to replace or add blood components. This is because disease or treatment can lower or mess up these components.
Key Takeaways
- Blood transfusions treat various medical conditions, including cancer and anemia.
- Chemotherapy patients may require blood transfusions due to low blood cell counts.
- Blood transfusions can significantly impact treatment outcomes and quality of life.
- Understanding the reasons behind blood transfusions is important for patients.
- Blood transfusions involve transferring blood or blood components from a donor.
Understanding Blood Transfusions
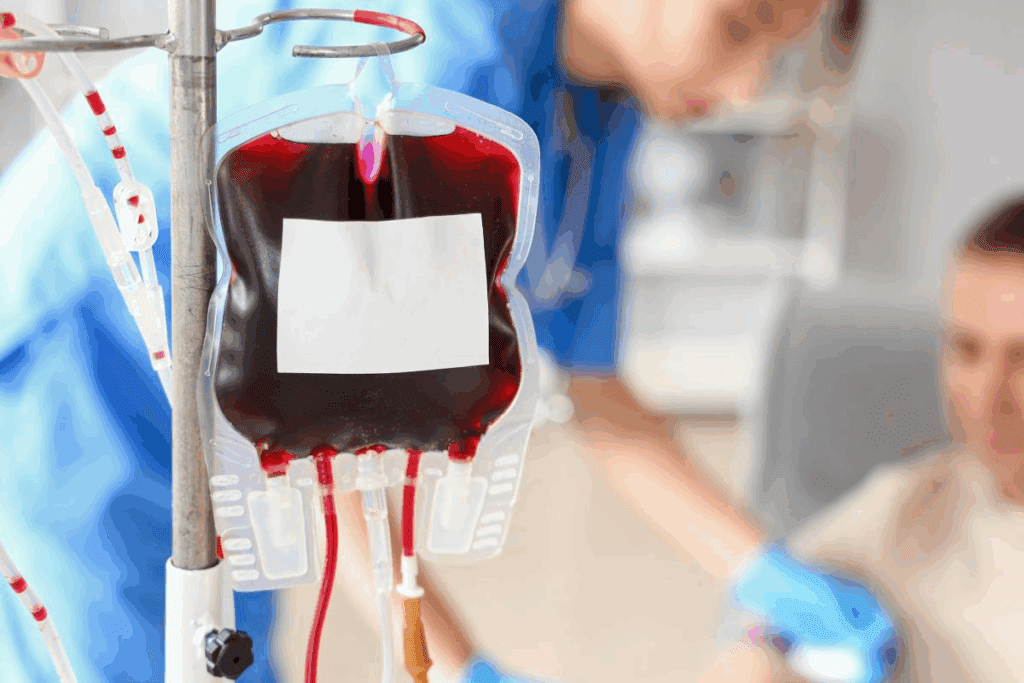
A Page blood transfusion is a procedure that involves transferring blood or blood components into a patient’s bloodstream. It helps patients recover from surgeries, manage chronic conditions, or overcome diseases that affect their blood.
What is a Blood Transfusion?
A blood transfusion is a medical procedure where we transfer blood or its components into a patient’s bloodstream. It’s important for replacing or supplementing specific blood components that may be depleted or dysfunctional. There are several types of blood transfusions, each designed to address specific medical Page needs.
