Last Updated on November 18, 2025 by Ugurkan Demir

Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of two or more cervical vertebrae. This condition can severely restrict neck movement and sometimes give the appearance of being born with a short neck. We are dedicated to providing expert care for individuals affected by this condition.
Recent studies suggest that KFS may be more prevalent than previously thought, with some estimates as high as 1 in 172 births. At Liv Hospital, we understand the importance of comprehensive care for patients with congenital spine fusion.
Key Takeaways
- Klippel-Feil syndrome is a congenital disorder that affects cervical vertebrae.
- The condition can cause restricted neck movement.
- KFS may be more prevalent than previously estimated.
- Expert care is crucial for managing the condition.
- Liv Hospital provides compassionate and comprehensive care for KFS patients.
What Causes Fused Vertebrae in the Neck

Understanding the causes of fused vertebrae in the neck is crucial for diagnosing and managing conditions like Klippel-Feil Syndrome. Fused vertebrae can result from a combination of genetic, environmental, and developmental factors.
Congenital vs. Acquired Causes
Fused vertebrae in the neck can be either congenital or acquired. Congenital fusions occur during embryonic development, while acquired fusions result from trauma, infection, or other pathological processes. Klippel-Feil Syndrome is a significant congenital condition characterized by the fusion of cervical vertebrae.
The Role of Embryonic Development
Research indicates that Klippel-Feil Syndrome occurs due to a failure in the normal segmentation of cervical mesodermal somites during embryonic development. This failure leads to the abnormal fusion of vertebrae. Understanding embryonic development is crucial for grasping the underlying causes of congenital spinal anomalies.
Genetic Factors in Vertebral Fusion
Genetic factors play a significant role in the development of Klippel-Feil Syndrome and other congenital spinal anomalies. Studies have identified several genes associated with vertebral segmentation and development. These genetic factors can influence the severity and presentation of the condition.
Understanding Klippel-Feil Syndrome: A Rare Congenital Disorder

Understanding Klippel-Feil syndrome requires a deep dive into its historical background, clinical features, and the various types that have been identified over the years. Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of any two of the seven cervical vertebrae.
Historical Background and Discovery
Klippel-Feil syndrome was first described by Maurice Klippel and André Feil in 1912. Their pioneering work laid the foundation for our current understanding of this complex condition. As Klippel and Feil noted, the syndrome is often associated with other skeletal, renal, auditory, and cardiac anomalies, highlighting its multifaceted nature.
“The presence of fused cervical vertebrae in KFS patients is just one aspect of a broader spectrum of potential abnormalities,” as emphasized by later studies. This understanding has been crucial in shaping the diagnostic and treatment approaches for KFS.
Defining Characteristics of KFS
KFS is characterized by its classic triad: short neck appearance, low posterior hairline, and limited neck mobility. However, not all patients exhibit all three features, and the severity can vary widely. The condition is often associated with other congenital anomalies, making a comprehensive evaluation crucial.
Types and Classifications
KFS can be classified into three main types based on the extent of cervical spine involvement and associated anomalies. Type I involves a single fusion level, Type II involves multiple non-contiguous fusion levels, and Type III includes both cervical spine fusions and lower thoracic or lumbar spine anomalies. Understanding these classifications is essential for determining the prognosis and appropriate management strategy.
As we continue to explore KFS, it becomes clear that this condition is more than just a simple congenital anomaly; it’s a complex disorder that requires a multidisciplinary approach to management.
The Classic Triad: Key Clinical Features of KFS
Understanding the clinical manifestations of Klippel-Feil Syndrome is crucial for accurate diagnosis and management. The classic triad associated with KFS includes a short neck appearance, low posterior hairline, and limited neck mobility. These features are not only distinctive but also critical for the diagnosis of this rare congenital disorder.
Short Neck Appearance
One of the hallmark features of Klippel-Feil Syndrome is the appearance of a short neck. This is due to the congenital fusion of any two of the seven cervical vertebrae. The fusion can occur at various levels and can lead to a significant reduction in neck length. The short neck appearance is often one of the first signs that lead to further investigation and diagnosis of KFS.
Low Posterior Hairline
Another characteristic feature of KFS is a low posterior hairline. This occurs when the hairline extends further down the back than usual, giving the appearance of a lower hairline at the back of the head. This feature, while not exclusive to KFS, is a significant indicator when considered alongside other symptoms.
Limited Neck Mobility
Limited neck mobility is a critical clinical feature of Klippel-Feil Syndrome. The fusion of cervical vertebrae restricts the normal range of motion of the neck, leading to reduced flexibility. This limitation can vary in severity depending on the extent and level of vertebral fusion.
| Clinical Feature | Description | Significance in KFS Diagnosis |
|---|---|---|
| Short Neck Appearance | Congenital fusion of cervical vertebrae leading to reduced neck length | One of the primary signs leading to KFS diagnosis |
| Low Posterior Hairline | Hairline extends further down the back than usual | Significant indicator when considered with other symptoms |
| Limited Neck Mobility | Restriction in neck movement due to vertebral fusion | Critical feature varying in severity based on fusion extent |
Not all patients with KFS display the entire classic triad, but these features are crucial for diagnosis. The presence and severity of these characteristics can vary widely among individuals, making a comprehensive evaluation essential for accurate diagnosis.
“The classic triad of Klippel-Feil Syndrome, while not present in all cases, remains a cornerstone in the diagnosis of this complex condition.”
Prevalence and Demographics of Klippel-Feil Syndrome
Recent research has shed new light on the prevalence of Klippel-Feil Syndrome, challenging historical estimates. As we delve into the demographics of this rare congenital disorder, it becomes clear that our understanding of its prevalence has evolved significantly over time.
