After beating acute lymphoblastic leukemia, it’s key to know the signs of a possible relapse. At Liv Hospital, we help patients and their families spot early warning signs. These symptoms can be tricky to spot and might feel like the first time you got sick.
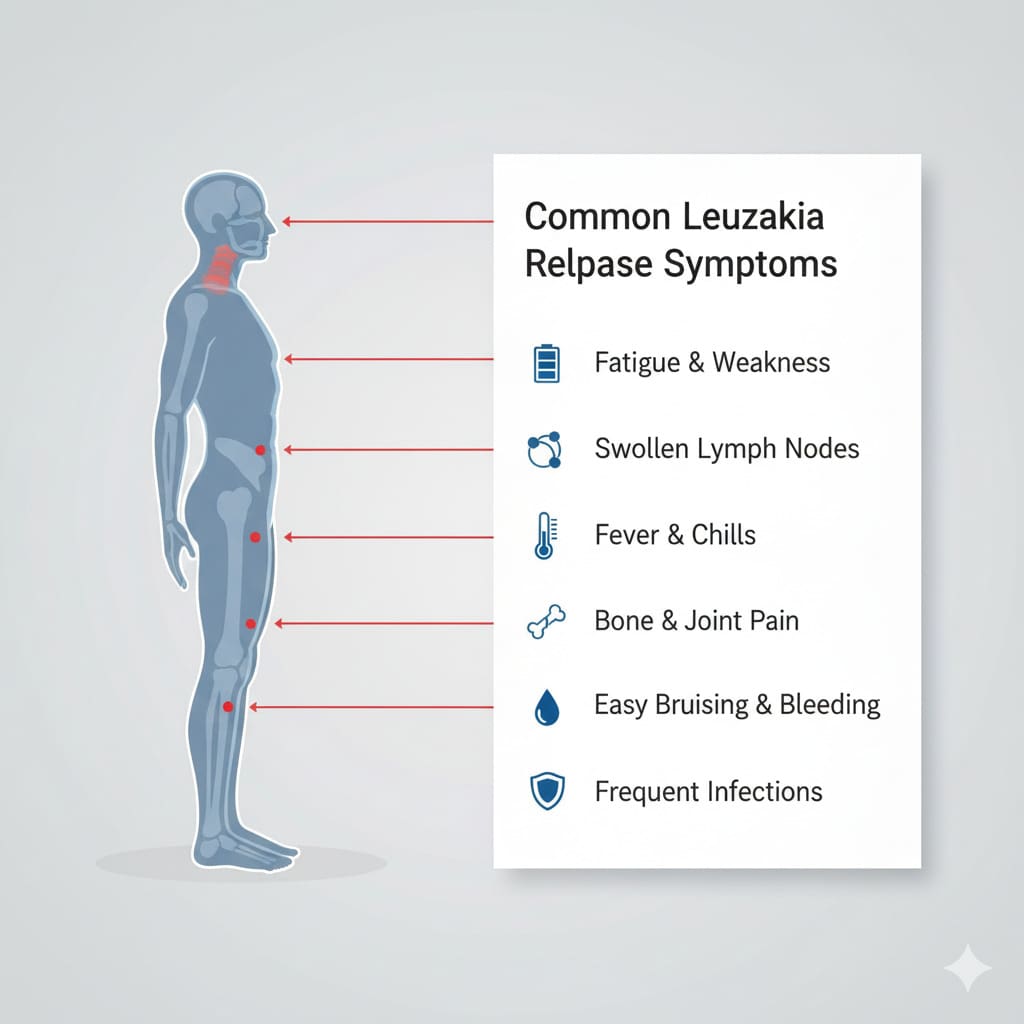
Common signs include persistent fatigue, recurrent infections, easy bleeding or bruising, fever, mouth sores, bone pain, and swollen lymph nodes. Spotting these signs early is critical for quick medical help. The chance of relapse varies, hitting 10-15% of kids and 40-50% of adults with ALL.
For leukemia patients, remission is just the start. Knowing about relapse is key to better treatment and life quality. A relapse happens when the disease comes back after a break. It’s important to understand this.
A relapse is when leukemia cells show up again in the bone marrow or blood. This happens after a patient has been in remission. It can be due to measurable residual disease (MRD), which are small leukemia cells left after treatment.
MRD testing is a big help in catching relapse early. It lets doctors act fast, which can lead to better results. Finding MRD means there’s a higher chance of relapse, so staying alert is important.
