Last Updated on November 26, 2025 by Bilal Hasdemir

At Liv Hospital, we know how vital effective treatment options are for brain cancer. Brain tumor medicine includes many drugs. These include chemotherapy agents and targeted therapies, key to treating brain cancer.
Recent studies highlight temozolomide as a top choice. It’s great because it can get past the blood-tumor barrier. We help our patients with the newest treatments, aiming for the best care and results for each person.
Key Takeaways
- Temozolomide is a widely used chemotherapy drug for brain cancer.
- Liv Hospital provides world-class healthcare with a focus on individualized treatment.
- Brain cancer treatment involves a range of medications, including targeted therapies.
- Effective treatment options are key to better patient outcomes.
- Liv Hospital’s teams guide patients through the latest therapies.
Understanding Brain Tumor Medicine and Treatment Approaches
Effective treatment of brain tumors needs a deep understanding of available medicines. We will look at the different ways to treat brain tumors. This includes the role of medicines and the challenges they face.
The Role of Medications in Brain Cancer Treatment
Medications are key in treating brain cancer. They target cancer cells, slowing their growth. These drugs can be used alone or with other treatments like surgery and radiation.
“The use of chemotherapy in brain cancer treatment has changed how we manage this disease,” a leading neuro-oncologist. “By knowing how different medicines work, we can make treatments more effective.”
How Brain Tumor Drugs Work
Brain tumor chemotherapy drugs target fast-growing cancer cells. They can be taken by mouth or given through an IV, based on the drug and treatment plan. The goal is to get the drug to the tumor without harming healthy tissue.
The way these drugs work varies. Some damage cancer cells’ DNA, while others stop cell division. Knowing how they work helps choose the best treatment.
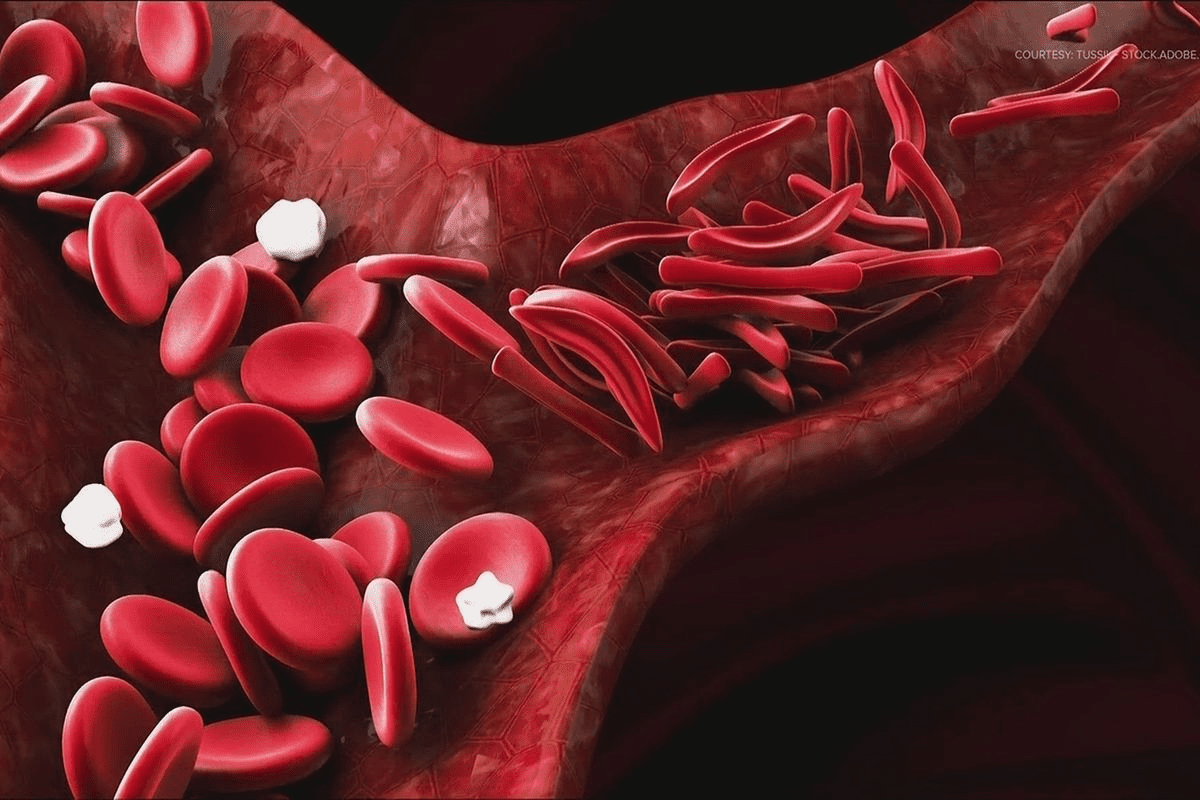
The Blood-Brain Barrier Challenge
One big challenge in treating brain tumors is the blood-brain barrier (BBB). The BBB keeps many substances, including some medicines, out of the brain. This barrier makes it hard for gbm chemotherapy drugs to work, so finding ways to get past it is key.