Historical Estimates
Historically, Klippel-Feil Syndrome was considered to be extremely rare, with estimates ranging from 1 in 40,000 to 1 in 50,000 live births. These figures were based on early clinical observations and limited population studies.
Current Understanding
More recent studies suggest that Klippel-Feil Syndrome may be more common than initially thought. Some research indicates a prevalence as high as 1.2% in certain populations, although this figure may include asymptomatic cases or those with mild symptoms that were previously undiagnosed.
Gender Distribution and Risk Factors
Research into the gender distribution of Klippel-Feil Syndrome has yielded mixed results, with some studies suggesting a slight female predominance, while others find no significant gender difference. Understanding these demographics is crucial for identifying potential risk factors and improving diagnosis.
| Demographic Characteristic | Historical Data | Current Understanding |
|---|---|---|
| Prevalence | 1 in 40,000 to 1 in 50,000 | Up to 1.2% in some populations |
| Gender Distribution | Mixed results | Slight female predominance in some studies |
| Risk Factors | Limited understanding | Genetic factors, family history |
As we continue to refine our understanding of Klippel-Feil Syndrome, it’s clear that both historical estimates and current research play crucial roles in shaping our knowledge. Further studies are needed to fully elucidate the prevalence, demographics, and risk factors associated with this complex condition.
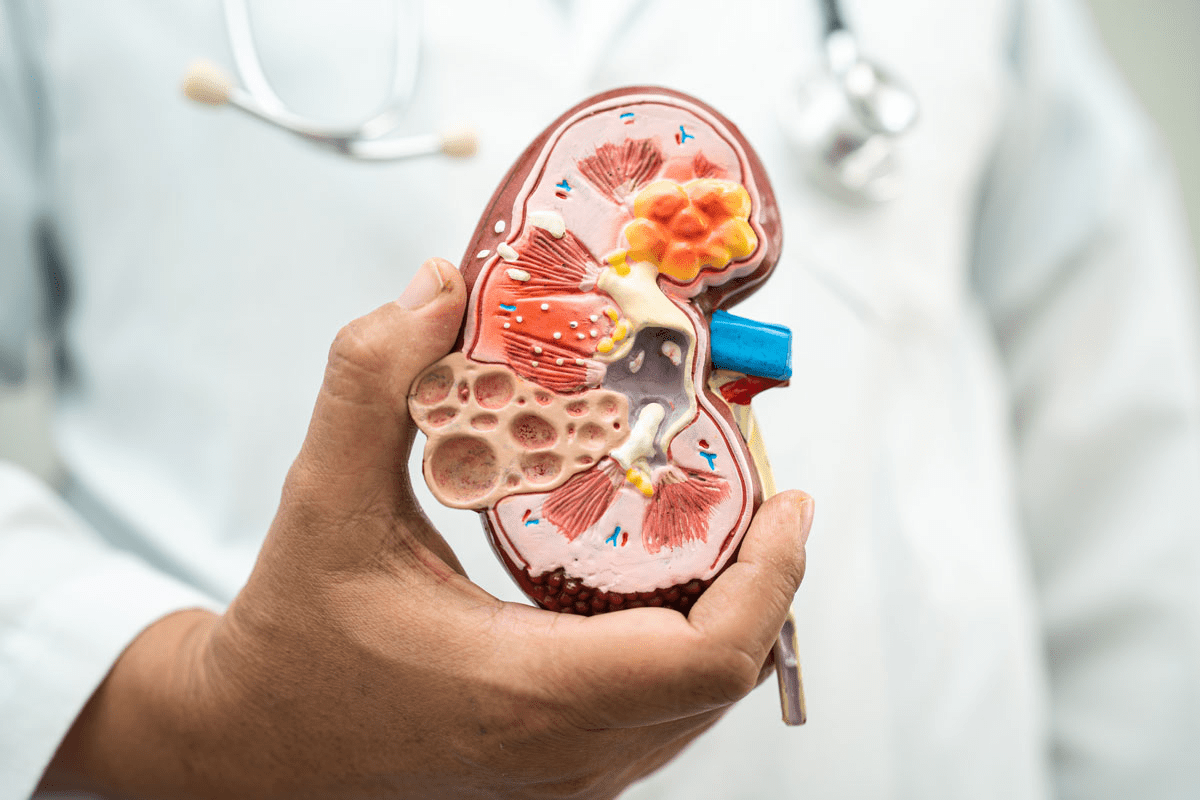
Common Locations of Fused Vertebrae in Neck
Fused vertebrae in the neck can occur at various levels, but some locations are more common than others in patients with Klippel-Feil Syndrome (KFS). Understanding these common fusion sites is crucial for diagnosing and managing the condition effectively.
C2-C3 Vertebral Fusion Patterns
The fusion of the C2 and C3 vertebrae is one of the most frequently observed patterns in KFS patients. This specific fusion can lead to a reduction in neck mobility and may contribute to the characteristic short neck appearance associated with the syndrome. Early detection through imaging studies is essential for proper management.
C5-C6 Vertebral Fusion Characteristics
Another common site for vertebral fusion in KFS is between the C5 and C6 vertebrae. This fusion can result in altered biomechanics of the cervical spine, potentially leading to increased stress on adjacent vertebrae. Regular monitoring is necessary to prevent complications.
Multiple Level Fusions and Their Implications
Multiple level fusions, where more than two vertebrae are fused together, can lead to more severe symptoms and complications in KFS patients. These can include increased risk of spinal instability, neurological issues, and restricted mobility. A comprehensive treatment plan is vital for managing these complex cases.
| Location of Fusion | Common Symptoms | Potential Complications |
|---|---|---|
| C2-C3 | Reduced neck mobility, short neck appearance | Spinal instability, neurological issues |
| C5-C6 | Altered cervical biomechanics, stress on adjacent vertebrae | Increased risk of degenerative changes |
| Multiple Levels | Severe restriction of mobility, complex spinal deformities | Neurological complications, significant spinal instability |
Understanding the specific locations and patterns of fused vertebrae in KFS is crucial for developing effective treatment strategies. By identifying the most common fusion sites and their implications, healthcare providers can offer targeted care to improve patient outcomes.
