Last Updated on November 17, 2025 by Ugurkan Demir

Having a blood clot is a serious and potentially dangerous situation. It’s important to know about fibrinolysis, the body’s way to break down clots. This knowledge is key for both patients and doctors.
At Liv Hospital, we follow the latest research and best practices. We help those with blood clots. How long it takes for a clot to dissolve depends on its size, location, and the body’s fibrinolysis process.
The fibrinolysis process starts with plasmin breaking down the clot. Some clots can dissolve by themselves, but medical help can speed up this process. Usually, it takes weeks to months for a clot to fully dissolve.
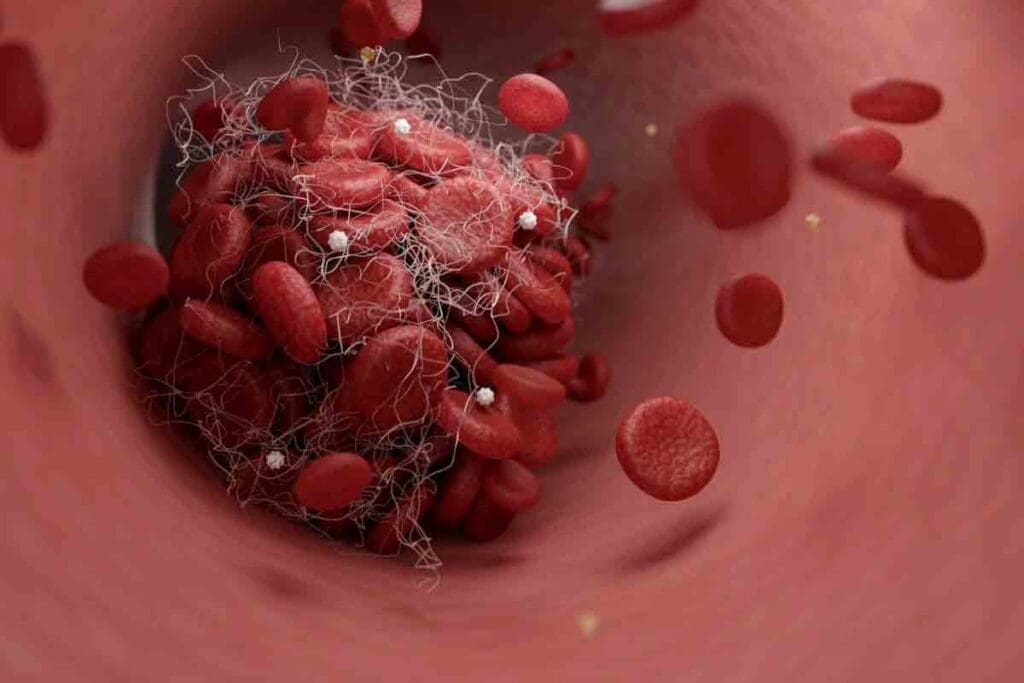
It’s important to know how blood clots form to understand the risks. Blood clots are like gel-like clumps of blood. They form when the body’s clotting mechanism is triggered. This process involves many factors and cells working together to stop bleeding when we’re hurt.
The clotting mechanism is key to our body’s health. It involves several steps and components. When a blood vessel gets injured, the body first constricts it to reduce blood flow.
Platelets, small cell fragments, then stick to the injury site, forming a plug. This plug is strengthened by a fibrin clot. This clot is made through chemical reactions involving clotting factors.
Clotting factors are proteins in the blood that work together to form fibrin. The fibrin clot traps blood cells, platelets, and other debris. This creates a solid clot that stops bleeding. This process is vital for preventing too much blood loss and helping us heal.
Blood clots can form in different parts of the body. This leads to various types of clots with different risks and consequences. The two main types are Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE).
Knowing about the different types of blood clots and where they form is key. It helps us recognize signs and symptoms. This can lead to timely medical help.
Fibrinolysis is how our bodies naturally break down blood clots. It’s a key part of getting better after a clot forms. This process uses the enzyme plasmin to break down fibrin, the main clot component.