Scientists are working on new brain cancer treatment drugs that can get past the BBB better. Until then, doctors must pick medicines that can get through the BBB or find other ways to deliver them.
Temozolomide: The First-Line Brain Tumor Medicine
Temozolomide is a key treatment for glioblastoma. It has greatly improved how we treat brain tumors. This chemotherapy drug is a major part of brain tumor medicine.
Temozolomide is chosen because it can get past the blood-brain barrier. This makes it perfect for treating brain tumors. It works by damaging the DNA of cancer cells, stopping them from growing and reproducing.
How Temozolomide Works Against Brain Tumors
Temozolomide damages DNA in cancer cells, which stops them from making more cells. This leads to cell death, slowing tumor growth. We use it with other treatments to make it more effective.
Effectiveness in Glioblastoma Treatment
Temozolomide is very effective against glioblastoma, even more so when combined with radiation therapy. Research shows that patients live longer when they take temozolomide as part of their treatment.
| Treatment Regimen | Survival Rate Improvement | Common Side Effects |
|---|---|---|
| Temozolomide + Radiation Therapy | 25% | Nausea, Fatigue |
| Temozolomide Alone | 15% | Hair Loss, Nausea |
Common Side Effects and Management
Temozolomide can cause side effects like nausea, fatigue, and hair loss. We help manage these with supportive care, like anti-nausea meds and rest. Sometimes, we adjust the dosage to lessen severe side effects.
Knowing how temozolomide works and its side effects helps us care for patients better. We aim to provide full care that meets both physical and emotional needs.
Carmustine (BCNU): A Powerful Alkylating Agent
Carmustine is a key player in fighting brain tumors. It’s vital in treating brain cancers like glioblastoma multiforme (GBM).
Mechanism of Action in Brain Cancer Cells
Carmustine works by adding groups to DNA, stopping cancer cells from copying themselves. This is key in slowing down brain tumors. Its ability to get past the blood-brain barrier makes it great for brain cancer treatment.
A study in the Journal of Neuro-Oncology found Carmustine is very effective against malignant gliomas.
“Carmustine has been a mainstay in the treatment of glioblastoma, giving patients a valuable option against this aggressive brain cancer.”
Wafer Implantation vs. Intravenous Administration
Carmustine can be given in two ways: as wafers implanted in the tumor or through an IV. Wafers deliver the drug right to the tumor, which can lower side effects.
| Administration Method | Advantages | Disadvantages |
|---|---|---|
| Wafer Implantation | Localized delivery, reduced systemic side effects | Limited to surgically accessible tumors |
| Intravenous Administration | Systemic distribution, can target multiple tumor sites | Higher risk of systemic side effects |
Patient Selection and Considerations
Choosing the right patients for Carmustine treatment is complex. It depends on the cancer type, stage, past treatments, and overall health. We focus on personalized plans to improve results and reduce side effects.