Diagnostic Approaches for Identifying Fused Vertebrae
Diagnosing fused vertebrae requires a comprehensive approach that combines clinical examination techniques with advanced imaging studies. We use a variety of methods to accurately identify and assess the extent of vertebral fusion.
Clinical Examination Techniques
A thorough clinical examination is the first step in diagnosing fused vertebrae. We assess neck mobility, looking for limitations in range of motion that may indicate fusion. We also examine the patient’s posture and look for any visible signs of spinal deformity. Clinical evaluation helps us identify potential neurological deficits and assess the overall impact of fused vertebrae on the patient’s quality of life.
During the examination, we pay particular attention to the classic triad associated with Klippel-Feil Syndrome: short neck appearance, low posterior hairline, and limited neck mobility. While not all patients exhibit all three features, their presence can guide our diagnostic process.
Imaging Studies: X-rays, CT, and MRI
Imaging studies are crucial for confirming the diagnosis of fused vertebrae and assessing the extent of fusion. We typically begin with X-rays, which provide a preliminary view of the spine and can reveal obvious fusions or other bony abnormalities.
For more detailed imaging, we often use Computed Tomography (CT) scans. CT scans offer a clearer picture of the bony structures, allowing us to assess the extent of fusion and identify any associated anomalies.
Magnetic Resonance Imaging (MRI) is particularly valuable for evaluating the soft tissues surrounding the spine, including the spinal cord and nerve roots. MRI helps us identify any neurological complications associated with fused vertebrae.
Genetic Testing Options
In cases where Klippel-Feil Syndrome is suspected, we may recommend genetic testing. While there is no single “KFS gene,” mutations in certain genes, such as GDF6 and GDF3, have been associated with the condition. Genetic testing can help confirm the diagnosis and provide information about the risk of passing the condition to offspring.
We discuss the benefits and limitations of genetic testing with our patients, ensuring they are fully informed about the process and its potential outcomes.
Potential Complications of Klippel-Feil Syndrome
Patients with Klippel-Feil Syndrome (KFS) are at risk for various complications, making comprehensive care essential. KFS is a complex condition characterized by the congenital fusion of any two of the seven cervical vertebrae. This fusion can lead to a range of issues, from mild discomfort to severe neurological problems.
Neurological Complications
One of the most significant concerns for individuals with KFS is the risk of neurological complications. The abnormal fusion of vertebrae can lead to spinal cord compression, resulting in symptoms such as pain, numbness, and weakness in the limbs. In severe cases, this compression can cause more severe neurological deficits, including paralysis.
According to a study published in the European Spine Jvournal, patients with KFS are at an increased risk of neurological complications due to the instability of the cervical spine. This instability can lead to degenerative changes and potentially severe neurological consequences.
Spinal Instability Risks
Spinal instability is another significant risk associated with KFS. The fusion of vertebrae can alter the normal biomechanics of the spine, leading to increased stress on the surrounding vertebrae and discs. This stress can result in degenerative changes, such as disc degeneration and osteoarthritis, which can further exacerbate spinal instability.
As noted by experts, “The presence of KFS increases the risk of spinal instability, which can lead to a range of complications, including neurological deterioration.” Therefore, monitoring and managing spinal instability is crucial in the care of patients with KFS.
Associated Systemic Conditions
KFS is often associated with various systemic conditions, including renal and cardiac anomalies. Studies have shown that individuals with KFS are at a higher risk of having congenital anomalies in other systems, emphasizing the need for comprehensive evaluation and management.
A thorough assessment is necessary to identify any associated conditions early, allowing for timely intervention. As we understand more about KFS, it becomes clear that a multidisciplinary approach is essential in managing the condition and its complications.
Risk Factors for Requiring Surgical Intervention
Certain factors increase the likelihood of requiring surgical intervention in patients with Klippel-Feil Syndrome (KFS). Understanding these risk factors is crucial for effective management and treatment planning.
Gender-Related Risk Factors
Research has shown that gender can play a role in the likelihood of requiring surgical intervention for KFS patients. Studies indicate that females may be more likely to require surgery due to the nature of their spinal abnormalities. We will examine the specific gender-related risk factors in detail.
| Gender | Surgical Intervention Rate | Common Complications |
|---|---|---|
| Male | 35% | Spinal instability, neurological symptoms |
| Female | 45% | Neurological progression, chronic pain |
Degree of Spinal Instability
The degree of spinal instability is a significant risk factor for requiring surgical intervention in KFS patients. Patients with more pronounced spinal instability are at a higher risk of neurological complications. We assess the degree of instability through advanced imaging techniques.
Neurological Symptom Progression
The progression of neurological symptoms is another critical factor that may necessitate surgical intervention. Patients experiencing rapid progression of neurological symptoms are more likely to require surgery to prevent further deterioration.
Pain and Quality of Life Considerations
Pain management and quality of life are essential considerations when evaluating the need for surgical intervention. Surgical options are often considered when conservative management fails to alleviate pain and improve quality of life. We work closely with patients to understand their specific needs and develop a personalized treatment plan.
Treatment Options for Fused Vertebrae and KFS
The management of fused vertebrae and Klippel-Feil Syndrome (KFS) requires a multifaceted approach. We recognize that each patient’s condition is unique, and therefore, treatment plans are tailored to address specific needs and symptoms.
Conservative Management Approaches
For many patients with KFS, conservative management is the initial treatment strategy. This approach includes physical therapy to improve neck mobility and strength, as well as pain management techniques to address discomfort associated with the condition.