When a blood clot forms, the fibrinolytic system kicks in. Plasminogen turns into plasmin, which breaks down the clot. This is important for keeping blood flowing well and avoiding damage.
Small clots in superficial veins might dissolve by themselves. The size and location of the clot, and the person’s health, play big roles. Also, any conditions that affect clotting or fibrinolysis matter.
In some cases, the body can break down small clots. This helps restore normal blood flow.
Even though fibrinolysis is natural, sometimes we need medical help. Big clots or those in important places like deep veins or lungs need treatment. Anticoagulant therapy or thrombolytic treatment might be needed to manage the clot.
Knowing when to get medical help is key. Signs like more pain, swelling, or trouble breathing mean you should see a doctor right away.
When someone is diagnosed with DVT, they often ask how long it takes for the clot to go away. The time it takes for Deep Vein Thrombosis to resolve can vary a lot. This depends on several factors.
The process of dissolving DVT is slow and can take weeks or even months. Usually, it takes the body 3 to 6 months to fully dissolve a clot. But, this time can change based on the clot’s size and where it is, and the patient’s health.
Several things can affect how fast a DVT dissolves. These include:
As DVT dissolves, patients will hit several recovery points. These include:
It’s key to keep an eye on the dissolving process with regular doctor visits. Tests like ultrasound help track how the clot is doing. They also help doctors adjust treatment if needed.
Pulmonary embolism (PE) is a serious condition where a blood clot blocks the lungs’ blood vessels. The time it takes for this clot to dissolve varies among individuals. Knowing what affects this process helps both patients and healthcare providers manage the condition better. We will look at typical dissolution times, factors that influence resolution, and the long-term outlook after treatment.
The time it takes for a pulmonary embolism to dissolve can range from weeks to months. Anticoagulant therapy is used to prevent more clots and help dissolve the existing one naturally.
Several factors can affect how quickly a pulmonary embolism dissolves. These include the clot’s size and location, the patient’s age, overall health, and any underlying medical conditions.
| Factor | Impact on PE Resolution |
| Clot Size | Larger clots may take longer to dissolve |
| Patient Age | Older patients may have slower resolution |
| Overall Health | Presence of comorbidities can complicate resolution |
| Anticoagulant Therapy | Essential for preventing new clots and aiding dissolution |
The long-term outlook for patients after PE treatment varies. While many recover fully, some may face long-term complications like chronic thromboembolic pulmonary hypertension (CTEPH).
Effective management of pulmonary embolism requires a detailed approach. This includes anticoagulant therapy and lifestyle changes. Monitoring and follow-up are key to spotting complications early.
Knowing what affects how fast a blood clot dissolves is key to good treatment. Many things can influence this rate. These include the clot’s size and location, the patient’s health, and their genes.
The size and where a blood clot is located greatly affect how fast it dissolves. Bigger clots dissolve slower than smaller ones. Clots in deeper veins, like in the legs, dissolve differently than those in shallower veins.
| Clot Characteristic | Impact on Dissolution Time |
| Clot Size | Larger clots generally take longer to dissolve |
| Clot Location | Deep vein clots may take longer than superficial clots |
A person’s age and health can really affect how well their body dissolves blood clots. Older people might have trouble dissolving clots because they’re less active and might have health issues. People with long-term illnesses, like diabetes or heart disease, also face challenges.
Key health factors influencing clot dissolution include:
Genetics can also play a part in how fast a blood clot dissolves. Some people might have genes that make their blood clot faster or slower. This can affect how quickly a clot forms and dissolves.
Understanding these genetic factors can help healthcare providers tailor treatment plans to individual patients.
Blood thinners are often used to manage blood clots. But do they actually dissolve them? The answer depends on how anticoagulants work and their role in managing clots.
Anticoagulants, or blood thinners, don’t dissolve blood clots directly. Instead, they stop the clot from getting bigger. This lets the body break it down naturally through fibrinolysis.
This process is key for managing deep vein thrombosis (DVT) and pulmonary embolism (PE). By stopping clotting factors in the liver or blocking their action, blood thinners reduce clot growth. This gives the body’s natural fibrinolytic system a chance to dissolve the clot over time.
