Last Updated on November 27, 2025 by Bilal Hasdemir

At Liv Hospital, we know how vital it is to understand abnormal heart rhythms on an electrocardiogram (ECG). An ECG shows the heart’s electrical activity as waveforms. Changes in these waveforms can point to arrhythmias or dysrhythmias.
These irregularities can cause a fast, slow, or irregular heartbeat. This can lead to symptoms and complications. Knowing about these rhythms is key for diagnosis and treatment. We’ll look at the most common arrhythmias, their meanings, and what they say about your heart’s health.
Key Takeaways
- Abnormal heart rhythms, or arrhythmias, are detected on ECG as deviations from the typical electrical activity pattern.
- An ECG measures the heart’s electrical activity as waveforms to identify disturbances in the normal cardiac rhythm.
- Understanding abnormal heart rhythms is vital for diagnosis and management.
- Arrhythmias can cause a fast, slow, or irregular heartbeat, leading to symptoms and complications.
- Liv Hospital offers top-notch cardiac care with a focus on patient-centered treatment.
Understanding Heart Rhythm Basics and ECG Interpretation
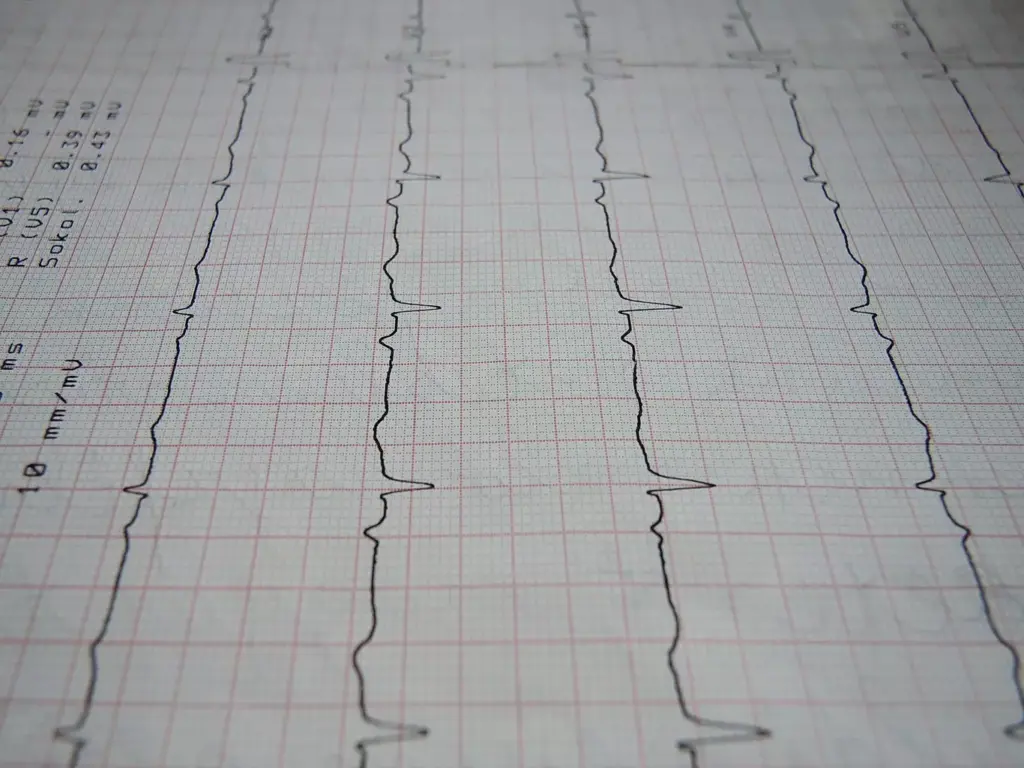
To understand abnormal heart rhythms, we must first learn about heart rhythm basics and ECG interpretation. An electrocardiogram (ECG) is a key tool for checking the heart’s electrical activity. We will look at what an ECG is, how it works, and why knowing normal heart rhythms is important.