We also recommend regular monitoring to assess the progression of the condition and adjust the treatment plan as necessary.
Surgical Techniques and Considerations
In more severe cases of KFS, or when conservative management is insufficient, surgical intervention may be necessary. Surgical techniques can vary depending on the specific characteristics of the condition, such as the location and extent of vertebral fusion.
We consider factors such as the patient’s overall health, the presence of neurological symptoms, and the degree of spinal instability when determining the need for surgical intervention.
Rehabilitation Strategies
Following surgical treatment, or as part of conservative management, rehabilitation strategies play a crucial role in helping patients regain optimal function and manage symptoms. These strategies may include physical therapy, occupational therapy, and lifestyle modifications.
Our team works closely with patients to develop personalized rehabilitation plans that address their unique needs and goals.
Living with Klippel-Feil Syndrome: Daily Challenges and Adaptations
Living with KFS involves navigating a range of daily difficulties that can impact various aspects of life. Individuals with this condition often need to make significant adaptations to manage their symptoms effectively and maintain a good quality of life.
Physical Activity Modifications
One of the primary challenges for individuals with KFS is modifying their physical activities to accommodate their condition. High-impact exercises and contact sports are generally discouraged due to the risk of injury and exacerbating spinal instability. Instead, patients are often advised to engage in low-impact activities such as swimming or cycling, which can help maintain cardiovascular fitness without putting excessive strain on the neck.
It’s also important for individuals with KFS to consult with healthcare professionals to develop a personalized exercise plan that takes into account their specific condition and limitations.
Ergonomic Considerations
Ergonomic adjustments are crucial for individuals with KFS to reduce discomfort and prevent further complications. This includes using ergonomic furniture and equipment that supports proper posture and reduces strain on the neck and spine.
- Adjusting workstations to promote good posture
- Using supportive pillows and mattresses
- Avoiding heavy lifting or bending
Psychosocial Support Resources
Living with KFS can have a significant psychosocial impact, affecting an individual’s mental health and social interactions. Access to psychosocial support resources is vital for managing the emotional and psychological aspects of the condition.
Educational and Workplace Accommodations
Individuals with KFS may require specific accommodations in educational and workplace settings to ensure their comfort and productivity. This can include modifications to their workspace, flexible scheduling, and the provision of necessary assistive devices.
By understanding the daily challenges associated with KFS and implementing appropriate adaptations, individuals with this condition can lead fulfilling lives. It’s essential for patients, families, and healthcare providers to work together to develop comprehensive management plans that address the unique needs of each individual.
Conclusion: Advances in Understanding and Managing Fused Vertebrae
Advances in diagnosis and treatment have significantly improved the management of Klippel-Feil Syndrome (KFS). Ongoing research continues to enhance our understanding of fused vertebrae and KFS, leading to better patient outcomes. We have seen significant progress in fused vertebrae understanding, allowing for more effective managing of fused vertebrae.
The complexity of KFS requires a comprehensive approach to care, incorporating advances in KFS management. By combining clinical expertise with cutting-edge technology, we can provide personalized treatment plans that address the unique needs of each patient. This integrated approach enables us to improve the quality of life for individuals living with KFS.
As we continue to advance our understanding of KFS, we remain committed to providing world-class healthcare with complete support for international patients. Our goal is to empower patients with the knowledge and resources they need to navigate their condition, ensuring they receive the best possible care.
FAQ
What is Klippel-Feil syndrome?
Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of two or more cervical vertebrae, which can lead to limited neck mobility and other associated complications.
What causes fused vertebrae in the neck?
Fused vertebrae in the neck are often caused by congenital factors related to embryonic development, with genetic factors playing a significant role in the development of Klippel-Feil syndrome.
What are the classic symptoms of Klippel-Feil syndrome?
The classic triad of KFS includes a short neck appearance, low posterior hairline, and limited neck mobility, which are key clinical features used in diagnosis.
How common is Klippel-Feil syndrome?
Recent studies suggest that KFS may be more prevalent than previously thought, with estimates as high as 1 in 172 births, although historical estimates ranged from 1 in 40,000 to 1 in 50,000.
What are the potential complications of Klippel-Feil syndrome?
Potential complications of KFS include neurological complications, risks of spinal instability, and associated systemic conditions, which can significantly impact the quality of life for individuals with the condition.
How is Klippel-Feil syndrome diagnosed?
Diagnosis of KFS involves clinical examination techniques, imaging studies such as X-rays, CT, and MRI, and genetic testing options to identify the presence and extent of vertebral fusion.
What are the treatment options for fused vertebrae and KFS?
Treatment options for fused vertebrae and KFS include conservative management approaches, surgical techniques, and rehabilitation strategies, which are tailored to the individual’s specific needs and the severity of their condition.
When is surgical intervention necessary for KFS patients?
Surgical intervention is considered necessary for KFS patients when there are significant risk factors such as gender-related factors, degree of spinal instability, and progression of neurological symptoms.
How can individuals with KFS adapt to daily challenges?
Individuals with KFS can adapt to daily challenges by making physical activity modifications, considering ergonomic adjustments, and accessing psychosocial support resources to manage their condition effectively.
What is the prognosis for individuals with Klippel-Feil syndrome?
The prognosis for individuals with KFS varies depending on the severity of their condition and the presence of associated complications, but with proper management and care, many individuals can lead active and fulfilling lives.
What is Klippel-Feil syndrome?
Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of two or more cervical vertebrae, which can lead to limited neck mobility and other associated complications.
What causes fused vertebrae in the neck?
Fused vertebrae in the neck are often caused by congenital factors related to embryonic development, with genetic factors playing a significant role in the development of Klippel-Feil syndrome.
What are the classic symptoms of Klippel-Feil syndrome?