There are several anticoagulants available, each with its own effectiveness and guidelines. Some of the most commonly used include:
These medications are effective in preventing clot growth and reducing the risk of new clots. The choice of anticoagulant depends on the type and location of the clot, the patient’s health, and drug interactions.
| Anticoagulant | Typical Use | Monitoring Requirements |
| Warfarin | DVT, PE, Atrial Fibrillation | Regular INR monitoring |
| Rivaroxaban | DVT, PE, Stroke prevention | No routine monitoring needed |
| Apixaban | DVT, PE, Atrial Fibrillation | No routine monitoring needed |
| Dabigatran | DVT, PE, Atrial Fibrillation | No routine monitoring needed |
The length of anticoagulant therapy varies by clot type, location, and patient risk factors. For example, patients with provoked DVT may need 3-6 months of treatment. Those with unprovoked DVT or PE might need treatment for longer, sometimes forever.
For atrial fibrillation, treatment is often long-term to prevent stroke. The decision on treatment length is made based on the risk of clot recurrence versus bleeding complications.
Understanding blood thinners’ role in clot management is key to effective treatment. They don’t dissolve clots directly but are vital in preventing clot growth and allowing the body to naturally resolve them.
To dissolve blood clots fast, doctors use many treatments. These include medicines and surgeries. We’ll look at how these help patients get better from blood clots.
Thrombolytic drugs quickly break down blood clots in serious cases. They start the body’s natural process to dissolve the clot. This makes the clot smaller and easier to absorb.
Common Thrombolytic Medications:
These drugs are given through an IV or directly into the clot. They work well but can cause bleeding. Doctors use them only when the clot is very serious.
Catheter-directed thrombolysis (CDT) is a less invasive method. It uses a catheter to deliver the drug right to the clot. This method is safer and more effective than giving the drug all over the body.
Benefits of CDT:
Sometimes, surgery is needed to remove a blood clot. Surgical thrombectomy removes the clot from the blood vessel.
| Treatment Option | Indications | Benefits | Risks |
| Thrombolytic Medications | Severe or life-threatening clots | Rapid clot dissolution | Bleeding complications |
| Catheter-Directed Thrombolysis | Large or limb-threatening clots | Targeted therapy, reduced bleeding risk | Procedure-related complications |
| Surgical Thrombectomy | Failed medical therapy or CDT, large clots | Immediate clot removal | Surgical risks, recovery time |
Knowing about these treatments helps both patients and doctors choose the best option for blood clots.
Natural methods like changing your diet and staying active can help dissolve blood clots. These steps can boost your recovery and health, alongside medical care.
Eating a balanced diet with lots of fruits, veggies, and whole grains helps your body dissolve clots naturally. Some foods and supplements might also help with clot dissolution.
| Food | Nutrient | Potential Benefit |
| Fatty fish | Omega-3 fatty acids | Improves circulation |
| Nuts and seeds | Vitamin E | Prevents platelet aggregation |
| Berries and leafy greens | Antioxidants | Reduces inflammation |
Light exercise, as advised by doctors, can help you recover by improving blood flow and preventing more clots.
Drinking enough water is key for blood flow and clot management. Staying hydrated supports your body’s natural clot-dissolving processes.
Monitoring blood clot dissolution involves both tests and watching for signs. It’s key to track how clots dissolve to adjust treatments and avoid problems.
Ultrasound is used to check clot size and location, mainly for DVT. For PE, computed tomography pulmonary angiography (CTPA) helps see the clot’s size and where it is.
D-dimer blood tests show if a clot is dissolving by measuring a protein fragment. Regular blood tests also check if anticoagulant therapy is working and safe.
When a clot dissolves, patients might see swelling and pain lessen. For PE, better breathing and less chest pain mean the clot is breaking down.
It’s important for patients to notice these signs and talk to their doctor. While these signs are good, they can’t replace tests.
Regular check-ups with doctors are key to tracking clot dissolution. They can adjust treatments based on how the patient is doing and test results.
Patients should talk about their symptoms and any changes. This teamwork helps make sure the treatment is right for them.
It’s important to know about the risks when dissolving blood clots. We’ll look at bleeding risks and long-term issues like post-thrombotic syndrome.