How often a relapse happens depends on the type of leukemia. For example, ALL has a higher risk in kids and some adults. CML can come back after stopping treatment. Knowing these facts helps plan better care.
Finding leukemia relapse early is key to better management and survival. Regular checks, like MRD testing and bone marrow biopsies, help catch relapse early. This makes treatment more effective.
By knowing the signs and risks of relapse, patients and doctors can plan better. This ensures quick action if the disease comes back.
Spotting leukemia relapse symptoms early can greatly help treatment. If you’ve had leukemia before, knowing the signs of relapse is key. This way, you can get medical help fast.
Leukemia relapse can show up in different ways. Physical symptoms might be fatigue, infections that keep coming back, bone pain, or easy bleeding. Laboratory findings include abnormal blood counts, like more blast cells, found in blood tests.
It’s important to keep an eye on both symptoms and lab results with your doctor. This helps catch relapse early and act quickly.
How fast symptoms show up can differ a lot. Some people might notice changes slowly over weeks or months. Others might see symptoms come on fast.
Knowing this can help spot relapse early. Always watch for any changes and tell your doctor right away.
| Symptom | Typical Timeline | Action |
|---|---|---|
| Fatigue | Weeks to months | Report persistent tiredness |
| Recurrent infections | Variable | Seek medical attention for frequent infections |
| Bleeding or bruising | Days to weeks | Report unusual bleeding or bruising |
Telling if it’s leukemia relapse or something else can be hard. Symptoms like fatigue and infections can have many causes.
Getting a detailed medical check is key. Regular check-ups and tests help find the right cause and start treatment fast.
Knowing the signs of leukemia relapse and talking to your doctor can help catch it early. This boosts your chances of getting good treatment.
When leukemia comes back, one of the first signs is often persistent fatigue. This fatigue and weakness can really affect a person’s life. It’s important to know what relapse-related fatigue looks like to catch it early.
Relapse-related fatigue is very tiredness that lasts a long time. It makes it hard to do everyday things. Unlike regular tiredness, this kind doesn’t get better with rest and can come with other symptoms like weakness and shortness of breath.
Key characteristics include:
It’s important to tell the difference between relapse-related fatigue and normal tiredness after treatment. Normal tiredness usually gets better with time. But, relapse-related fatigue gets worse and lasts longer.
| Characteristics | Relapse-Related Fatigue | Normal Recovery Tiredness |
|---|---|---|
| Duration | Persists over time | Improves over time |
| Severity | Severe, interferes with daily activities | Mild to moderate, manageable |
| Response to Rest | Not relieved by rest | Improves with rest |
If you’re feeling very tired and it’s not going away, tell your doctor. Reporting fatigue early can help get the right treatment sooner.
We recommend reporting fatigue if you experience:
A weakened immune system during leukemia relapse can cause frequent infections. It’s important to be alert. Knowing about these infections and immune system changes helps spot relapse early.
Patients with leukemia relapse face a higher risk of infections. This is because their immune system is not working well. They might get:
Some immune system changes can signal a relapse. These include:
Keeping an eye on these changes is key to catching relapse early.
Stopping infections is key in managing leukemia relapse. Ways to do this include:
Using these methods can greatly lower the chance of serious infections during relapse.
Unusual bleeding and bruising can signal leukemia relapse. We’ll look at the warning signs and how they relate to relapse.
Abnormal bleeding patterns can mean leukemia is coming back. This includes frequent nosebleeds, bleeding gums, or long bleeding after small cuts. It’s because of low platelet counts or how the platelets work.
Watching these signs closely and telling your doctor is key. For more on how leukemia affects the body, check this resource.
Easy bruising can also mean leukemia is coming back. Bruises might show up without reason or be bigger than usual. This is often because of thrombocytopenia, or low platelet count.
Keeping an eye on platelet count is key to managing bleeding risks. Regular blood tests can spot any platelet count issues early.
| Platelet Count Range | Interpretation | Recommended Action |
|---|---|---|
| Normal (150,000 – 450,000/μL) | No bleeding risk | Continue regular monitoring |
| Low (50,000 – 149,000/μL) | Moderate bleeding risk | Precautions against injury; follow-up tests |
| Very Low ( | High bleeding risk | Immediate medical attention; possible platelet transfusion |
Knowing these symptoms can help catch leukemia relapse early. Regular doctor visits are important to keep an eye on your health.
Bone and joint pain can signal leukemia coming back. It’s important for patients and doctors to watch for it. Pain can be scary, so knowing what it feels like and where it hurts is key to getting help fast.