Understanding Carmustine’s treatment details helps us tailor plans for each patient’s needs.
Lomustine (CCNU): Oral Nitrosourea for Brain Tumors
Lomustine is a key oral nitrosourea in treating brain tumors. It plays a big role in chemotherapy for brain cancer patients. This helps improve their treatment results.
Treatment Protocol and Effectiveness
Lomustine is easy to take because it’s an oral medication. The dosage and treatment plan depend on the patient’s health and tumor type. Research shows it works well on some brain tumors, like glioblastoma.
Lomustine’s success comes from its ability to get past the blood-brain barrier. This lets it directly attack tumor cells. This makes it a key part of brain tumor treatment.
Managing Lomustine’s Side Effect Profile
Lomustine usually has mild side effects like nausea, vomiting, and tiredness. It’s important to manage these side effects well. This helps patients stay on their treatment plan. We suggest patients work with their healthcare team to find ways to handle side effects.
Combination Therapy Applications
Lomustine is often paired with other drugs to boost its effectiveness. The PCV combination, with procarbazine, lomustine, and vincristine, is a common treatment for some brain tumors. Using it with other drugs can lead to better results for aggressive tumors.
Understanding lomustine’s role in treating brain tumors helps us support patients better. We can help them navigate the benefits and challenges of their treatment.
The PCV Combination: Procarbazine, CCNU, and Vincristine
Procarbazine, CCNU, and vincristine are known as the PCV combination. They are a strong mix for treating brain cancer. This mix has been key in fighting certain brain tumors. It works by combining the strengths of each drug to better fight cancer.
Synergistic Effects of the PCV Regimen
The PCV mix attacks cancer cells in different ways. Procarbazine damages DNA in cancer cells, stopping them from copying. CCNU (Lomustine) also damages DNA, making the treatment stronger. Vincristine stops cells from dividing by messing with their structure.
This multi-action approach helps the PCV mix target brain tumor cells well. It can lead to better results than using one drug alone.
Ideal Candidates for PCV Therapy
People with certain brain tumors, like oligodendrogliomas, might get better with PCV. Choosing PCV depends on the tumor type, genetic markers, and the patient’s health.
We look at each patient’s situation to see if PCV is right for them. We check the tumor and the patient’s health history.
Treatment Schedule and Monitoring
The PCV treatment goes in cycles, lasting 6-8 weeks. Procarbazine is taken orally for 14 days. CCNU is taken orally on day 1. Vincristine is given through an IV on days 1 and 8.
We watch for side effects like low blood counts, nerve damage, and stomach problems. Regular blood tests and checks on the nervous system help manage these issues. We adjust the treatment as needed.
Bevacizumab (Avastin): Targeted Therapy for Recurrent Tumors
Bevacizumab, also known as Avastin, is a key treatment for recurrent brain tumors. It has shown promise in improving outcomes for those with brain cancer that keeps coming back.
Anti-Angiogenic Mechanism of Action
Bevacizumab stops new blood vessels from forming. Tumors need new blood vessels to grow. By blocking vascular endothelial growth factor (VEGF), it stops tumors from getting the nutrients they need.
In the case of recurrent brain tumors, bevacizumab is a game-changer. It targets the tumor’s ability to grow by creating new blood vessels. This offers a new way to fight the disease.
Effectiveness in Reducing Brain Swelling
Bevacizumab is also great at reducing brain swelling. This swelling, or edema, can cause headaches and seizures. By reducing swelling, it improves symptoms and quality of life for patients.
Studies show bevacizumab can cut down on swelling around tumors. This is key for patients with tumors that keep coming back. It helps manage symptoms and keeps the brain working better.
Response Assessment Challenges
It’s hard to tell how well bevacizumab is working. MRI scans might not show the full picture because of the drug’s effects. So, doctors have to look at more than just scans to understand how the treatment is doing.
New imaging and tools are being developed. They help doctors see how well the treatment is working. This includes advanced MRI scans and other tests that give more detailed information.