The classic triad of KFS includes a short neck appearance, low posterior hairline, and limited neck mobility, which are key clinical features used in diagnosis.
How common is Klippel-Feil syndrome?
Recent studies suggest that KFS may be more prevalent than previously thought, with estimates as high as 1 in 172 births, although historical estimates ranged from 1 in 40,000 to 1 in 50,000.
What are the potential complications of Klippel-Feil syndrome?
Potential complications of KFS include neurological complications, risks of spinal instability, and associated systemic conditions, which can significantly impact the quality of life for individuals with the condition.
How is Klippel-Feil syndrome diagnosed?
Diagnosis of KFS involves clinical examination techniques, imaging studies such as X-rays, CT, and MRI, and genetic testing options to identify the presence and extent of vertebral fusion.
What are the treatment options for fused vertebrae and KFS?
Treatment options for fused vertebrae and KFS include conservative management approaches, surgical techniques, and rehabilitation strategies, which are tailored to the individual’s specific needs and the severity of their condition.
When is surgical intervention necessary for KFS patients?
Surgical intervention is considered necessary for KFS patients when there are significant risk factors such as gender-related factors, degree of spinal instability, and progression of neurological symptoms.
How can individuals with KFS adapt to daily challenges?
Individuals with KFS can adapt to daily challenges by making physical activity modifications, considering ergonomic adjustments, and accessing psychosocial support resources to manage their condition effectively.
What is the prognosis for individuals with Klippel-Feil syndrome?
The prognosis for individuals with KFS varies depending on the severity of their condition and the presence of associated complications, but with proper management and care, many individuals can lead active and fulfilling lives.

Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of two or more cervical vertebrae. This condition can severely restrict neck movement and sometimes give the appearance of being born with a short neck. We are dedicated to providing expert care for individuals affected by this condition.
Recent studies suggest that KFS may be more prevalent than previously thought, with some estimates as high as 1 in 172 births. At Liv Hospital, we understand the importance of comprehensive care for patients with congenital spine fusion.
Key Takeaways
- Klippel-Feil syndrome is a congenital disorder that affects cervical vertebrae.
- The condition can cause restricted neck movement.
- KFS may be more prevalent than previously estimated.
- Expert care is crucial for managing the condition.
- Liv Hospital provides compassionate and comprehensive care for KFS patients.
What Causes Fused Vertebrae in the Neck

Understanding the causes of fused vertebrae in the neck is crucial for diagnosing and managing conditions like Klippel-Feil Syndrome. Fused vertebrae can result from a combination of genetic, environmental, and developmental factors.
Congenital vs. Acquired Causes
Fused vertebrae in the neck can be either congenital or acquired. Congenital fusions occur during embryonic development, while acquired fusions result from trauma, infection, or other pathological processes. Klippel-Feil Syndrome is a significant congenital condition characterized by the fusion of cervical vertebrae.
The Role of Embryonic Development
Research indicates that Klippel-Feil Syndrome occurs due to a failure in the normal segmentation of cervical mesodermal somites during embryonic development. This failure leads to the abnormal fusion of vertebrae. Understanding embryonic development is crucial for grasping the underlying causes of congenital spinal anomalies.
Genetic Factors in Vertebral Fusion
Genetic factors play a significant role in the development of Klippel-Feil Syndrome and other congenital spinal anomalies. Studies have identified several genes associated with vertebral segmentation and development. These genetic factors can influence the severity and presentation of the condition.
Understanding Klippel-Feil Syndrome: A Rare Congenital Disorder

Understanding Klippel-Feil syndrome requires a deep dive into its historical background, clinical features, and the various types that have been identified over the years. Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of any two of the seven cervical vertebrae.
Historical Background and Discovery
Klippel-Feil syndrome was first described by Maurice Klippel and André Feil in 1912. Their pioneering work laid the foundation for our current understanding of this complex condition. As Klippel and Feil noted, the syndrome is often associated with other skeletal, renal, auditory, and cardiac anomalies, highlighting its multifaceted nature.
“The presence of fused cervical vertebrae in KFS patients is just one aspect of a broader spectrum of potential abnormalities,” as emphasized by later studies. This understanding has been crucial in shaping the diagnostic and treatment approaches for KFS.
Defining Characteristics of KFS
KFS is characterized by its classic triad: short neck appearance, low posterior hairline, and limited neck mobility. However, not all patients exhibit all three features, and the severity can vary widely. The condition is often associated with other congenital anomalies, making a comprehensive evaluation crucial.
Types and Classifications
KFS can be classified into three main types based on the extent of cervical spine involvement and associated anomalies. Type I involves a single fusion level, Type II involves multiple non-contiguous fusion levels, and Type III includes both cervical spine fusions and lower thoracic or lumbar spine anomalies. Understanding these classifications is essential for determining the prognosis and appropriate management strategy.
As we continue to explore KFS, it becomes clear that this condition is more than just a simple congenital anomaly; it’s a complex disorder that requires a multidisciplinary approach to management.
The Classic Triad: Key Clinical Features of KFS
Understanding the clinical manifestations of Klippel-Feil Syndrome is crucial for accurate diagnosis and management. The classic triad associated with KFS includes a short neck appearance, low posterior hairline, and limited neck mobility. These features are not only distinctive but also critical for the diagnosis of this rare congenital disorder.
Short Neck Appearance
One of the hallmark features of Klippel-Feil Syndrome is the appearance of a short neck. This is due to the congenital fusion of any two of the seven cervical vertebrae. The fusion can occur at various levels and can lead to a significant reduction in neck length. The short neck appearance is often one of the first signs that lead to further investigation and diagnosis of KFS.
Low Posterior Hairline
Another characteristic feature of KFS is a low posterior hairline. This occurs when the hairline extends further down the back than usual, giving the appearance of a lower hairline at the back of the head. This feature, while not exclusive to KFS, is a significant indicator when considered alongside other symptoms.