What Is an Electrocardiogram (ECG)?
An ECG uses electrodes on the skin to catch the heart’s electrical signals. These signals are then sent to create a heart activity record. ECG interpretation is key to spotting both normal and abnormal heart rhythms.
Normal Heart Rhythm Patterns
A normal heart rhythm, or sinus rhythm, shows consistent electrical activity. It has a heart rate of 60 to 100 beats per minute (bpm). Knowing what a normal ECG looks like helps spot any heart rhythm problems.
How Heart Rate and Rhythm Are Measured
On an ECG, heart rate is found by counting the time between heartbeats. The rhythm is checked by looking at how consistent these intervals are. Doctors look for regular patterns and specific wave types to see if the heart rhythm is normal or if there’s an arrhythmia. Accurate measurement and interpretation are essential for diagnosing and treating heart rhythm issues.
Abnormal Heart Rhythms on ECG: Classification and Overview

Arrhythmias are heart rhythm and rate issues. Knowing about them is key for diagnosis and treatment. We sort these heart rhythm problems by their cause and features. This helps us figure out the best way to manage them.
Tachycardias vs. Bradycardias
Heart rhythms can be fast or slow. Tachycardias are when the heart beats too quickly, over 100 times a minute. Bradycardias happen when the heart beats too slowly, under 60 times a minute. Knowing this is important because it affects symptoms and treatment options.
Atrial vs. Ventricular Arrhythmias
Arrhythmias can start in different parts of the heart. Atrial arrhythmias start in the upper chambers, like atrial fibrillation. Ventricular arrhythmias start in the lower chambers, like ventricular tachycardia. Where the arrhythmia starts affects how it’s treated and its impact on the heart.
Impact on Cardiac Output and Symptoms
Arrhythmias can affect how well the heart works and cause symptoms. Symptoms can include dizziness, shortness of breath, and tiredness. How bad these symptoms are depends on the type of arrhythmia and the person’s heart health.
| Type of Arrhythmia | Origin | Characteristics |
|---|---|---|
| Tachycardia | Various | Heart rate > 100 bpm |
| Bradycardia | Various | Heart rate |
| Atrial Fibrillation | Atria | Irregular, rapid atrial rate |
| Ventricular Tachycardia | Ventricles | Fast, potentially life-threatening |
Atrial Fibrillation and Flutter: Chaotic Upper Chamber Rhythms
Atrial fibrillation and atrial flutter are common heart rhythm disorders. They affect patient outcomes a lot. These conditions cause irregular heart rhythms in the atria. This can raise the risk of stroke and other heart problems.
Atrial Fibrillation: Irregular Rhythm and Stroke Risk
Atrial fibrillation makes the heart’s upper chambers beat chaotically. This irregular rhythm increases the risk of stroke because of blood clots. People with atrial fibrillation might feel palpitations, shortness of breath, and fatigue.
Managing atrial fibrillation means controlling the heart rate and preventing stroke. Anticoagulation therapy is used. Sometimes, cardioversion or ablation is done to restore a normal rhythm.
Atrial Flutter: Rapid and Regular Atrial Activity
Atrial flutter has a rapid and regular atrial activity, showing a “sawtooth” pattern on the ECG. It can also raise the risk of stroke, but less than atrial fibrillation.
Managing atrial flutter includes rate control, rhythm control, and anticoagulation therapy. Ablation is a very effective treatment for atrial flutter. It can cure the condition.
Supraventricular Tachycardias: The Most Common Arrhythmias in Young Adults
Supraventricular tachycardias (SVTs) are common in young adults. They cause the heart to beat too fast, starting above the ventricles. We’ll look at how they work, their types, and what they look like on an ECG, focusing on AVNRT and AVRT.
AVNRT: AV Nodal Reentrant Tachycardia
AVNRT is a common SVT. It happens when the heart’s AV node gets stuck in a loop. This leads to a fast heart rate, usually between 150 to 250 beats per minute. It’s caused by a dual-pathway physiology within the AV node.