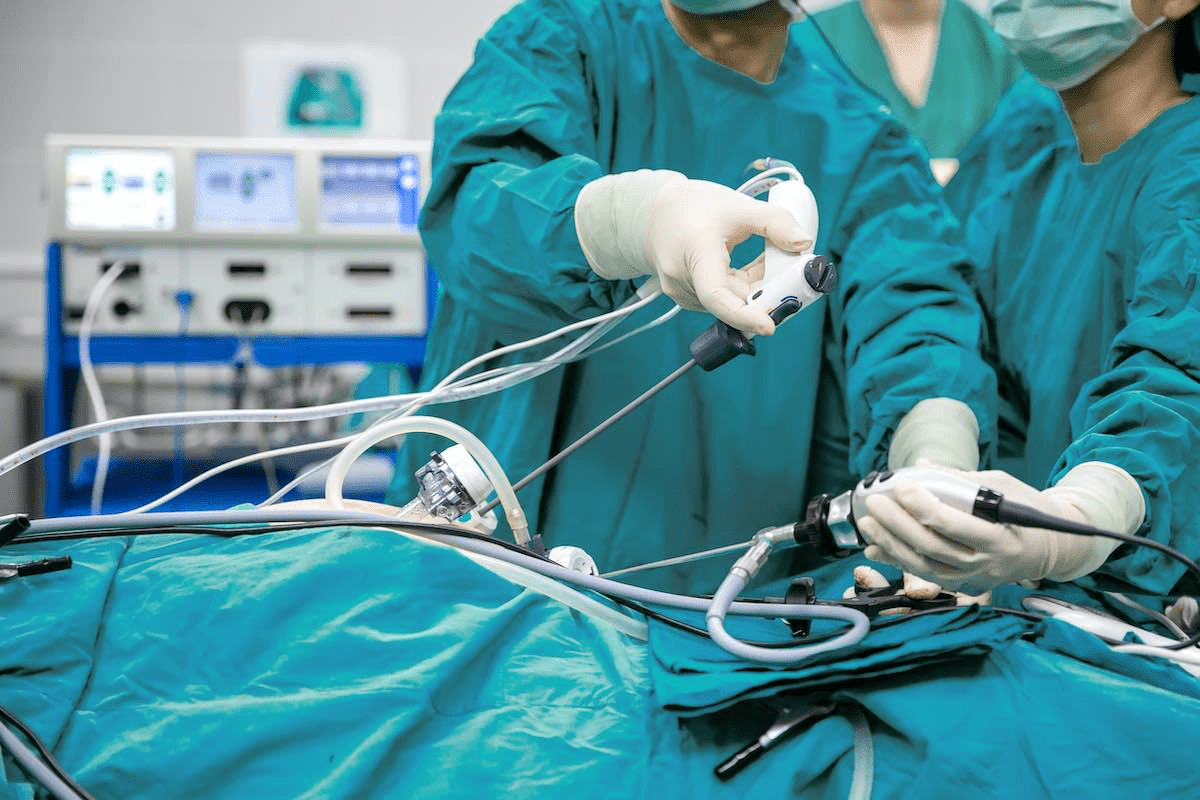
How Blood Transfusions Work
The process of a blood transfusion involves several steps, including blood typing Page, cross-matching, and the actual transfusion. We carry out these steps with great care to ensure the recipient’s safety. Blood typing determines the patient’s blood group, while cross-matching checks for compatibility between the donor’s and the recipient’s blood. Once compatibility is confirmed, the transfusion can proceed, typically in a controlled medical environment.
Understanding how blood transfusions work is essential for patients undergoing cancer treatment. It helps them better navigate their treatment options and manage complications. We are committed to providing complete care and support throughout this process.
- Red Page Blood Page Cell Transfusions: Used to treat coordinations or anemia.
- Platelet Transfusions: Help prevent or treat bleeding in patients with low platelet counts.
- Plasma Transfusions: Assist in managing bleeding disorders or conditions that affect clotting factors.
Reasons for Blood Transfusions in Chemo Patients
Chemotherapy patients often need blood transfusions. This is because chemo affects blood production and health. It’s a strong cancer fighter but comes with side effects that require blood transfusions.
Chemotherapy Side Effects
Chemotherapy targets fast-growing cells, including cancer and blood-making cells. This can cause bone marrow suppression and low blood cell counts. We’ll see how these effects lead to the need for blood transfusions.
Chemotherapy’s side effects vary and can be severe. Some patients get severe anemia, needing transfusions to boost oxygen delivery.
Blood Production Impairment
Chemotherapy can weaken the bone marrow, affecting blood cell production. This leads to anemia, neutropenia, and thrombocytopenia. Anemia is common and can greatly impact a patient’s life and treatment success.
With suppressed bone marrow, red and white blood cells, and platelets are made less. This causes fatigue, infection risks, and bleeding issues. Blood transfusions help manage these problems.
Managing Anemia
Anemia is common in chemo patients, caused by low red blood cells or hemoglobin. It’s key to manage anemia to improve health, reduce fatigue, and better treatment results. Blood transfusions help by increasing red blood cells and improving oxygen delivery.
We focus on managing anemia and other chemo side effects for the best patient outcomes. Understanding the need for blood transfusions helps us support patients through their treatment.
Signs That a Transfusion May Be Necessary
It’s important to know when a blood transfusion is needed. We watch patients closely who are getting chemotherapy. This is because their treatment can cause problems.
Symptoms of Low Blood Count
A low blood count, or anemia, shows in many ways. You might feel very tired, weak, or have pale skin. You could also breathe short, feel dizzy, or have a rapid heart rate.
Other signs include dark-colored urine and feeling really sick. If you see these, tell your doctor right away.
When to Seek Medical Advice
If you’re feeling any of these symptoms, get medical help. Call your doctor if your condition changes or gets worse.