Limited Neck Mobility
Limited neck mobility is a critical clinical feature of Klippel-Feil Syndrome. The fusion of cervical vertebrae restricts the normal range of motion of the neck, leading to reduced flexibility. This limitation can vary in severity depending on the extent and level of vertebral fusion.
| Clinical Feature | Description | Significance in KFS Diagnosis |
|---|---|---|
| Short Neck Appearance | Congenital fusion of cervical vertebrae leading to reduced neck length | One of the primary signs leading to KFS diagnosis |
| Low Posterior Hairline | Hairline extends further down the back than usual | Significant indicator when considered with other symptoms |
| Limited Neck Mobility | Restriction in neck movement due to vertebral fusion | Critical feature varying in severity based on fusion extent |
Not all patients with KFS display the entire classic triad, but these features are crucial for diagnosis. The presence and severity of these characteristics can vary widely among individuals, making a comprehensive evaluation essential for accurate diagnosis.
“The classic triad of Klippel-Feil Syndrome, while not present in all cases, remains a cornerstone in the diagnosis of this complex condition.”
Prevalence and Demographics of Klippel-Feil Syndrome
Recent research has shed new light on the prevalence of Klippel-Feil Syndrome, challenging historical estimates. As we delve into the demographics of this rare congenital disorder, it becomes clear that our understanding of its prevalence has evolved significantly over time.
Historical Estimates
Historically, Klippel-Feil Syndrome was considered to be extremely rare, with estimates ranging from 1 in 40,000 to 1 in 50,000 live births. These figures were based on early clinical observations and limited population studies.
Current Understanding
More recent studies suggest that Klippel-Feil Syndrome may be more common than initially thought. Some research indicates a prevalence as high as 1.2% in certain populations, although this figure may include asymptomatic cases or those with mild symptoms that were previously undiagnosed.
Gender Distribution and Risk Factors
Research into the gender distribution of Klippel-Feil Syndrome has yielded mixed results, with some studies suggesting a slight female predominance, while others find no significant gender difference. Understanding these demographics is crucial for identifying potential risk factors and improving diagnosis.
| Demographic Characteristic | Historical Data | Current Understanding |
|---|---|---|
| Prevalence | 1 in 40,000 to 1 in 50,000 | Up to 1.2% in some populations |
| Gender Distribution | Mixed results | Slight female predominance in some studies |
| Risk Factors | Limited understanding | Genetic factors, family history |
As we continue to refine our understanding of Klippel-Feil Syndrome, it’s clear that both historical estimates and current research play crucial roles in shaping our knowledge. Further studies are needed to fully elucidate the prevalence, demographics, and risk factors associated with this complex condition.
Common Locations of Fused Vertebrae in Neck
Fused vertebrae in the neck can occur at various levels, but some locations are more common than others in patients with Klippel-Feil Syndrome (KFS). Understanding these common fusion sites is crucial for diagnosing and managing the condition effectively.
C2-C3 Vertebral Fusion Patterns
The fusion of the C2 and C3 vertebrae is one of the most frequently observed patterns in KFS patients. This specific fusion can lead to a reduction in neck mobility and may contribute to the characteristic short neck appearance associated with the syndrome. Early detection through imaging studies is essential for proper management.
C5-C6 Vertebral Fusion Characteristics
Another common site for vertebral fusion in KFS is between the C5 and C6 vertebrae. This fusion can result in altered biomechanics of the cervical spine, potentially leading to increased stress on adjacent vertebrae. Regular monitoring is necessary to prevent complications.
Multiple Level Fusions and Their Implications
Multiple level fusions, where more than two vertebrae are fused together, can lead to more severe symptoms and complications in KFS patients. These can include increased risk of spinal instability, neurological issues, and restricted mobility. A comprehensive treatment plan is vital for managing these complex cases.
| Location of Fusion | Common Symptoms | Potential Complications |
|---|---|---|
| C2-C3 | Reduced neck mobility, short neck appearance | Spinal instability, neurological issues |
| C5-C6 | Altered cervical biomechanics, stress on adjacent vertebrae | Increased risk of degenerative changes |
| Multiple Levels | Severe restriction of mobility, complex spinal deformities | Neurological complications, significant spinal instability |
Understanding the specific locations and patterns of fused vertebrae in KFS is crucial for developing effective treatment strategies. By identifying the most common fusion sites and their implications, healthcare providers can offer targeted care to improve patient outcomes.
Diagnostic Approaches for Identifying Fused Vertebrae
Diagnosing fused vertebrae requires a comprehensive approach that combines clinical examination techniques with advanced imaging studies. We use a variety of methods to accurately identify and assess the extent of vertebral fusion.
Clinical Examination Techniques
A thorough clinical examination is the first step in diagnosing fused vertebrae. We assess neck mobility, looking for limitations in range of motion that may indicate fusion. We also examine the patient’s posture and look for any visible signs of spinal deformity. Clinical evaluation helps us identify potential neurological deficits and assess the overall impact of fused vertebrae on the patient’s quality of life.
During the examination, we pay particular attention to the classic triad associated with Klippel-Feil Syndrome: short neck appearance, low posterior hairline, and limited neck mobility. While not all patients exhibit all three features, their presence can guide our diagnostic process.
Imaging Studies: X-rays, CT, and MRI
Imaging studies are crucial for confirming the diagnosis of fused vertebrae and assessing the extent of fusion. We typically begin with X-rays, which provide a preliminary view of the spine and can reveal obvious fusions or other bony abnormalities.
For more detailed imaging, we often use Computed Tomography (CT) scans. CT scans offer a clearer picture of the bony structures, allowing us to assess the extent of fusion and identify any associated anomalies.