AVRT: AV Reentrant Tachycardia
AVRT is another SVT. It’s caused by an extra electrical pathway between the atria and ventricles. This makes the heart beat too fast. AVRT can be orthodromic or antidromic, depending on how the electrical impulse moves.
Identifying SVT on ECG Tracings
To spot SVTs on an ECG, look for certain signs. These include a narrow QRS complex tachycardia and specific rates. We’ll go over the ECG features that help tell AVNRT and AVRT apart.
| Characteristics | AVNRT | AVRT |
|---|---|---|
| Mechanism | Reentrant circuit within AV node | Accessory pathway between atria and ventricles |
| ECG Features | Narrow QRS, often without visible P waves | Narrow QRS, may show retrograde P waves |
| Rate | Typically 150-250 bpm | Variable, often 150-250 bpm |
For more detailed information on arrhythmias, we recommend visiting NCBI’s resource on cardiac arrhythmias.
Ventricular Tachyarrhythmias: Life-Threatening Rhythm Disturbances
It’s key for doctors to know about ventricular tachyarrhythmias to treat them right away. These serious heart rhythm problems can cause cardiac arrest if not treated quickly.
Ventricular Tachycardia: Sustained vs. Non-sustained
Ventricular tachycardia (VT) is a serious heart rhythm problem. It happens in the ventricles and has a fast heart rate, over 100 beats per minute. VT is divided into two types: sustained and non-sustained.
- Sustained VT: Lasts more than 30 seconds and can lead to hemodynamic instability.
- Non-sustained VT: Lasts less than 30 seconds and may not cause significant symptoms.
Both types of VT need careful checking and treatment to avoid bad outcomes.
Ventricular Fibrillation: Cardiac Arrest Rhythm
Ventricular fibrillation (VF) is a severe heart rhythm problem. It can cause sudden cardiac arrest. It’s a chaotic rhythm that makes the heart pump blood poorly.
“Ventricular fibrillation is a medical emergency that requires immediate defibrillation and advanced cardiac life support to restore a viable cardiac rhythm.”
Quick recognition and treatment of VF are critical. Delaying can lower the chance of successful resuscitation.
We stress the need to understand these serious heart rhythm problems. This is to give the right care and better patient results.
Bradyarrhythmias: When the Heart Beats Too Slowly
A slow heart rate, or bradyarrhythmia, needs careful diagnosis and management. It can lead to serious problems if not treated right. There are different types, like sinus bradycardia and heart blocks, each with its own signs and treatment needs.
Sinus Bradycardia: Physiologic vs. Pathologic
Sinus bradycardia is when the heart beats slower than usual, under 60 beats per minute. It starts in the sinoatrial node. It can be normal in athletes or during sleep, or it can be caused by health issues, medicines, or problems with the sinoatrial node. It’s important to know the difference to treat it correctly.
“A slow heart rate is not always a cause for concern,” as it can be a normal adaptation in certain individuals. But, if it causes symptoms like dizziness, fatigue, or even fainting, it needs to be checked. We must look at the whole situation to find the real cause.
Heart Blocks on ECG
Heart blocks happen when the normal path between the atria and ventricles is disrupted. They are divided into three degrees based on how bad the block is. First-degree has a long PR interval on ECG, second-degree has missed beats, and third-degree means no connection between atrial and ventricular beats.
To spot heart blocks on an ECG, we need to look at the P wave, PR interval, and QRS complex. Knowing how to read an ECG well is key to finding these problems.
Treating bradyarrhythmias, like sinus bradycardia and heart blocks, depends on why it’s happening and how bad the symptoms are. Some people might not need treatment, but others might need a pacemaker or treatment for the cause.
Premature Beats and Ectopic Rhythms
It’s important to know about premature beats and ectopic rhythms to help patients with heart rhythm problems. These irregular heartbeats can be harmless or show a bigger issue with the heart. So, it’s key to spot and understand them well.