Everolimus: mTOR Inhibition in Brain Tumors
Everolimus is important in treating brain tumors linked to tuberous sclerosis complex. It blocks the mTOR pathway. This pathway controls cell growth, division, and survival.
Treatment of Subependymal Giant Cell Astrocytomas
Everolimus is used for subependymal giant cell astrocytomas. These tumors happen in people with tuberous sclerosis complex. It makes these tumors smaller and relieves symptoms.
Key Benefits of Everolimus:
- Reduces tumor size
- Alleviates symptoms
- Targeted therapeutic approach
Molecular Targeting Approach
The mTOR pathway is key for cell functions. In tuberous sclerosis complex, it’s overactive due to gene mutations. Everolimus blocks this pathway, giving a precise treatment.
Patient Monitoring Requirements
Monitoring patients on everolimus is vital. It checks if the treatment works and is safe. This includes:
| Monitoring Parameter | Frequency |
|---|---|
| Tumor size assessment | Every 3-6 months |
| Liver function tests | Monthly |
| Blood counts | Monthly |
Regular checks help doctors adjust the treatment for better results.
Cisplatin and Carboplatin: Platinum-Based Therapies
In the fight against brain tumors, cisplatin and carboplatin are key players. They are used a lot, mainly in kids, because they target fast-growing cancer cells well.
Applications in Pediatric Brain Tumors
Cisplatin and carboplatin are big in treating brain tumors in kids. They can get past the blood-brain barrier, making them good against many brain cancers. We mix them with other drugs to make them work better.
Using cisplatin in kids has shown good results, like in medulloblastoma and germ cell tumors. Carboplatin, though, has fewer side effects, which makes it a better choice sometimes.
Overcoming Resistance Mechanisms
But, tumors can grow resistant to these drugs. They might fix DNA damage faster or not take in the drugs as well. To beat this, we’re looking at mixing these drugs with others to make tumors more sensitive.
Strategies to overcome resistance include:
- Combining platinum-based therapies with other chemotherapy agents
- Using drugs that inhibit DNA repair mechanisms
- Modulating the dose and schedule of platinum-based therapies
Nephrotoxicity and Ototoxicity Management
Cisplatin can harm kidneys and ears. To lessen these effects, we use a few methods. We give lots of water and use drugs like amifostine to protect kidneys. For ear damage, we watch hearing with tests and adjust doses to avoid hearing loss.
It’s important to manage side effects well. This way, patients can stick to their treatment plans without big breaks. By watching patients closely and tweaking treatment plans, we can lessen the bad effects of cisplatin and carboplatin.
Etoposide: Topoisomerase Inhibitor for Brain Cancer
Etoposide is a key player in fighting brain cancer. It works by stopping the growth of cancer cells. We’ll look at how it works, how it’s given, and its role in saving lives.
Mechanism of DNA Damage in Cancer Cells
Etoposide blocks topoisomerase II, a vital enzyme for DNA and cell growth. This action damages cancer cells’ DNA, stopping them from growing.
Key Mechanism: It traps the topoisomerase II-DNA complex, causing DNA breaks. This leads to cancer cells dying off.
Oral vs. Intravenous Administration
Etoposide can be taken by mouth or given through an IV. Each way has its own benefits and things to think about.
| Administration Method | Advantages | Considerations |
|---|---|---|
| Oral | Easy for patients to take at home, less invasive | How well it’s absorbed can vary, might upset the stomach |
| Intravenous | Guarantees the right dose, good for those in the hospital | Needs a vein for injection, might cause reactions |
Role in Salvage Therapy
Etoposide is a go-to for patients with brain tumors that come back or don’t respond to treatment. It’s special because it can get into the brain.
Etoposide is a vital option for those with few other choices. It shows how important it is in treating brain cancer.
Emerging Brain Tumor Drugs and Experimental Therapies
The field of brain tumor treatment is changing fast. New treatments are being developed to help patients more. We’re moving towards treatments that are more targeted and tailored to each person.