Magnetic Resonance Imaging (MRI) is particularly valuable for evaluating the soft tissues surrounding the spine, including the spinal cord and nerve roots. MRI helps us identify any neurological complications associated with fused vertebrae.
Genetic Testing Options
In cases where Klippel-Feil Syndrome is suspected, we may recommend genetic testing. While there is no single “KFS gene,” mutations in certain genes, such as GDF6 and GDF3, have been associated with the condition. Genetic testing can help confirm the diagnosis and provide information about the risk of passing the condition to offspring.
We discuss the benefits and limitations of genetic testing with our patients, ensuring they are fully informed about the process and its potential outcomes.
Potential Complications of Klippel-Feil Syndrome
Patients with Klippel-Feil Syndrome (KFS) are at risk for various complications, making comprehensive care essential. KFS is a complex condition characterized by the congenital fusion of any two of the seven cervical vertebrae. This fusion can lead to a range of issues, from mild discomfort to severe neurological problems.
Neurological Complications
One of the most significant concerns for individuals with KFS is the risk of neurological complications. The abnormal fusion of vertebrae can lead to spinal cord compression, resulting in symptoms such as pain, numbness, and weakness in the limbs. In severe cases, this compression can cause more severe neurological deficits, including paralysis.
According to a study published in the European Spine Jvournal, patients with KFS are at an increased risk of neurological complications due to the instability of the cervical spine. This instability can lead to degenerative changes and potentially severe neurological consequences.
Spinal Instability Risks
Spinal instability is another significant risk associated with KFS. The fusion of vertebrae can alter the normal biomechanics of the spine, leading to increased stress on the surrounding vertebrae and discs. This stress can result in degenerative changes, such as disc degeneration and osteoarthritis, which can further exacerbate spinal instability.
As noted by experts, “The presence of KFS increases the risk of spinal instability, which can lead to a range of complications, including neurological deterioration.” Therefore, monitoring and managing spinal instability is crucial in the care of patients with KFS.
Associated Systemic Conditions
KFS is often associated with various systemic conditions, including renal and cardiac anomalies. Studies have shown that individuals with KFS are at a higher risk of having congenital anomalies in other systems, emphasizing the need for comprehensive evaluation and management.
A thorough assessment is necessary to identify any associated conditions early, allowing for timely intervention. As we understand more about KFS, it becomes clear that a multidisciplinary approach is essential in managing the condition and its complications.
Risk Factors for Requiring Surgical Intervention
Certain factors increase the likelihood of requiring surgical intervention in patients with Klippel-Feil Syndrome (KFS). Understanding these risk factors is crucial for effective management and treatment planning.
Gender-Related Risk Factors
Research has shown that gender can play a role in the likelihood of requiring surgical intervention for KFS patients. Studies indicate that females may be more likely to require surgery due to the nature of their spinal abnormalities. We will examine the specific gender-related risk factors in detail.
| Gender | Surgical Intervention Rate | Common Complications |
|---|---|---|
| Male | 35% | Spinal instability, neurological symptoms |
| Female | 45% | Neurological progression, chronic pain |
Degree of Spinal Instability
The degree of spinal instability is a significant risk factor for requiring surgical intervention in KFS patients. Patients with more pronounced spinal instability are at a higher risk of neurological complications. We assess the degree of instability through advanced imaging techniques.
Neurological Symptom Progression
The progression of neurological symptoms is another critical factor that may necessitate surgical intervention. Patients experiencing rapid progression of neurological symptoms are more likely to require surgery to prevent further deterioration.
Pain and Quality of Life Considerations
Pain management and quality of life are essential considerations when evaluating the need for surgical intervention. Surgical options are often considered when conservative management fails to alleviate pain and improve quality of life. We work closely with patients to understand their specific needs and develop a personalized treatment plan.
Treatment Options for Fused Vertebrae and KFS
The management of fused vertebrae and Klippel-Feil Syndrome (KFS) requires a multifaceted approach. We recognize that each patient’s condition is unique, and therefore, treatment plans are tailored to address specific needs and symptoms.
Conservative Management Approaches
For many patients with KFS, conservative management is the initial treatment strategy. This approach includes physical therapy to improve neck mobility and strength, as well as pain management techniques to address discomfort associated with the condition.
We also recommend regular monitoring to assess the progression of the condition and adjust the treatment plan as necessary.
Surgical Techniques and Considerations
In more severe cases of KFS, or when conservative management is insufficient, surgical intervention may be necessary. Surgical techniques can vary depending on the specific characteristics of the condition, such as the location and extent of vertebral fusion.
We consider factors such as the patient’s overall health, the presence of neurological symptoms, and the degree of spinal instability when determining the need for surgical intervention.
Rehabilitation Strategies
Following surgical treatment, or as part of conservative management, rehabilitation strategies play a crucial role in helping patients regain optimal function and manage symptoms. These strategies may include physical therapy, occupational therapy, and lifestyle modifications.
Our team works closely with patients to develop personalized rehabilitation plans that address their unique needs and goals.
Living with Klippel-Feil Syndrome: Daily Challenges and Adaptations
Living with KFS involves navigating a range of daily difficulties that can impact various aspects of life. Individuals with this condition often need to make significant adaptations to manage their symptoms effectively and maintain a good quality of life.
Physical Activity Modifications
One of the primary challenges for individuals with KFS is modifying their physical activities to accommodate their condition. High-impact exercises and contact sports are generally discouraged due to the risk of injury and exacerbating spinal instability. Instead, patients are often advised to engage in low-impact activities such as swimming or cycling, which can help maintain cardiovascular fitness without putting excessive strain on the neck.
It’s also important for individuals with KFS to consult with healthcare professionals to develop a personalized exercise plan that takes into account their specific condition and limitations.
Ergonomic Considerations
Ergonomic adjustments are crucial for individuals with KFS to reduce discomfort and prevent further complications. This includes using ergonomic furniture and equipment that supports proper posture and reduces strain on the neck and spine.