Premature Atrial Contractions (PACs)
Premature Atrial Contractions (PACs) start in the heart’s upper chambers. They can happen for many reasons, like stress or too much caffeine. On an ECG, PACs show up as an odd P wave and an early beat.
Clinical Implications: Most people with PACs don’t feel anything, but it can cause discomfort. For those with heart problems, PACs might mean a higher chance of other heart issues.
Premature Ventricular Contractions (PVCs)
Premature Ventricular Contractions (PVCs) start in the heart’s lower chambers. They are common in both healthy people and those with heart issues. PVCs are seen on an ECG as a wide QRS complex without a P wave before it.
Symptoms and Causes: PVCs can make people feel like their heart is skipping beats. They can be set off by stress, caffeine, or some medicines. Sometimes, they point to a bigger heart problem.
Clinical Significance and Management
The importance of premature beats and ectopic rhythms varies. It depends on why they happen, how often, and if they cause symptoms. Often, they are not serious and don’t need treatment. But, for those with heart disease, more checks and care might be needed.
“The presence of premature beats and ectopic rhythms on an ECG can provide valuable insights into a patient’s cardiac health, guiding further diagnostic testing and treatment strategies.”
Management Strategies: Treatment aims to fix the cause, ease symptoms, and stop problems. This might include changing lifestyle habits, taking medicines, or sometimes, more serious treatments like catheter ablation.
| Arrhythmia Type | ECG Characteristics | Common Causes |
|---|---|---|
| Premature Atrial Contractions (PACs) | Abnormal P wave, early atrial contraction | Stress, caffeine, underlying heart disease |
| Premature Ventricular Contractions (PVCs) | Wide QRS complex, no preceding P wave | Stress, caffeine, certain medications, underlying heart disease |
Understanding premature beats and ectopic rhythms helps doctors give better care. This leads to better health outcomes for patients.
Diagnosis and Treatment of Cardiac Arrhythmias
Diagnosing and treating cardiac arrhythmias needs a detailed approach. This includes using advanced diagnostic methods and creating personalized treatment plans. We will look at how to diagnose and manage arrhythmias, making sure patients get the right care for their condition.
Advanced Diagnostic Methods
Advanced diagnostic methods are key in finding and understanding cardiac arrhythmias. Techniques like electrocardiogram (ECG) monitoring, Holter monitoring, and electrophysiology studies (EPS) give important insights into the heart’s electrical activity.
ECG monitoring is a non-invasive test that records the heart’s electrical activity for 24 to 48 hours. Holter monitoring can record for up to several days, catching arrhythmias that happen less often. EPS involves putting catheters into the heart to directly record its electrical signals and induce arrhythmias safely.
| Diagnostic Method | Description | Clinical Use |
|---|---|---|
| ECG Monitoring | Non-invasive recording of heart’s electrical activity | Initial diagnosis and monitoring |
| Holter Monitoring | Extended ECG recording over several days | Capturing intermittent arrhythmias |
| Electrophysiology Studies (EPS) | Invasive recording of heart’s electrical signals | Detailed analysis and induction of arrhythmias |
Pharmacological Management
Medicine is a big part of treating cardiac arrhythmias. Drugs like beta-blockers, anti-arrhythmic drugs, and anticoagulants help control heart rate, restore rhythm, and prevent blood clots.
The right medicine depends on the arrhythmia type, patient’s health, and possible side effects. For example, beta-blockers slow the heart rate in fast arrhythmias, while anti-arrhythmic drugs keep the rhythm normal.
Ablation and Device Therapy
Ablation therapy uses energy to destroy abnormal heart pathways that cause arrhythmias. Catheter ablation is a minimally invasive method that works well for some arrhythmias, like AVNRT and atrial flutter.
Device therapy includes pacemakers and implantable cardioverter-defibrillators (ICDs). Pacemakers regulate the heart’s rhythm with electrical impulses. ICDs detect and correct dangerous arrhythmias by delivering a shock.
Lifestyle Modifications and Prevention
Changing your lifestyle is important in managing and preventing cardiac arrhythmias. Eating well, exercising, avoiding stimulants, and managing stress are key.