For severe anemia or other serious issues, a blood transfusion might be needed. We want to help you get better. Our team is ready to answer your questions and concerns.
Types of Blood Components Used in Transfusions
Transfusion medicine uses different blood components to treat health issues. Blood has several key parts, each with its own role. These roles are vital for patient care.
Red Blood Cells
Red Blood Cells (RBCs) are key in transfusions. They carry oxygen from the lungs to the body’s tissues. We give RBC transfusions to patients with low oxygen levels or anemia.
Importance of RBC Transfusions: RBC transfusions boost the blood’s oxygen-carrying ability. This helps tissues get the oxygen they need, supporting the body’s functions.
Platelets
Platelets are vital for blood clotting. We give them to patients with low platelet counts or clotting issues. This is common in those undergoing chemotherapy or with bleeding disorders.
Role in Preventing Bleeding: Platelet transfusions help prevent bleeding in at-risk patients. This improves their prognosis and quality of life.
Plasma and its Role
Plasma is the liquid part of blood used in transfusions. It has proteins and clotting factors essential for patients with clotting disorders or significant blood loss. Plasma transfusions help restore these vital proteins.
Clinical Significance: Plasma transfusions are used in surgeries and emergency medicine. They help manage bleeding and aid in patient recovery.
Transfusions of blood components are key in modern medicine. They help treat many medical conditions. Understanding the different blood components and their uses helps us better care for patients needing transfusions.
The Blood Donation Process
Learning about the blood donation process can make people feel more comfortable about giving. It’s key to keeping a steady blood supply for those who need it.
How Blood is Collected
The blood collection process is detailed and safe. We use Page sterile equipment to keep the blood clean. It starts with registration and a health check to make sure the donor is okay.
- A healthcare professional will then clean the area where the needle will be inserted.
- The donation process itself usually takes around 10-15 minutes.
- After the donation, donors are monitored for a short period to ensure they are feeling era Page Page well.
Safety Measures for Donors
Keeping our donors safe is our main priority. We follow strict rules to protect both donors and those who receive the blood. Don Page or screening includes tests for diseases. We also give donors tips on what to do after donating to avoid any bad reactions.
Some of the safety measures include:
- Using sterile and disposable equipment for each donation.
- Conducting thorough health screenings before Page the donation.
- Monitoring donors during and after the donation process.
By knowing and following these steps, we make sure blood donations are safe and effective. We urge those who can to donate blood. It’s a kind act that can greatly help patients in need.
Pre-Transfusion Testing and Compatibility
Pre-transfusion testing is key to making blood transfusions safe and effective. We know how important it is to prevent bad reactions and keep patients safe.
The main goal is to check if the blood is compatible. This means looking at the blood type and other factors to avoid bad reactions. Making sure the blood is compatible is a big deal for patient safety.
Importance of Blood Typing
Blood typing is a big part of pre-transfusion testing. We find out the patient’s blood group to make sure the donated blood is safe. The main groups are A, B, AB, and O, each with its own traits.
Getting the blood type right is key to avoid serious reactions. These reactions can be very dangerous.
- The ABO blood group system is the most critical factor in determining compatibility.
- Rh factor is another important consideration, as it can also impact the compatibility of the blood.
Knowing the patient’s blood type helps us pick the right blood for them. This makes the treatment safer and more effective.
Crossmatching Process
The crossmatching process is a final check to make sure the blood is safe. It mixes the donor’s red blood cells with the recipient’s serum to look for bad reactions. A compatible match is key for a safe transfusion.
“The crossmatch is the final check before transfusion, ensuring that the blood is safe for the recipient.”
AABB Standards
This process is very detailed and important. We do it to find any problems that could cause bad reactions. This way, we make sure the transfusion is safe and works well.
- The donor’s red blood cells are mixed with the recipient’s serum.
- The mixture is then observed for signs of hemolysis or agglutination.
- If no adverse reaction is observed, the blood is deemed compatible for transfusion.
Through pre-transfusion testing, like blood typing and crossmatching, we make blood transfusions safer and more effective. Our strict testing ensures patients get the best care.
Potential Risks and Side Effects
Blood transfusions are generally safe but can have risks. We’ll look at these risks and side effects. This helps patients make informed decisions about their care.
Immediate Reactions
Immediate reactions to blood transfusions can vary. They can be mild or severe. These reactions include:
- Allergic reactions, which can show as hives, itching, or severe anaphylactic reactions.
- Hemolytic reactions, where the transfused blood is attacked by the patient’s immune system, leading to the destruction of red blood cells.