Leukemia pain in bones and joints is different. It can hurt a lot and get worse if not treated. This pain comes from leukemia cells in the bone marrow, causing damage and swelling. Knowing this helps tell leukemia pain apart from other kinds of pain.
Leukemia pain can show up in many places. It often hurts in long bones, the spine, and pelvis. It can also affect joints like knees, hips, and shoulders. Spotting these spots can help find leukemia early.
Managing pain well is key when checking for bone and joint pain. A mix of treatments, like medicine and physical therapy, can help. Working with your doctor to find the right pain plan is important.
Knowing about leukemia pain in bones and joints helps patients get help quickly. Good pain care makes life better and helps during checks.
Fever and night sweats can be scary, and for leukemia patients, they might mean a relapse. These symptoms are worrying and very important to notice. They can tell us if leukemia is coming back.
Fever is common in leukemia patients. But some patterns can mean a higher risk of relapse. Recurrent or persistent fever and night sweats need quick medical help. We watch fever patterns closely because they can show early signs of relapse.
Here are the fever signs that might mean relapse:
Night sweats are another symptom that can mean leukemia is coming back. Night sweats are different from normal sweating. They are very wet and happen even when it’s cool. We see night sweats as a sign the body is fighting the disease. If you have night sweats and fever, it’s very important to get checked.
Leukemia patients need to know when to get medical help fast. If you have a fever over 38 °C (100.4 °F) that won’t go away or with other bad symptoms, call your doctor right away. We stress the need for quick medical checks to catch relapse early.
Here are times when you should get medical help right away:
Leukemia relapse can show up as swollen lymph nodes and bigger organs. It’s key to check yourself often. We’ll show you what to look for and why it matters.
Checking your lymph nodes regularly is a big step in catching leukemia relapse early. These small, bean-shaped bodies are part of your lymphatic system. Here’s how to check them:
Finding lymph node changes early can really help with treatment. A top hematologist says, “Watching for swelling in lymph nodes is a key sign of leukemia coming back.”
“The lymph nodes are often the first place where leukemia cells gather, making them a key sign of possible relapse.”
Getting bigger spleen or liver can mean leukemia is coming back. This happens when leukemia cells build up in these organs.
| Organ | Symptoms of Enlargement | Potential Complications |
|---|---|---|
| Spleen | Discomfort or pain in the upper left abdomen, feeling full quickly | Rupture, infection, anemia |
| Liver | Discomfort or pain in the upper right abdomen, jaundice | Liver dysfunction, coagulopathy |
Other signs might also show leukemia relapse. These include:
It’s important to watch for these signs and tell your doctor right away.
Knowing these signs and checking yourself often can help you catch leukemia relapse early. This way, you can stay on top of your health.
Leukaemia relapse shows up differently in kids, adults, and the elderly. It’s important to know these differences to catch it early and treat it right.
In kids, leukaemia relapse can look like the first time. Look out for:
Kids might also act differently, like being really tired or moody. It’s key for parents and caregivers to watch for these signs and tell the doctor fast.
In adults, leukaemia relapse can be tricky to spot. It might look like other health issues. Adults might notice:
Adults should tell their doctors if they notice these signs, even more so if they’ve had leukaemia before.
Older patients face extra challenges because of other health issues and aging. Symptoms like tiredness, weakness, and infections can mean many things. It’s very important to think about leukaemia relapse.
| Age Group | Common Relapse Symptoms | Special Considerations |
|---|---|---|
| Pediatric | Bone and joint pain, lymph node swelling, spleen or liver enlargement | Behavioral changes, irritability |
| Adult | Unexplained weight loss, night sweats, recurrent infections | Symptoms can be subtle, resembling other conditions |
| Elderly | Fatigue, weakness, recurrent infections | Comorbid conditions, age-related decline |
Knowing how leukaemia relapse looks in different ages is key. It helps everyone spot it early and start treatment fast.
After remission, it’s key to keep checking on patients. This helps catch any signs of relapse early. We make sure patients get regular tests and visits.
MRD testing finds tiny leukemia cells left behind. It’s important for knowing the risk of relapse and planning treatment.
MRD testing looks at bone marrow samples with advanced methods like PCR or flow cytometry. It shows how well treatment worked and if relapse is likely.
Regular blood tests check blood cell counts and look for odd results. We use these to spot early signs of relapse.
Important blood work includes:
Imaging and bone marrow tests give us important info on leukemia cells in the body.
Bone marrow biopsies and scans like CT or PET help us see how much disease is there and watch for relapse signs.