People with arrhythmias should know their condition and when to get medical help. Learning about symptoms and following treatment plans is essential for managing the condition well.
Prevention Strategies
- Maintain a healthy weight and diet
- Exercise regularly but avoid excessive strain
- Avoid caffeine and nicotine
- Manage stress through relaxation techniques
- Adhere to prescribed medication regimens
Conclusion: Managing and Living with Abnormal Heart Rhythms
Understanding and managing abnormal heart rhythms is key to good heart health. We’ve looked at different types of arrhythmias, how to diagnose them, and treatment options. To live well with these rhythms, we need a full plan that includes medical care, lifestyle changes, and learning about the condition.
Handling arrhythmias well means using medicine, ablation, and devices, along with making healthy lifestyle choices. It’s also vital to educate patients. When they know about their arrhythmia and how to manage it, they can live better.
In conclusion, managing abnormal heart rhythms is a complex task. We’re dedicated to top-notch healthcare for everyone, including international patients. With the help of doctors and patients working together, we can tackle the challenges of arrhythmia management and get the best results.
FAQ
What does an abnormal heartbeat mean on an ECG?
An abnormal heartbeat on an ECG might show a heart rate that’s too fast, too slow, or irregular. This could mean there’s a problem with the heart or an arrhythmia.
What are the most common types of arrhythmias?
Common arrhythmias include atrial fibrillation and atrial flutter. Also, supraventricular tachycardias (SVTs), ventricular tachycardia, and bradyarrhythmias like sinus bradycardia and heart blocks are common.
How are heart rate and rhythm measured on an ECG?
An ECG measures heart rate and rhythm by looking at the heart’s electrical activity. It checks the P wave, QRS complex, and T wave to see how fast and steady the heart is beating.
What is the difference between tachycardias and bradycardias?
Tachycardias are when the heart beats too fast. Bradycardias are when it beats too slow. Both can be treated with medical care.
What are the risks associated with atrial fibrillation?
Atrial fibrillation can lead to stroke, heart failure, and other heart problems. It’s important to manage it with anticoagulation therapy and other treatments.
How are premature atrial contractions (PACs) and premature ventricular contractions (PVCs) managed?
PACs and PVCs are usually harmless but might need treatment if they cause symptoms or are linked to heart disease. Treatment can include lifestyle changes and medications.
What is the role of ablation and device therapy in treating arrhythmias?
Ablation and device therapy, like pacemakers and ICDs, can treat certain arrhythmias. They help restore a normal heart rhythm and prevent complications.
Can lifestyle modifications help prevent or manage arrhythmias?
Yes, a healthy lifestyle can help prevent or manage arrhythmias. This includes keeping a healthy weight, exercising, reducing stress, and avoiding stimulants.
What are the symptoms of ventricular tachycardia?
Ventricular tachycardia symptoms include palpitations, dizziness, lightheadedness, and shortness of breath. If it lasts, it needs immediate medical attention.
How are bradyarrhythmias diagnosed on ECG?
Bradyarrhythmias are diagnosed on ECG by looking at the heart rate and rhythm. It checks for slow heart rates or conduction blocks to guide treatment.
References
- Mitchell, L. B., MD. (2025, February). Overview of arrhythmias and conduction disorders. In Merck Manuals Professional Edition. Retrieved from https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/abnormal-heart-rhythms/overview-of-abnormal-heart-rhythms Merck Manuals+1
- Desai, D. S., & Hajouli, S. (2023). Arrhythmias. In StatPearls [Internet]. National Library of Medicine. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK558923/ NCBI+1
- British Heart Foundation. (2022, June 1). Arrhythmias (abnormal heart rhythms). Retrieved from https://www.bhf.org.uk/informationsupport/conditions/arrhythmias British Heart Foundation
- HeartRythm.com.au. (n.d.). Normal and abnormal heart rhythms. Retrieved from https://heartrhythm.com.au/symptom/normal-and-abnormal-heart-rhythms/ Heart Rhythm Centre