- Adjusting workstations to promote good posture
- Using supportive pillows and mattresses
- Avoiding heavy lifting or bending
Psychosocial Support Resources
Living with KFS can have a significant psychosocial impact, affecting an individual’s mental health and social interactions. Access to psychosocial support resources is vital for managing the emotional and psychological aspects of the condition.
Educational and Workplace Accommodations
Individuals with KFS may require specific accommodations in educational and workplace settings to ensure their comfort and productivity. This can include modifications to their workspace, flexible scheduling, and the provision of necessary assistive devices.
By understanding the daily challenges associated with KFS and implementing appropriate adaptations, individuals with this condition can lead fulfilling lives. It’s essential for patients, families, and healthcare providers to work together to develop comprehensive management plans that address the unique needs of each individual.
Conclusion: Advances in Understanding and Managing Fused Vertebrae
Advances in diagnosis and treatment have significantly improved the management of Klippel-Feil Syndrome (KFS). Ongoing research continues to enhance our understanding of fused vertebrae and KFS, leading to better patient outcomes. We have seen significant progress in fused vertebrae understanding, allowing for more effective managing of fused vertebrae.
The complexity of KFS requires a comprehensive approach to care, incorporating advances in KFS management. By combining clinical expertise with cutting-edge technology, we can provide personalized treatment plans that address the unique needs of each patient. This integrated approach enables us to improve the quality of life for individuals living with KFS.
As we continue to advance our understanding of KFS, we remain committed to providing world-class healthcare with complete support for international patients. Our goal is to empower patients with the knowledge and resources they need to navigate their condition, ensuring they receive the best possible care.
FAQ
What is Klippel-Feil syndrome?
Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of two or more cervical vertebrae, which can lead to limited neck mobility and other associated complications.
What causes fused vertebrae in the neck?
Fused vertebrae in the neck are often caused by congenital factors related to embryonic development, with genetic factors playing a significant role in the development of Klippel-Feil syndrome.
What are the classic symptoms of Klippel-Feil syndrome?
The classic triad of KFS includes a short neck appearance, low posterior hairline, and limited neck mobility, which are key clinical features used in diagnosis.
How common is Klippel-Feil syndrome?
Recent studies suggest that KFS may be more prevalent than previously thought, with estimates as high as 1 in 172 births, although historical estimates ranged from 1 in 40,000 to 1 in 50,000.
What are the potential complications of Klippel-Feil syndrome?
Potential complications of KFS include neurological complications, risks of spinal instability, and associated systemic conditions, which can significantly impact the quality of life for individuals with the condition.
How is Klippel-Feil syndrome diagnosed?
Diagnosis of KFS involves clinical examination techniques, imaging studies such as X-rays, CT, and MRI, and genetic testing options to identify the presence and extent of vertebral fusion.
What are the treatment options for fused vertebrae and KFS?
Treatment options for fused vertebrae and KFS include conservative management approaches, surgical techniques, and rehabilitation strategies, which are tailored to the individual’s specific needs and the severity of their condition.
When is surgical intervention necessary for KFS patients?
Surgical intervention is considered necessary for KFS patients when there are significant risk factors such as gender-related factors, degree of spinal instability, and progression of neurological symptoms.
How can individuals with KFS adapt to daily challenges?
Individuals with KFS can adapt to daily challenges by making physical activity modifications, considering ergonomic adjustments, and accessing psychosocial support resources to manage their condition effectively.
What is the prognosis for individuals with Klippel-Feil syndrome?
The prognosis for individuals with KFS varies depending on the severity of their condition and the presence of associated complications, but with proper management and care, many individuals can lead active and fulfilling lives.
What is Klippel-Feil syndrome?
Klippel-Feil syndrome (KFS) is a rare congenital disorder characterized by the fusion of two or more cervical vertebrae, which can lead to limited neck mobility and other associated complications.
What causes fused vertebrae in the neck?
Fused vertebrae in the neck are often caused by congenital factors related to embryonic development, with genetic factors playing a significant role in the development of Klippel-Feil syndrome.
What are the classic symptoms of Klippel-Feil syndrome?
The classic triad of KFS includes a short neck appearance, low posterior hairline, and limited neck mobility, which are key clinical features used in diagnosis.
How common is Klippel-Feil syndrome?
Recent studies suggest that KFS may be more prevalent than previously thought, with estimates as high as 1 in 172 births, although historical estimates ranged from 1 in 40,000 to 1 in 50,000.
What are the potential complications of Klippel-Feil syndrome?
Potential complications of KFS include neurological complications, risks of spinal instability, and associated systemic conditions, which can significantly impact the quality of life for individuals with the condition.
How is Klippel-Feil syndrome diagnosed?
Diagnosis of KFS involves clinical examination techniques, imaging studies such as X-rays, CT, and MRI, and genetic testing options to identify the presence and extent of vertebral fusion.
What are the treatment options for fused vertebrae and KFS?
Treatment options for fused vertebrae and KFS include conservative management approaches, surgical techniques, and rehabilitation strategies, which are tailored to the individual’s specific needs and the severity of their condition.
When is surgical intervention necessary for KFS patients?
Surgical intervention is considered necessary for KFS patients when there are significant risk factors such as gender-related factors, degree of spinal instability, and progression of neurological symptoms.
How can individuals with KFS adapt to daily challenges?
Individuals with KFS can adapt to daily challenges by making physical activity modifications, considering ergonomic adjustments, and accessing psychosocial support resources to manage their condition effectively.
What is the prognosis for individuals with Klippel-Feil syndrome?
The prognosis for individuals with KFS varies depending on the severity of their condition and the presence of associated complications, but with proper management and care, many individuals can lead active and fulfilling lives.