Bleeding is a big risk with blood clot dissolution, mainly with anticoagulants. Anticoagulants stop new clots and prevent existing ones from growing. But they also raise the chance of bleeding. A study on PMC shows managing this risk is key for safety.
“The use of anticoagulants requires careful monitoring to balance the risk of clot formation against the risk of bleeding,” say doctors. To lower these risks, doctors watch patients closely and adjust their treatment as needed.
Post-thrombotic syndrome (PTS) is a long-term issue after deep vein thrombosis (DVT). It causes chronic pain, swelling, and skin color changes in the affected limb. PTS can greatly affect a patient’s life quality, so managing DVT well is important.
Wearing compression stockings and using the right anticoagulants can help prevent PTS. Catching DVT early and treating it right away is also key.
Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare but serious issue after a pulmonary embolism (PE). It’s high blood pressure in the lungs’ arteries due to long-term clots. CTEPH can cause right heart failure if not treated, so early diagnosis and treatment are critical.
Managing CTEPH often means a mix of medicine and sometimes surgery like pulmonary thromboendarterectomy. Regular monitoring and follow-up care are essential for those who’ve had a PE.
When recovering from a blood clot, it’s key to stop new clots from forming. There are many ways to do this. These strategies are important for a smooth recovery.
Compression therapy is a top choice for stopping new blood clots. Compression stockings or sleeves boost blood flow in the legs. This reduces clot risk by preventing blood from pooling in veins.
Compression therapy does more than just prevent clots. It also cuts down swelling and eases pain. Always talk to a doctor to find the right compression level and type for you.
Moving and exercising regularly is vital for clot prevention. Gentle exercises like walking or stretching boost circulation. We suggest short walks, even during long trips or when sitting for a while.
It’s bad to sit too long without moving. Simple moves like flexing your feet or ankles help blood flow. If you can’t move much, a doctor can help create a special exercise plan for you.
Changing your lifestyle can also help prevent blood clots long-term. Keeping a healthy weight is key, as extra weight puts more pressure on veins. Quitting smoking and drinking less alcohol also helps keep your blood flowing well.
Drinking enough water is also important. It makes your blood thinner and improves circulation. Eating a diet full of fruits, veggies, and whole grains is good for your heart too.
It’s important to know about blood clot dissolution and prevention. We talked about how things like clot size and location matter. Age and health also play a big role.
A summary on blood clot dissolution shows how key timely medical help is. Drugs like anticoagulants and thrombolytics help manage clots. Making lifestyle changes and using compression therapy can also help prevent and recover from blood clots.
Preventing and treating blood clots requires a full approach. Knowing the risks and symptoms is key. Following your doctor’s advice is also important. Combining medical treatment with lifestyle changes can lower the risk of blood clots and improve heart health.
We suggest talking to a healthcare professional to make a plan for managing and preventing blood clots. This way, you can take care of your heart health.
The time it takes for a blood clot to dissolve varies. It depends on the clot’s size, location, and the person’s health. It can take from a few days to several weeks or months.
Yes, blood clots can dissolve naturally through fibrinolysis. But sometimes, medical help is needed to avoid complications.
DVT dissolution time varies. It usually takes weeks to months. The size, location of the clot, and health play a role in how fast it dissolves.
Pulmonary embolism dissolution time varies. It usually takes days to weeks with proper treatment.
Blood thinners don’t dissolve clots directly. They prevent new clots and help the body dissolve existing ones.
Several things help dissolve blood clots. Anticoagulant therapy, thrombolytic medications, and lifestyle changes like diet and exercise are helpful.
Some blood clots can dissolve naturally. But others need medical treatment to avoid complications. Seek medical help if symptoms don’t improve or get worse.
The body’s fibrinolysis process breaks down blood clots. Thrombolytic medications can also speed up this process.
Preventing new clots involves lifestyle changes and medical treatment. Use compression therapy, exercise regularly, and follow a healthy diet. Also, take prescribed anticoagulant therapy as directed.
Signs of clot dissolution include reduced swelling, less pain, and better mobility. Ultrasound tests can also show if the clot is dissolving.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!