Sticking to a follow-up plan is key for good monitoring. Here’s a basic guide:
| Time After Remission | Tests and Evaluations | Frequency |
|---|---|---|
| 0-6 months | MRD testing, Blood work | Monthly |
| 6-12 months | Blood work, Bone marrow biopsy | Every 2-3 months |
| 1-2 years | Imaging studies, Blood work | Every 3-6 months |
By sticking to this monitoring plan, we can catch relapse early. Regular visits and tests are key to good leukemia care.
Leukemia relapse risk comes from many factors. These include genetics, molecular changes, and clinical aspects. Knowing these factors helps in managing and preventing relapse.
Genetic and molecular changes are key in leukemia relapse. Certain genetic mutations can increase the risk of relapse. For example, some chromosomal changes make leukemia cells harder to treat.
We watch patients with these high-risk genetic features closely. This helps us adjust their treatment plans.
Molecular risk factors like minimal residual disease (MRD) status are also important. Patients with detectable MRD after treatment face a higher risk of relapse. They might need more intense follow-up and treatment changes.
How well a patient responds to initial treatment is a big indicator of relapse risk. Achieving complete remission is the main goal of treatment. But, the speed and depth of response vary among patients.
Patients who respond quickly and have low MRD levels usually have a better outlook. On the other hand, slow response or high MRD levels suggest a higher risk of relapse. This might mean closer monitoring and more aggressive treatment.
Age at diagnosis is a significant factor in relapse risk. Older adults often face a higher risk due to less tolerance to chemotherapy and more health issues. Younger patients, including children, generally have a better prognosis, but it depends on the leukemia subtype.
The type of leukemia also affects relapse risk. For example, acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) have different risk factors. Within ALL, B-Cell ALL has specific risk profiles that influence treatment choices.
B-Cell ALL is common in children. Certain genetic abnormalities, like the Philadelphia chromosome, can raise the risk of relapse. Patients with these high-risk features might benefit from targeted therapies along with standard chemotherapy.
We also look at the patient’s response to initial treatment and MRD levels when assessing B-Cell ALL relapse risk. Understanding these factors helps us tailor treatment plans to improve outcomes for these patients.
When leukemia relapse is suspected, quick action is key. We’ve talked about symptoms like fatigue, infections, bleeding, and bone pain. Knowing these signs and risk factors helps catch relapse early.
Patients and doctors need to watch for these symptoms closely. Regular check-ups, MRD tests, and blood work help spot relapse early. Being alert and proactive can greatly improve patient outcomes.
Managing leukemia relapse well needs fast action and a solid treatment plan. It’s vital for patients and healthcare teams to work together. By understanding symptoms and warning signs, patients can play a big role in their care. This leads to better health results.
Symptoms of leukemia relapse include fatigue and infections that keep coming back. You might also notice easy bleeding, fever, mouth sores, bone pain, and swollen lymph nodes. These signs can be similar to when you were first diagnosed.
Doctors use physical checks, lab tests, and imaging to find leukemia relapse. A key test is measurable residual disease (MRD) testing. It helps spot small leukemia cells early, so treatment can start sooner.
Feeling very tired or weak is often the first sign of leukemia coming back. If you’re too tired to do daily things, it could mean relapse. Telling your doctor right away is important.
People with relapse get sick more easily. To stay safe, it’s important to know about common infections and how to avoid them. Taking steps to prevent infections is key.
If your platelets are low, you might bleed or bruise easily. Checking your platelet count regularly is important. This helps catch problems early and manage them better.
It’s important to know how leukemia relapse shows up in kids, adults, and older people. Each group has different signs. Knowing these helps doctors treat each patient better.
MRD testing finds small leukemia cells left after treatment. It’s a big help in catching relapse early. This way, doctors can start treatment sooner and improve chances of success.
Several things can increase the chance of leukemia coming back. These include genetic and molecular factors, how well you respond to treatment, your age, and the type of leukemia. Knowing these helps doctors plan better care and watch for signs of relapse.
If you think you might be relapsing, it’s important to act fast. Know the signs, understand the risks, and know what to do. Working with your doctor is key to catching and managing relapse early.
After treatment, it’s vital to keep an eye out for relapse. Regular blood tests, imaging, and bone marrow checks are important. They help find problems early, so treatment can start right away.
Healthline: Relapse of Acute Lymphoblastic Leukemia
Medical News Today: Can Leukemia Come Back After 20 Years?
Leukaemia Care: Relapsed and Refractory Acute Lymphoblastic Leukaemia (ALL)
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us