- Transfusion-related acute lung injury (TRALI), a serious condition characterized by the onset of non-cardiogenic pulmonary edema.
It’s important to understand these immediate reactions. Healthcare providers closely watch patients during transfusions. They quickly identify and manage any adverse reactions.
Long-term Implications
Long-term effects of blood transfusions can impact health. Some of these effects include:
- Iron overload, a condition that can occur with frequent transfusions, leading to damage in various organs such as the heart, liver, and endocrine glands.
- Transfusion-transmitted infections, though rare, are a risk due to strict screening.
- Immunomodulation, where the immune system’s response is altered, potentially increasing the risk of infections or affecting the outcome of surgeries.
To reduce these risks, healthcare providers use several strategies. They monitor iron levels, use leukoreduced blood components, and follow strict donor screening protocols.
Description
| Risk | Management Strategy | |
| Allergic Reactions | Immune response to transfused blood | Antihistamines, corticosteroids |
| Hemolytic Reactions | Destruction of red blood cells | Prompt cessation of transfusion, supportive care |
| TRALI | Non-cardiogenic pulmonary edema | Supportive care, oxygen therapy |
| Iron Overload | Excess iron accumulation | Iron chelation therapy |
Understanding the risks and side effects of blood transfusions is key. Patients and healthcare providers can work together. This helps minimize risks and ensures the best outcomes.
Emotional and Psychological Considerations
Blood transfusions are more than just a medical procedure. They have a big emotional and psychological effect on patients. The process can make people feel anxious or relieved.
Coping with the Need for Transfusions
Understanding why you need a blood transfusion is key. Patients often feel a mix of emotions, like fear or gratitude. It’s important to talk openly with your healthcare team to ease worries.
Having emotional support is very important. Patients should share their feelings with others. Family and friends can help a lot, making you feel less alone and anxious.
Support Systems Available
There are many ways to get help with the emotional side of blood transfusions. Support groups let patients share their stories and learn from others. They can be in-person or online.
Counseling services also offer emotional support. They help patients deal with their feelings and adjust to treatment. Don’t forget to ask your healthcare team for help too. They can support you both medically and emotionally.
By recognizing the emotional and psychological effects of blood transfusions, patients can handle their treatment better. Using the support available can improve their overall well-being.
Page Page Conclusion: The Importance of Blood Transfusions
Blood transfusions are key in patient care, mainly for those getting chemotherapy. They are vital for managing anemia and supporting blood production. They also help in recovery.
Impact on Recovery
Blood transfusions greatly aid in recovery. They replace lost blood components, helping patients regain strength and reduce fatigue. This improves their overall health.
Encouraging Blood Donation
To have enough blood for transfusions, we urge eligible people to donate. Groups like the American Red Cross and local blood banks work hard to collect and distribute blood. Donating blood can greatly help patients in need.
As medical care advances, blood transfusions remain essential for many treatments. We thank blood donors and healthcare workers for their dedication. Together, they provide life-saving care.
FAQ
Why do people need blood transfusions?
Blood transfusions replace or supplement blood components. This is needed when these components are low or not working right. This often happens due to disease or treatments like chemotherapy.
What is a blood transfusion?
A blood transfusion is when blood or its parts are given to a patient. It’s to replace or add to blood components that are low or not working.
Why do cancer patients undergoing chemotherapy need blood transfusions?
Cancer patients on chemotherapy may need transfusions. This is to manage anemia, low white blood cell counts, and bleeding. Chemotherapy can weaken the bone marrow.Page>
What are the possible risks and side effects of blood transfusions?
Blood transfusions can cause immediate reactions like allergic reactions and hemolytic reactions. They can also lead to long-term issues like iron overload and infections. These are due to the transfusion itself.
Can you donate blood if you have cancer?
No, people with cancer usually can’t donate blood. Cancer can be passed through blood transfusions. Also, some cancer treatments can make the blood quality poor.
How many blood transfusions can a person have?
The number of transfusions varies based on the person’s health and treatment needs. Some may need many transfusions during their treatment.
What are the signs that indicate a blood transfusion may be necessary?
Signs like fatigue, shortness of breath, dizziness, and pale skin may mean a transfusion is needed. This is true for patients on chemotherapy or with bleeding issues.
Why are blood transfusions critical for patients undergoing chemotherapy?
Blood transfusions help manage side effects of chemotherapy. This includes anemia and low blood cell counts. These issues can affect treatment success and quality of life.
Are blood transfusions serious medical procedures?
Yes, blood transfusions are serious. They need careful thought and monitoring. This is to avoid risks and ensure safe treatment.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra2207946