Immunotherapy Approaches for Brain Tumors
Immunotherapy uses the body’s immune system to fight cancer. Checkpoint inhibitors and CAR-T cell therapy are being tested. They aim to help the body fight tumor cells better.
Immunotherapy for brain tumors is just starting. But early results look good. More trials are needed to see how well it works.
Targeted Molecular Therapies in Development
Targeted molecular therapies target specific genetic changes in tumors. BRAF inhibitors and IDH inhibitors are being studied for brain tumors. They aim to kill cancer cells without harming healthy ones.
Creating these therapies requires knowing a lot about tumor genetics. Genetic profiling helps find the right targets for treatment.
Personalized Medicine and Genetic Profiling
Personalized medicine is changing how we treat brain tumors. It tailors treatments to each patient’s unique genetic profile. Genetic profiling helps find specific mutations to target.
Using genetic profiling in treatment planning is a big step forward. It lets us choose the best treatments for each patient’s tumor.
The future of brain tumor treatment looks bright. With new drugs, immunotherapy, and personalized medicine, we can hope for better outcomes. Ongoing research and trials will guide us forward.
Conclusion: The Future of Brain Tumor Medicine
The future of brain tumor medicine looks bright. Ongoing research is leading to better treatments. New therapies for brain cancer are giving hope to patients all over the world.
At Liv Hospital, we’re dedicated to top-notch care for international patients. We use the latest in brain tumor treatment. Our team works hard to give patients the best care, from start to finish.
We’re always looking to improve brain tumor medicine. Our focus is on personalized care for each patient. With new treatments on the horizon, we’re committed to helping patients make informed choices and achieve the best results.
FAQ
What is the role of medications in brain tumor treatment?
Medications are key in treating brain tumors. They help manage the disease in many ways. This includes using chemotherapy, targeted therapy, and immunotherapy to slow tumor growth and ease symptoms.
How do brain tumor drugs work?
Brain tumor drugs target cancer cells in different ways. They can stop DNA replication, block blood vessel growth, or target specific pathways. This helps fight cancer while protecting healthy tissue.
What is the blood-brain barrier, and how does it affect treatment?
The blood-brain barrier protects the brain by blocking certain substances. It can make it hard for some drugs to reach tumors. We work to find ways to get drugs past this barrier for effective treatment.
What is temozolomide, and how is it used in glioblastoma treatment?
Temozolomide is a chemotherapy drug for glioblastoma. It stops cancer cells from reproducing by damaging their DNA. We often use it with other treatments to get the best results.
What are the common side effects of temozolomide, and how can they be managed?
Side effects of temozolomide include nausea, fatigue, and low blood cell counts. We manage these with supportive care. This includes anti-nausea meds, rest, and checking blood counts regularly.
How does carmustine work, and what are its applications in brain cancer treatment?
Carmustine damages DNA in cancer cells, stopping them from growing. It’s used to treat brain tumors, often by implanting wafers directly into the tumor.
What is the PCV combination, and how is it used in brain cancer treatment?
The PCV combination is a chemotherapy mix of procarbazine, lomustine, and vincristine. It’s used for certain brain tumors. The drugs work together to treat the cancer more effectively.
How does bevacizumab work, and what are its benefits in treating recurrent brain tumors?
Bevacizumab stops new blood vessels from forming, starving tumors. It’s used to reduce swelling and slow tumor growth in recurrent brain tumors.
What is everolimus, and how is it used in treating subependymal giant cell astrocytomas?
Everolimus is an mTOR inhibitor for subependymal giant cell astrocytomas. It targets the mTOR pathway, which controls cell growth. This helps treat the tumor.
What are the emerging trends in brain tumor treatment?
New trends include immunotherapy, targeted therapies, and personalized medicine. We’re exploring ways to use the immune system, target genetic mutations, and tailor treatments for each patient.
How do institutions like Liv Hospital contribute to brain tumor treatment?
Places like Liv Hospital offer top-notch healthcare. They provide advanced treatments and personalized care for international patients. We aim to deliver cutting-edge care that meets each patient’s unique needs.